Hate salad or veggies? Just keep eating them. Here’s how our tastebuds adapt to what we eat
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Do you hate salad? It’s OK if you do, there are plenty of foods in the world, and lots of different ways to prepare them.
But given almost all of us don’t eat enough vegetables, even though most of us (81%) know eating more vegetables is a simple way to improve our health, you might want to try.
If this idea makes you miserable, fear not, with time and a little effort you can make friends with salad.
Why don’t I like salads?
It’s an unfortunate quirk of evolution that vegetables are so good for us but they aren’t all immediately tasty to all of us. We have evolved to enjoy the sweet or umami (savoury) taste of higher energy foods, because starvation is a more immediate risk than long-term health.
Vegetables aren’t particularly high energy but they are jam-packed with dietary fibre, vitamins and minerals, and health-promoting compounds called bioactives.
Those bioactives are part of the reason vegetables taste bitter. Plant bioactives, also called phytonutrients, are made by plants to protect themselves against environmental stress and predators. The very things that make plant foods bitter, are the things that make them good for us.
Unfortunately, bitter taste evolved to protect us from poisons, and possibly from over-eating one single plant food. So in a way, plant foods can taste like poison.
For some of us, this bitter sensing is particularly acute, and for others it isn’t so bad. This is partly due to our genes. Humans have at least 25 different receptors that detect bitterness, and we each have our own genetic combinations. So some people really, really taste some bitter compounds while others can barely detect them.
This means we don’t all have the same starting point when it comes to interacting with salads and veggies. So be patient with yourself. But the steps toward learning to like salads and veggies are the same regardless of your starting point.
It takes time
We can train our tastes because our genes and our receptors aren’t the end of the story. Repeat exposures to bitter foods can help us adapt over time. Repeat exposures help our brain learn that bitter vegetables aren’t posions.
And as we change what we eat, the enzymes and other proteins in our saliva change too. This changes how different compounds in food are broken down and detected by our taste buds. How exactly this works isn’t clear, but it’s similar to other behavioural cognitive training.
Add masking ingredients
The good news is we can use lots of great strategies to mask the bitterness of vegetables, and this positively reinforces our taste training.
Salt and fat can reduce the perception of bitterness, so adding seasoning and dressing can help make salads taste better instantly. You are probably thinking, “but don’t we need to reduce our salt and fat intake?” – yes, but you will get more nutritional bang-for-buck by reducing those in discretionary foods like cakes, biscuits, chips and desserts, not by trying to avoid them with your vegetables.
Adding heat with chillies or pepper can also help by acting as a decoy to the bitterness. Adding fruits to salads adds sweetness and juiciness, this can help improve the overall flavour and texture balance, increasing enjoyment.
Pairing foods you are learning to like with foods you already like can also help.
The options for salads are almost endless, if you don’t like the standard garden salad you were raised on, that’s OK, keep experimenting.
Experimenting with texture (for example chopping vegetables smaller or chunkier) can also help in finding your salad loves.
Challenge your biases
Challenging your biases can also help the salad situation. A phenomenon called the “unhealthy-tasty intuition” makes us assume tasty foods aren’t good for us, and that healthy foods will taste bad. Shaking that assumption off can help you enjoy your vegetables more.
When researchers labelled vegetables with taste-focused labels, priming subjects for an enjoyable taste, they were more likely to enjoy them compared to when they were told how healthy they were.
The bottom line
Vegetables are good for us, but we need to be patient and kind with ourselves when we start trying to eat more.
Try working with biology and brain, and not against them.
And hold back from judging yourself or other people if they don’t like the salads you do. We are all on a different point of our taste-training journey.
Emma Beckett, Senior Lecturer (Food Science and Human Nutrition), School of Environmental and Life Sciences, University of Newcastle
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why We’re Called “10almonds”, And Other Questions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Avid coffee drinker so very interested in the results Also question Is there something that you could take or eat that would prevent the caffeine from stimulating the kidneys? I tried to drink decaf from morning to night not a good result! Thanks❞
That is a good question! The simple answer is “no” (but keep reading, because all is not lost)
There’s no way (that we yet know of) to proof the kidneys against the stimulating effect of caffeine. This is especially relevant because part of caffeine’s stimulating effect is noradrenergic, and that “ren” in the middle there? It’s about the kidneys. This is just because the adrenal gland is situated next to them (actually, it’s pretty much sitting on top of them), hence the name, but it does mean that the kidneys are about the hardest thing in the body to have not affected by caffeine.
However! The effects of caffeine in general can be softened a little with l-theanine (found in tea, or it can be taken as a supplement). It doesn’t stop it from working, but it makes the curve of the effect a little gentler, and so it can reduce some unwanted side effects.
You can read more about l-theanine here:
❝How to jump start a inactive metabolism and keep it going? THANKYOU❞
The good news is, if you’re alive, your metabolism is active (it never stops!). So, it may just need perking up a little.
As for keeping it going, well, that’s what we’re here for! We’re all in favor of healthy longevity.
We’ll do a main feature soon on what we can do to influence our metabolism in either direction, but to give some quick notes here:
- A lot of our metabolism is influenced by genes and is unalterable (without modifying our genes, anyway)
- Metabolism isn’t just one thing—it’s many. And sometimes, parts of our metabolism can be much quicker or slower than others.
- When people talk about wanting a “faster metabolism”, they’re usually referring to fat-burning, and that’s just a small part of the picture, but we understand that it’s a focal point for many.
There really is enough material for a whole main feature on metabolic tweaks, though, so watch this space!
❝Why the name “10 Almonds?” Is this recommended by the Doctor? A daily dosage? And, if so, why? Thanks! Please answer me…I truly want to know!❞
Almonds are very nutritionally dense, and for example 20g of almonds (so, about 20 almonds) would give a 100% daily dose of zinc, amongst other nutrients.
We also do like to think that we give our readers an easily digestible dose of condensed “nutrition” in the form of health information.
However! That’s not actually the reason at all. It’s a reference to a viral Facebook hoax! There was a post going around that claimed:
❝HEADACHE REMEDY. Eat 10–12 almonds, the equivalent of two aspirins, next time you have a headache❞ ← not true!
It made us think about how much health-related disinformation there was circulating online! So, calling ourselves 10almonds was a bit of a nod to that story, but also a reminder to ourselves:
We must always publish information with good scientific evidence behind it!
Share This Post
-
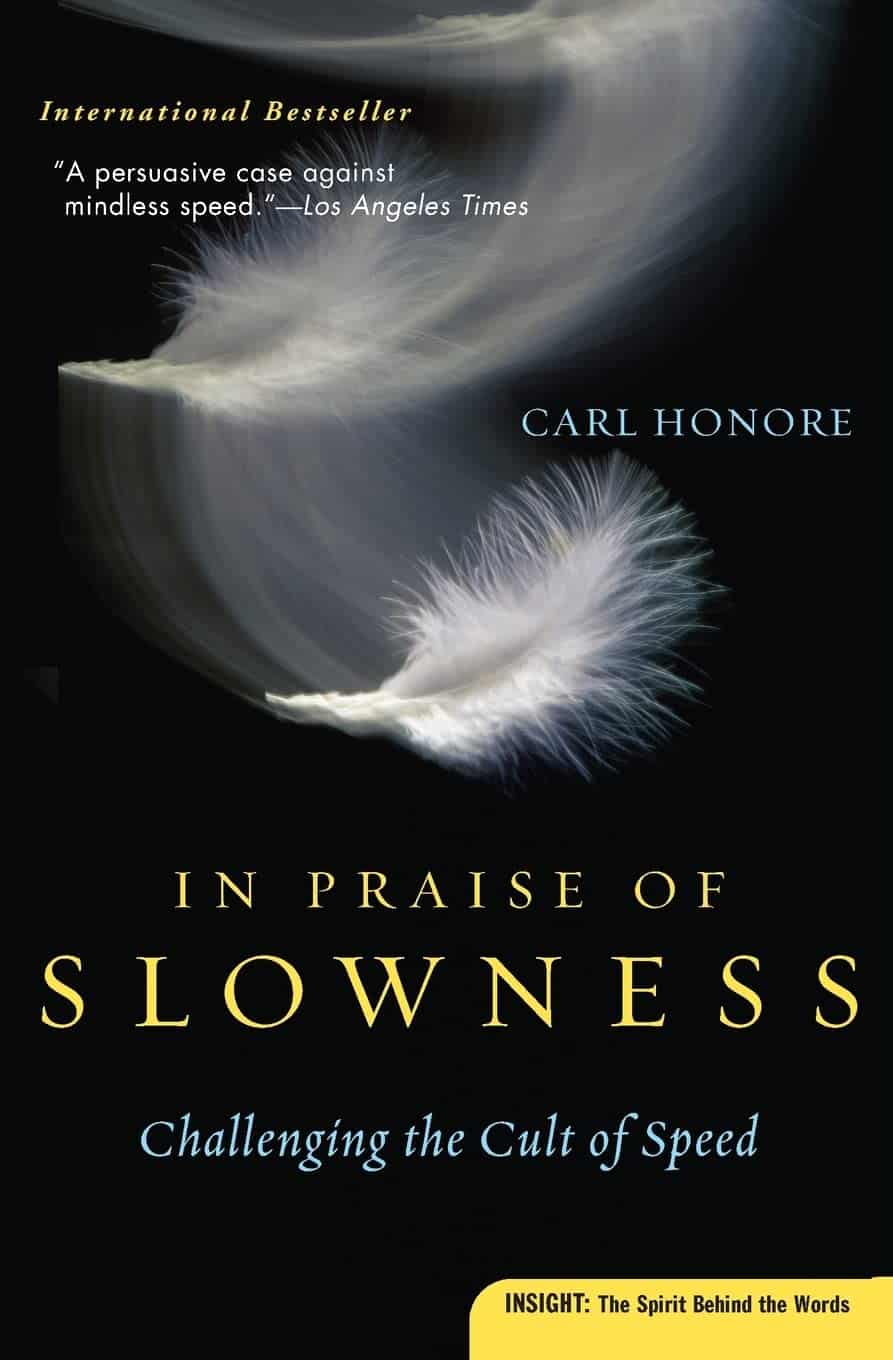
In Praise of Slowness – by Carl Honoré
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This isn’t just about “taking the time to smell the roses” although yes, that too. Rather, it’s mostly about looking at what drives us to speed everything up in the first place, and correcting where appropriate.
If your ancestors had time to eat fruit and lie in the sun, then why, with all of modern technology now available, are you harangued 16+ hours a day by the pressures of universally synchronized timepieces?
Honoré places a lot of the blame squarely on the industrial revolution; whereas previously our work would be limited by craftsmen who take a year to complete something, or the pace of animals in a field, now humans had to keep up with the very machines that were supposed to serve us—and it’s only got worse from there.
This book takes a tour of many areas affected by this artificial “need for speed”, and how it harms not just our work-life balance, but also our eating habits, the medical attention we get, and even our love lives.
The prescription is deceptively simple, “slow down”. But Honoré dedicates the final three chapters of the book to the “how” of this, when of course there’s a lot the outside world will not accommodate—but where we can slow down, there’s good to be gained.
Bottom line: if you’ve ever felt that you could get all of your life into order if you could just pause the outside world for a week or two, this is the book for you.
Click here to check out In Praise of Slowness, and make time for what matters most!
Share This Post
-
Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
First things first… How much fiber should we be eating?
- The World Health Organization recommends we each get at least 25g of fiber per day:
- A more recent meta-review of studies, involving thousands of people and decades of time, suggests 25–29g is ideal:
- The British Nutritional Foundation gives 30g as the figure:
- The US National Academy of Sciences’ Institute of Medicine recommends 21g–38g per day, depending on age and sex:
- A large study last year gave 30–40g as the figure:
*This one is also a great read to understand more about the “why” of fiber
Meanwhile, the average American gets 16g of fiber per day.
So, how to get more fiber, without piling on too many carbs?
Foods that contain fiber generally contain carbs (there’s a limit to how much celery most people want to eat), so there are two key ideas here:
- Getting a good carb:fiber ratio
- Making substitutions that boost fiber without overdoing (or in some case, even changing) carbs
Meat → Lentils
Well-seasoned lentils can be used to replaced ground beef or similar. A cup of boiled lentils contains 18g of fiber, so you’re already outdoing the average American’s daily total.
Meat → Beans
Black beans are a top-tier option here (15g per cup, cooked weight), but many kinds of beans are great.
Chicken/Fish → Chickpeas
Yes, chicken/fish is already meat, but we’re making a case for chickpeas here. Cooked and seasoned appropriately, they do the job, and pack in 12g of fiber per cup. Also… Hummus!
Bonus: Hummus, eaten with celery sticks.
White pasta/bread → Wholewheat pasta/bread
This is one where “moderation is key”, but if you’re going to eat pasta/bread, then wholewheat is the way to go. Fiber amounts vary, so read labels, but it will always have far more than white.
Processed salty snacks → Almonds and other nuts
Nuts in general are great, but almonds are top-tier for fiber, amongst other things. A 40g handful of almonds contains about 10g of fiber.
Starchy vegetables → Non-starchy vegetables
Potatoes, parsnips, and their friends have their place. But they cannot compete with broccoli, peas, cabbage, and other non-starchy vegetables for fiber content.
Bonus: if you’re going to have starchy vegetables though, leave the skins on!
Fruit juice → Fruit
Fruit juice has had most, if not all, of its fiber removed. Eat an actual juicy fruit, instead. Apples and bananas are great options; berries such as blackberries and raspberries are even better (at around 8g per cup, compared to the 5g or so depending on the size of an apple/banana)
Processed cereals → Oats
5g fiber per cup. Enough said.
Summary
Far from being a Herculean task, getting >30g of fiber per day can be easily accomplished by a lentil ragù with wholewheat pasta.
If your breakfast is overnight oats with fruit and some chopped almonds, you can make it to >20g already by the time you’ve finished your first meal of the day.
Enjoy!
Share This Post
Related Posts
-
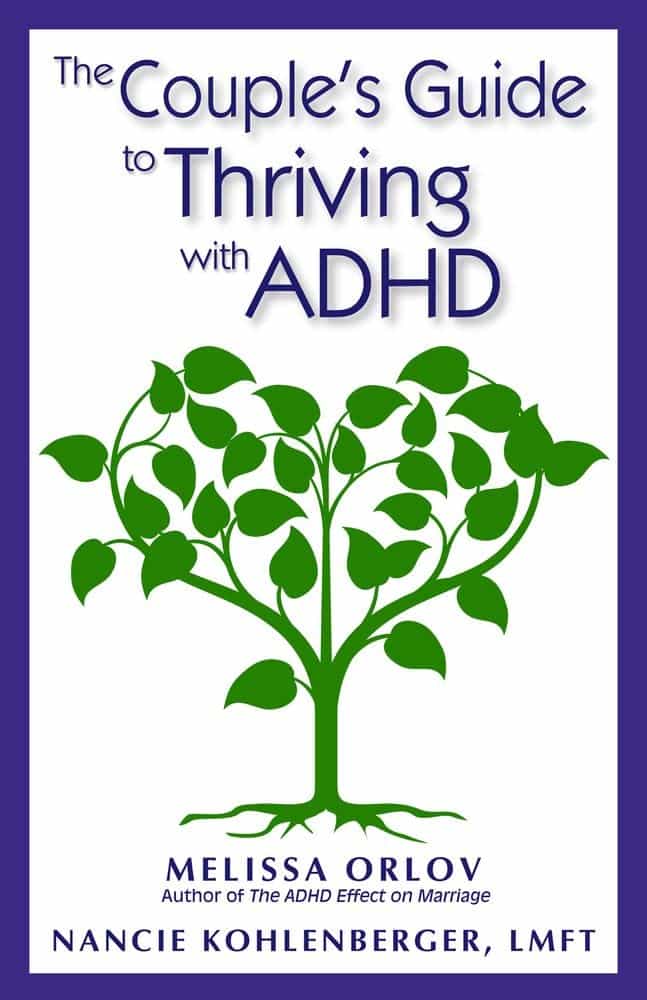
The Couple’s Guide to Thriving with ADHD – by Melissa Orlov and Nancie Kohlenberger
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ADHD (what a misleadingly-named condition) is most often undiagnosed in adults, especially older adults, and has far-reaching effects. This book explores those!
Oftentimes ADHD is not a deficit of attention, it’s just a lack of choice about where one’s attention goes. And the H? It’s mostly not what people think it is. The diagnostic criteria have moved far beyond the original name.
But in a marriage, ADHD symptoms such as wandering attention, forgetfulness, impulsiveness, and a focus on the “now” to the point of losing sight of the big picture (the forgotten past and the unplanned future), can cause conflict.
The authors write in a way that is intended for the ADHD and/or non-ADHD partner to read, and ideally, for both to read.
They shine light on why people with or without ADHD tend towards (or away from) certain behaviours, what miscommunications can arise, and how to smooth them over.
Best of all, an integrated plan for getting you both on the same page, so that you can tackle anything that arises, as the diverse team (with quite different individual strengths) that you are.
Bottom line: if you or a loved one has ADHD symptoms, this book can help you navigate and untangle what can otherwise sometimes get a little messy.
Click here to check out The Couple’s Guide to Thriving with ADHD, and learn how to do just that!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Exercise That Protects Your Brain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Neuroscientist In The Gym
This is Dr. Wendy Suzuki. She’s a neuroscientist, and an expert in the neurobiology of memory, as well as neuroplasticity, and the role of exercise in neuroprotection.
We’ve sneakily semi-featured her before when we shared her Big Think talk:
Brain Benefits In Three Months… Through Walking?
Today we’re going to expand on that a little!
A Quick Recap
To share the absolute key points of that already fairly streamlined rundown:
- Exercise boosts levels of neurotransmitters such as dopamine and serotonin (and, which wasn’t mentioned there, noradrenaline)
- These are responsible for motivation, happiness, and focus (amongst other things)
- Persistent exercise boosts certain regions of the brain in particular, most notably the pre-frontal cortex and the hippocampi*
- These are responsible for planning and memory (amongst other things)
Dr. Suzuki advocates for stepping up your exercise routine if you can, with more exercise generally being better than less (unless you have some special medical reason why that’s not the case for you).
*often referred to in the singular as the hippocampus, but you have one on each side of your brain (unless a serious accident/incident destroyed one, but you’ll know if that applies to you, unless you lost both, in which case you will not remember about it).
What kind(s) of workout?
While a varied workout is best for overall health, for these brain benefits specifically, what’s most important is that it raises your heart rate.
This is why in her Big Think talk we shared before, she talks about the benefits of taking a brisk walk daily. See also:
If that’s not your thing, though (and/or is for whatever reason an inaccessible form of exercise for you), there is almost certainly some kind of High Intensity Interval Training that is a possibility for you. That might sound intimidating, but if you have a bit of floor and can exercise for one minute at a time, then HIIT is an option for you:
How To Do HIIT (Without Wrecking Your Body)
Dr. Suzuki herself is an ardent fan of “intenSati” which blends cardio workouts with yoga for holistic mind-and-body fitness. In fact, she loves it so much that she became a certified exercise instructor:
How much is enough?
It’s natural to want to know the minimum we can do to get results, but Dr. Suzuki would like us to bear in mind that when it comes to our time spent exercising, it’s not so much an expense of time as an investment in time:
❝Exercise is something that when you spend time on it, it will buy you time when you start to work❞
Read more: A Neuroscientist Experimented on Her Students and Found a Powerful Way to Improve Brain Function
Ok, but we really want to know how much!
Dr. Suzuki recommends at least three to four 30-minute exercise sessions per week.
Note: this adds up to less than the recommended 150 minutes of moderate exercise per week, but high-intensity exercise counts for twice the minutes for these purposes, e.g. 1 minute of high-intensity exercise is worth 2 minutes of moderate exercise.
How soon will we see benefits?
Benefits start immediately, but stack up cumulatively with continued long-term exercise:
❝My lab showed that a single workout can improve your ability to shift and focus attention, and that focus improvement will last for at least two hours. ❞
…which is a great start, but what’s more exciting is…
❝The more you’re working out, the bigger and stronger your hippocampus and prefrontal cortex gets. Why is that important?
Because the prefrontal cortex and the hippocampus are the two areas that are most susceptible to neurodegenerative diseases and normal cognitive decline in aging. ❞
In other words, while improving your heart rate through regular exercise will help prevent neurodegeneration by the usual mechanism of reducing neuroinflammation… It’ll also build the parts of your brain most susceptible to decline, meaning that when/if decline sets in, it’ll take a lot longer to get to a critical level of degradation, because it had more to start with.
Read more:
Inspir Modern Senior Living | Dr. Wendy Suzuki Boosts Brain Health with Exercise
Want more from Dr. Suzuki?
You might enjoy her TED talk:
Click Here If The Embedded Video Doesn’t Load Automatically
Prefer text? TED.com has a transcript for you
Prefer lots of text? You might like her book, which we haven’t reviewed yet but will soon:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- Exercise boosts levels of neurotransmitters such as dopamine and serotonin (and, which wasn’t mentioned there, noradrenaline)
-
The Energy Plan – by James Collins
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There’s a lot of conflicting advice out there about how we should maintain our energy levels, for example:
- Eat fewer carbs!
- Eat more carbs!
- Eat slow-release carbs!
- Eat quick-release carbs!
- Practise intermittent fasting!
- Graze constantly throughout the day!
- Forget carbs and focus on fats!
- Actually it’s all about B-vitamins!
…and so on.
What Collins does differently is something much less-often seen:
Here, we’re advised on how to tailor our meals to our actual lifestyle, taking into account the day we actually have each day. For example:
- What will our energy needs be for the day?
- Will our needs be intense, or long, or both, or neither?
- What kind of recovery have we had, or do we need, from previous activities?
- Do we need to replace lost muscle glycogen, or are we looking to trim the fat?
- Are we doing a power-up or just maintenance today?
Rather than bidding us have a five-way spreadsheet and do advanced mathematics for every meal, though, Collins has done the hard work for us. The book explains the various principles in a casual format with a light conversational tone, and gives us general rules to follow.
These rules cover what to do for different times of day… and also, at different points in our life (the metabolic needs of a 13-year-old, 33-year-old, and 83-year-old, are very different!). That latter’s particularly handy, as a lot of books assume an age bracket for the reader, and this one doesn’t.
In short: a great book for anyone who wants to keep their energy levels up (throughout life’s ups and downs in activity) without piling on the pounds or starving oneself.
Click here to check out The Energy Plan on Amazon and fuel your days better!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: