Make Your Coffee Heart-Healthier!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Health-Hack Your Coffee
We have previously written about the general health considerations (benefits and potential problems) of coffee:
The Bitter Truth About Coffee (or is it?)
Today, we will broadly assume that you are drinking coffee (in general, not necessarily right now, though if you are, same!) and would like to continue to do so. We also assume you’d like to do so as healthily as possible.
Not all coffees are created equal
If you order a coffee in France or Italy without specifying what kind, the coffee you receive will be short, dark, and handsome and without sugar. Healthwise, this is not a bad starting point. However…
- It will usually be espresso
- Or it may be what in N. America is called a French press (in Europe it’s just called a cafetière)
Both of these kinds of coffee mean that cafestol, a compound found in the oily part of coffee and which is known to raise LDL (“bad” cholesterol”), stays in the drink.
Read: Cafestol and Kahweol: A Review on Their Bioactivities and Pharmacological Properties
Also: Cafestol extraction yield from different coffee brew mechanisms
If you’re reading that second one and wondering what a mocha pot or a Turkish coffee is, they are these things:
- Mocha pot: a stovetop device used for making espresso without an espresso machine
- Turkish coffee pot: also a stovetop device; this thing makes some of the strongest coffee you have ever encountered. Turks usually add sugar (this writer doesn’t; but my taste in coffee been described as “coffee like a punch in the face”)
So, wonderful as they are for those of us who love strong coffee, they also produce the highest in-drink levels of cafestol. If you’d like to cut the cafestol (for example, if you are keeping an eye on your LDL), we recommend…
The humble filter coffee
Whether by your favorite filter coffee machine or a pour-over low-tech coffee setup of the kind you could use even without an electricity supply, the filter keeps more than just the coffee grinds out; it keeps the cafestol out too; most of it, anyway, depending on what kind of filter you use, and the grind of the coffee:
Physical characteristics of the paper filter and low cafestol content filter coffee brews
What about instant coffee?
It has very little cafestol in it. It’s up to you whether that’s sufficient reason to choose it over any other form of coffee (this coffee-lover could never)
Want to make any coffee healthier?
This one isn’t about the cafestol, but…
If you take l-theanine (see here for our previous main feature about l-theanine), the l-theanine acts as a moderator and modulator of the caffeine, amongst other benefits:
The Cognitive-Enhancing Outcomes of Caffeine and L-theanine: A Systematic Review
As to where to get that, we don’t sell it, but here’s an example product on Amazon
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Can You Gain Muscle & Lose Fat At The Same Time?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝Is it possible to lose fat and gain muscle at the same time, or do we need to focus on one and then the other, and if so, which order is best?❞
Contrary to popular belief, you can do both simultaneously! However, it’s not as easy as doing just one or the other, which is why most bodybuilders, for example, have a “building phase” and a “cutting phase”.
The reason it’s difficult is because of the diet. Growing muscle doesn’t just take protein and micronutrients; it takes energy as well, which must come from carbohydrates and/or fats. Therefore, it is tricky to eat enough to build muscle and to fuel the workouts that are required to build the muscle (you can’t hit the gym in a state of rabbit starvation* and expect to perform well at your workout), while at the same time not eating enough carbs/fats to have any excess to store as fat.
*So-called because rabbit-meat is very lean, such that when during times of famine, European peasants tried to subsist off mostly rabbits, their health quickly plummeted for lack of energy. It’s also been called “salmon starvation”, apparently, for the same reason:
In French it’s called “Mal de caribou” (caribou sickness), by the way. But you get the idea: eat too much lean protein without enough carbs/fats, and woe shall befall.
So, if you want to do both at once, you need to be incredibly on top of your macros, and the bad news is, only you (or a coach working directly with you) can work out what precise macros requirements your body has, because it depends on your body and your activities.
The easier “half-way house”
We will get to the “building phase” and “cutting phase” of bodybuilders, but first, here’s an option that’s very worthy of consideration, and it is: forget about your weight and just focus on health while incidentally doing regular resistance exercises and HIIT.
What will happen if you do this (assuming a healthy balanced diet, nothing special and without counting anything, but we’re talking at least mostly whole-foods, and at least mostly plants; the Mediterranean diet is great for this, as it is for most things) is:
- The dietary approach described will gradually improve your metabolic health if it wasn’t already good. If it was already good, it’ll likely just maintain it, rather than improve it.
- The resistance exercises will, if engaged with seriously (it has to be difficult to do, or your muscles won’t have any reason to grow), gradually build muscle. This will be very gradual, because you’re not eating for bodybuilding, nor optimizing your general lifestyle for same. Historically many women have feared lifting weights because they don’t want to “look like a weightlifter”, but the kinds of bodies that word brings to mind are not the kind that happen by accident (especially for women, with our different hormones guiding our bodies to a different composition); it takes a lot of single-minded dedication to specifically optimize size gains, for a long time.
- The high-intensity interval training (HIIT) will more rapidly improve your metabolic health, and unlike most forms of exercise, it will actually result in a gradual reduction of fat, if you have superfluous fat to lose. This is because whereas most forms of cardio exercise increase the heartrate for a while but then have a corresponding metabolic slump afterwards to make up for it, HIIT confuses the heart (in a good way) which results in it having to grow stronger, and not doing any compensatory metabolic slump:
How To Do HIIT (Without Wrecking Your Body) ← as well as the “how to”, this also gives some of the science behind it, too
This will, thus, result in gradual gain of muscle and loss of fat—or if you take it easier with the exercise, then you can easily settle into just maintaining your body composition as it is, but that wasn’t the question today.
So, there you have it, that’s how to do both at once! Now, if you want more dramatic results, then more dramatic methods are called for:
What bodybuilders (mostly) do
Matters of genetic predisposition and commonplace use of steroids aside, here’s how bodybuilders get that “lots of muscle, no fat” figure:
- First, get into “moderate” shape if not already there.
- Bulk up: eat amounts of food that will seem unreasonable to a non-bodybuilder; eating 2x or even 3x the “recommended” daily calorie amount is common; focus is typically on getting adequate (for bodybuilding purposes) protein while also carb-loading for workouts and getting at least enough fats for fat-soluble vitamins to work. In the gym, focus on doing sets of very few reps with the heaviest weights one can safely lift, while doing minimal cardio, and also sleeping a lot (9–12hrs per day), which is essential because this is putting a huge strain on the body and it needs a chance to recover and rebuild.
- Cut down: maintain protein intake (to at least mostly maintain muscles) while keeping carbs and fats low, doing cardio work (HIIT is still ideal) and running a calorie deficit for a short while (there is no use in trying to maintain a long-term calorie deficit; your body will try to save you from starvation by storing any fat it can and slowing your metabolism).
Phases 2 and 3 are then cycled, alternating every month, or every 6 weeks, or every 2 months or so, depending on personal preferences and scheduling considerations (bodybuilders will often have competitions they are working towards, so they need to time things to be at the end of a cutting phase to look their “best” by bodybuilder standards).
Disclaimer: bodybuilding is complex, and can be ruinous to the health if practised inexpertly, because of its extreme nature. We don’t recommend serious bodybuilding per se in general, but if you are going to do it, please consult with a professional bodybuilding coach, and do not rely on a few paragraphs from us that are intended only to give the most basic overview of how bodybuilders can approach the “gain muscle, lose fat” problem.
Want to know more?
We’ve written on some related topics previously; here’s a three-part series:
- How To Lose Weight (Healthily!)
- How To Build Muscle (Healthily!)
- How To Gain Weight (Healthily!) ← this one’s specifically about gaining healthy levels of fat, for any who want/need that
And also:
Can We Do Fat Redistribution? ← yes we can, but there are caveats
Take care!
Share This Post
-
Why Do We Have Crooked Teeth When Our Ancestors Didn’t?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Evidence shows that people in ancient times typically had straight teeth set well into strong jaws, with even wisdom teeth fitting properly.
So, what went wrong? Did evolution do us a disservice?
Some information to chew on
Transition from hard-to-chew diets to processed, refined foods over millennia has reduced jaw size while tooth size stayed constant. Smaller jaws lead to tooth crowding, crookedness, and impacted wisdom teeth, requiring braces or extractions in modern times.
However, all is not lost!
Studies on non-human animals show softer diets reduce jaw and facial growth, causing dental crowding. In other words: dental crowding is primarily attributed to dietary and lifestyle changes, though genetics may play a role.
And notably, when it comes to humans, populations with less processed diets experience fewer dental problems, suggesting lifestyle modifications could help prevent tooth crowding.
And no, it is not too late. Remember, you are rebuilding your body all the time, including your bones!
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
The Exercises That Can Fix Sinus Problems (And More) ← this also improves the jaw structure
Take care!
Share This Post
-
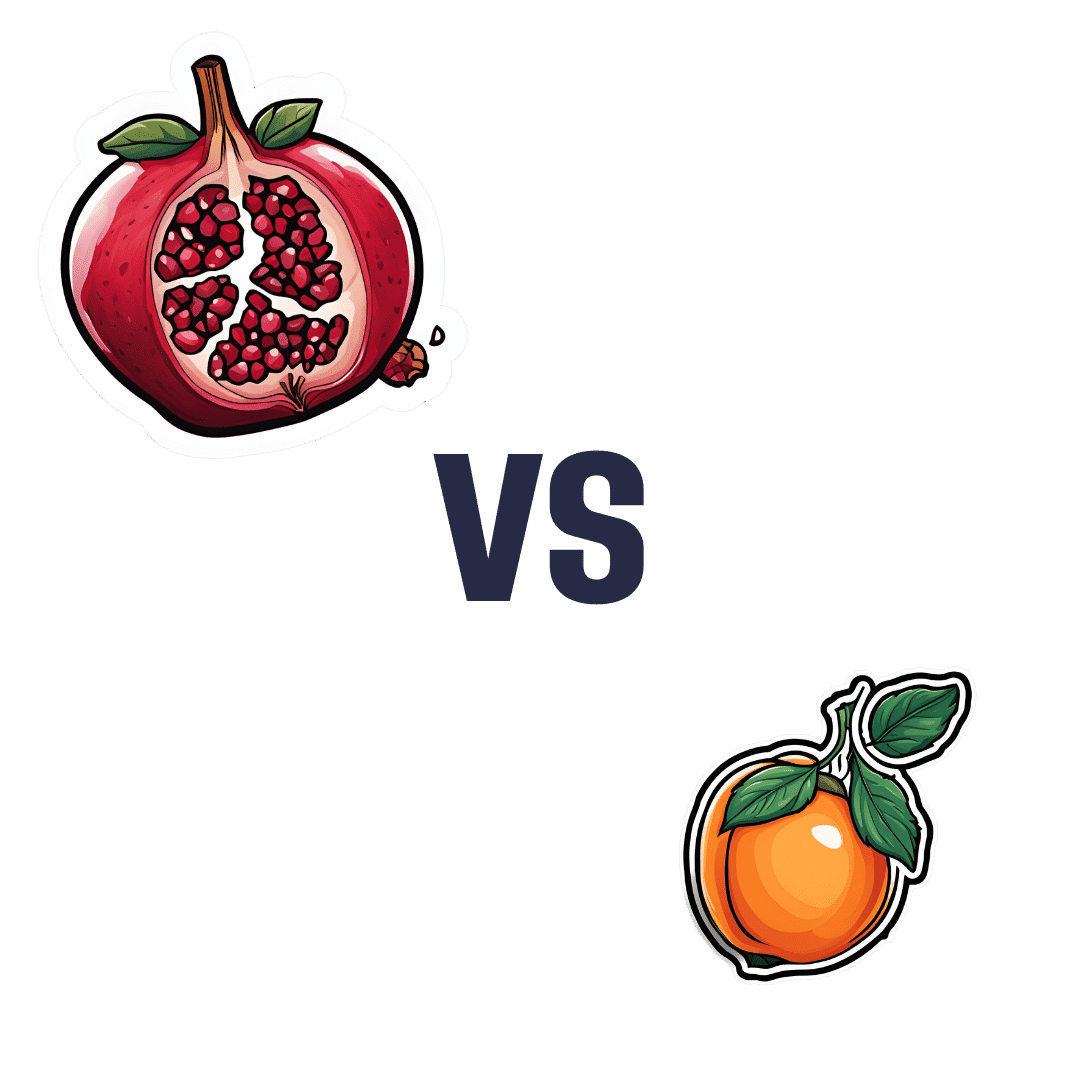
Pomegranate vs Apricot – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pomegranate to apricot, we picked the pomegranate.
Why?
Both are great! Top tier fruits. But ultimately, pomegranate does have more to offer:
In terms of macros, pomegranate has more protein, carbs, and fiber (and even a little healthy fat—it’s the seeds); the main deciding factor on macros for fruits is almost always the fiber, and that’s the case here, which is why we hand the win to pomegranates in this category.
In the category of vitamins, pomegranates have more of vitamins B1, B2, b5, B6, B7, B9, K, and choline, while apricots have more of vitamins A, B3, and E. A clear win for pomegranates here.
When it comes to minerals, pomegranate has more copper, calcium, magnesium, manganese, phosphorus, selenium, and zinc, while apricots boast just a little more calcium and iron. Another easy win for pomegranates.
Looking at polyphenols, apricots finally win a category, with greater overall polyphenol coverage.
Which is good, but not enough to overcome the other three categories all being in pomegranates’ favor—hence the overall win for pomegranates here!
Of course, the solution is to enjoy both! Diversity is good, for exactly such reasons as this.
Want to learn more?
You might like to read:
Pomegranate’s Health Gifts Are Mostly In Its Peel ← in other words, the one part of the fruit you don’t normally eat. However! It can be dried and ground into a powder supplement, or else made in pomegranate tea.
Enjoy!
Share This Post
Related Posts
-
Why are tall people more likely to get cancer? What we know, don’t know and suspect
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
People who are taller are at greater risk of developing cancer. The World Cancer Research Fund reports there is strong evidence taller people have a higher chance of of developing cancer of the:
- pancreas
- large bowel
- uterus (endometrium)
- ovary
- prostate
- kidney
- skin (melanoma) and
- breast (pre- and post-menopausal).
But why? Here’s what we know, don’t know and suspect.
Pexels/Andrea Piacquadio Height does increase your cancer risk – but only by a very small amount. Christian Vinces/Shutterstock A well established pattern
The UK Million Women Study found that for 15 of the 17 cancers they investigated, the taller you are the more likely you are to have them.
It found that overall, each ten-centimetre increase in height increased the risk of developing a cancer by about 16%. A similar increase has been found in men.
Let’s put that in perspective. If about 45 in every 10,000 women of average height (about 165 centimetres) develop cancer each year, then about 52 in each 10,000 women who are 175 centimetres tall would get cancer. That’s only an extra seven cancers.
So, it’s actually a pretty small increase in risk.
Another study found 22 of 23 cancers occurred more commonly in taller than in shorter people.
Why?
The relationship between height and cancer risk occurs across ethnicities and income levels, as well as in studies that have looked at genes that predict height.
These results suggest there is a biological reason for the link between cancer and height.
While it is not completely clear why, there are a couple of strong theories.
The first is linked to the fact a taller person will have more cells. For example, a tall person probably has a longer large bowel with more cells and thus more entries in the large bowel cancer lottery than a shorter person.
Scientists think cancer develops through an accumulation of damage to genes that can occur in a cell when it divides to create new cells.
The more times a cell divides, the more likely it is that genetic damage will occur and be passed onto the new cells.
The more damage that accumulates, the more likely it is that a cancer will develop.
A person with more cells in their body will have more cell divisions and thus potentially more chance that a cancer will develop in one of them.
Some research supports the idea having more cells is the reason tall people develop cancer more and may explain to some extent why men are more likely to get cancer than women (because they are, on average, taller than women).
However, it’s not clear height is related to the size of all organs (for example, do taller women have bigger breasts or bigger ovaries?).
One study tried to assess this. It found that while organ mass explained the height-cancer relationship in eight of 15 cancers assessed, there were seven others where organ mass did not explain the relationship with height.
It is worth noting this study was quite limited by the amount of data they had on organ mass.
Is it because tall people have more cells? Halfpoint/Shutterstock Another theory is that there is a common factor that makes people taller as well as increasing their cancer risk.
One possibility is a hormone called insulin-like growth factor 1 (IGF-1). This hormone helps children grow and then continues to have an important role in driving cell growth and cell division in adults.
This is an important function. Our bodies need to produce new cells when old ones are damaged or get old. Think of all the skin cells that come off when you use a good body scrub. Those cells need to be replaced so our skin doesn’t wear out.
However, we can get too much of a good thing. Some studies have found people who have higher IGF-1 levels than average have a higher risk of developing breast or prostate cancer.
But again, this has not been a consistent finding for all cancer types.
It is likely that both explanations (more cells and more IGF-1) play a role.
But more research is needed to really understand why taller people get cancer and whether this information could be used to prevent or even treat cancers.
I’m tall. What should I do?
If you are more LeBron James than Lionel Messi when it comes to height, what can you do?
Firstly, remember height only increases cancer risk by a very small amount.
Secondly, there are many things all of us can do to reduce our cancer risk, and those things have a much, much greater effect on cancer risk than height.
We can take a look at our lifestyle. Try to:
- eat a healthy diet
- exercise regularly
- maintain a healthy weight
- be careful in the sun
- limit alcohol consumption.
And, most importantly, don’t smoke!
If we all did these things we could vastly reduce the amount of cancer.
You can also take part in cancer screening programs that help pick up cancers of the breast, cervix and bowel early so they can be treated successfully.
Finally, take heart! Research also tells us that being taller might just reduce your chance of having a heart attack or stroke.
Susan Jordan, Associate Professor of Epidemiology, The University of Queensland and Karen Tuesley, Postdoctoral Research Fellow, School of Public Health, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
STI rates are increasing among midlife and older adults. We need to talk about it
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Globally, the rates of common sexually transmissible infections (STIs) are increasing among people aged over 50. In some cases, rates are rising faster than among younger people.
Recent data from the United States Centers for Disease Control and Prevention shows that, among people aged 55 and older, rates of gonorrhoea and chlamydia, two of the most common STIs, more than doubled between 2012 and 2022.
Australian STI surveillance data has reflected similar trends. Between 2013 and 2022, there was a steady increase in diagnoses of chlamydia, gonorrhoea and syphilis among people aged 40 and older. For example, there were 5,883 notifications of chlamydia in Australians 40 plus in 2013, compared with 10,263 in 2022.
A 2020 study of Australian women also showed that, between 2000 and 2018, there was a sharper increase in STI diagnoses among women aged 55–74 than among younger women.
While the overall rate of common STIs is highest among young adults, the significant increase in STI diagnoses among midlife and older adults suggests we need to pay more attention to sexual health across the life course.
Fit Ztudio/Shutterstock Why are STI rates rising among older adults?
STI rates are increasing globally for all age groups, and an increase among midlife and older people is in line with this trend.
However, increases of STIs among older people are likely due to a combination of changing sex and relationship practices and hidden sexual health needs among this group.
The “boomer” generation came of age in the 60s and 70s. They are the generation of free love and their attitude to sex, even as they age, is quite different to that of generations before them.
Given the median age of divorce in Australia is now over 43, and the internet has ushered in new opportunities for post-separation dating, it’s not surprising that midlife and older adults are exploring new sexual practices or finding multiple sexual partners.
People may start new relationships later in life. Tint Media/Shutterstock It’s also possible midlife and older people have not had exposure to sexual health education in school or do not relate to current safe sex messages, which tend to be directed toward young people. Condoms may therefore seem unnecessary for people who aren’t trying to avoid pregnancy. Older people may also lack confidence negotiating safe sex or accessing STI screening.
Hidden sexual health needs
In contemporary life, the sex lives of older adults are largely invisible. Ageing and older bodies are often associated with loss of power and desirability, reflected in the stereotype of older people as asexual and in derogatory jokes about older people having sex.
With some exceptions, we see few positive representations of older sexual bodies in film or television.
Older people’s sexuality is also largely invisible in public policy. In a review of Australian policy relating to sexual and reproductive health, researchers found midlife and older adults were rarely mentioned.
Sexual health policy generally targets groups with the highest STI rates, which excludes most older people. As midlife and older adults are beyond childbearing years, they also do not feature in reproductive health policy. This means there is a general absence of any policy related to sex or sexual health among midlife or older adults.
Added to this, sexual health policy tends to be focused on risk rather than sexual wellbeing. Sexual wellbeing, including freedom and capacity to pursue pleasurable sexual experiences, is strongly associated with overall health and quality of life for adults of all ages. Including sexual wellbeing as a policy priority would enable a focus on safe and respectful sex and relationships across the adult life course.
Without this priority, we have limited knowledge about what supports sexual wellbeing as people age and limited funding for initiatives to engage with midlife or older adults on these issues.
Midlife and older adults may have limited knowledge about STIs. Southworks/Shutterstock How can we support sexual health and wellbeing for older adults?
Most STIs are easily treatable. Serious complications can occur, however, when STIs are undiagnosed and untreated over a long period. Untreated STIs can also be passed on to others.
Late diagnosis is not uncommon as some STIs can have no symptoms and many people don’t routinely screen for STIs. Older, heterosexual adults are, in general, less likely than other groups to seek regular STI screening.
For midlife or older adults, STIs may also be diagnosed late because some doctors do not initiate testing due to concerns they will cause offence or because they assume STI risk among older people is negligible.
Many doctors are reluctant to discuss sexual health with their older patients unless the patient explicitly raises the topic. However, older people can be embarrassed or feel awkward raising matters of sex.
Resources for health-care providers and patients to facilitate conversations about sexual health and STI screening with older patients would be a good first step.
To address rising rates of STIs among midlife and older adults, we also need to ensure sexual health promotion is targeted toward these age groups and improve accessibility of clinical services.
More broadly, it’s important to consider ways to ensure sexual wellbeing is prioritised in policy and practice related to midlife and older adulthood.
A comprehensive approach to older people’s sexual health, that explicitly places value on the significance of sex and intimacy in people’s lives, will enhance our ability to more effectively respond to sexual health and STI prevention across the life course.
Jennifer Power, Associate Professor and Principal Research Fellow, Australian Research Centre in Sex, Health and Society, La Trobe University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Calculate (And Enjoy) The Perfect Night’s Sleep
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is Dr. Michael Breus, a clinical psychologist and sleep specialist, and he wants you to get a good night’s sleep, every night.
First, let’s assume you know a lot of good advice about how to do that already in terms of environment and preparation, etc. If you want a recap before proceeding, then we recommend:
Get Better Sleep: Beyond The Basics
Now, what does he want to add?
Wake up refreshed
Of course, how obtainable this is will depend on the previous night’s sleep, but there is something important we can do here regardless, and it’s: beat sleep inertia.
Sleep inertia is what happens when we wake up groggy (for reasons other than being ill, drugged, etc) rather than refreshed. It’s not actually related to how much sleep we have, though!
Rather, it pertains to whether we woke up during a sleep cycle, or between cycles:
- If we wake up between sleep cycles, we’ll avoid sleep inertia.
- If we wake up during a sleep cycle, we’ll be groggy.
Deep sleep generally occurs in 90-minute blocks, albeit secretly that is generally 3× 20 minute blocks in a trenchcoat, with transition periods between, during which the brainwaves change frequency.
REM sleep generally occurs in 20 minute blocks, and will usually arrive in series towards the end of our natural sleep period, to fit neatly into the last 90-minute cycle.
Sometimes these will appear a little out of order, because we are complicated organic beings, but those are the general trends.
In any case, the take-away here is: interrupt them at your peril. You need to wake up between cycles. There are two ways you can do this:
- Carefully calculate everything, and set a very precise alarm clock (this will work so long as you are correct in guessing how long it will take you to fall asleep)
- Use a “sunrise” lamp alarm clock, that in the hour approaching your set alarm time, will gradually increase the light. Because the body will not naturally wake up during a cycle unless a threat is perceived (loud noise, physical rousing, etc), the sunrise lamp method means that you will wake up between sleep cycles at some point during that hour (towards the beginning or end, depending on what your sleep balance/debt is like).
Do not sleep in (even if you have a sleep debt); it will throw everything out.
Caffeine will not help much in the morning
Assuming you got a reasonable night’s sleep, your brain has been cleansed of adenosine (a sleepy chemical), and if you are suffering from sleep inertia, the grogginess is due to melatonin (a different sleepy chemical).
Caffeine is an adenosine receptor blocker, so that will do nothing to mitigate the effects of melatonin in your brain that doesn’t have any meaningful quantity of adenosine in it in the morning.
Adenosine gradually accumulates in the brain over the course of the day (and then gets washed out while we sleep), so if you’re sleepy in the afternoon (for reasons other than: you just had a nap and now have sleep inertia again), then caffeine can block that adenosine in the afternoon.
Of course, caffeine is also a stimulant (it increases adrenaline levels and promotes vasoconstriction), but its effects at healthily small doses are modest for most people, and you’d do better by splashing cold water on your face and/or listening to some upbeat music.
Learn more: The Two Sides Of Caffeine
Time your naps correctly (if you take naps)
Dr. Breus has a lot to say about this, based on a lot of clinical research, but as it’s entirely consistent with what we’ve written before (based on the exact same research), to save space we’ll link to that here:
How To Be An Expert Nap-Artist (With No “Sleep-Hangovers”)
Calculate your bedtime correctly
Remember what we said about sleep cycles? This means that that famous “7–9 hours sleep” is actually “either 7½ or 9 hours sleep”—because those are multiples of 90 minutes, whereas 8 hours (for example) is not.
So, consider the time you want to get up (ideally, this should be relatively early, and the same time every day), and then count backwards either 7½ or 9 hours sleep (you choose), add 20–30 minutes to fall asleep, and that’s your bedtime.
So for example: if you want to have 7½ hours sleep and get up at 6am, then your bedtime is anywhere between 10pm and 10:10pm.
Remember how we said not to sleep in, even if you have a sleep debt? Now is the time to pay it off, if you have one. If you normally sleep 7½ hours, then make tonight a 9-hour sleep (plus 20–30 minutes to fall asleep). This means you’ll still get up at 6am, but your bedtime is now anywhere between 8:30pm and 8:40pm.
Want to know more from Dr. Breus?
You might like this excellent book of his that we reviewed a while back:
The Power of When – by Dr. Michael Breus
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: