Genius Gut – by Dr. Emily Leeming
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to the gut-brain information interchange, 90% of it is the gut talking to the brain (the brain is a good listener). As such, one of the best things we can do for our brain is ensure our gut has good things to say.
Dr. Leeming talks us through doing a quick initial assessment to judge the general goodness/badness of our current gut situation (based on output, not input, so it’s about the actual goodness/badness, not what we expect it should be), before going on to explain a lot of the anatomy and physiology at hand.
The hacks themselves may be, in their titles, things you already know—but where the real value of this book lies is in all the data and science collated under each of those hacks, allowing the reader to optimize everything rather than just guessing. Which can mean optimize by doing things as close to perfectly as possible, or it can mean optimize by doing/using the things that get the best results for the minimum effort. It’s up to you!
The style is very casual and friendly, even conversational, while not skimping on science (and indeed, citations are frequently provided for such).
Bottom line: if you’d like to improve your gut health, especially with the goal of improving your brain health, this is an excellent book for that.
Click here to check out Genius Gut, and make yours better for you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Avocado vs Goji Berries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing avocado to goji berries, we picked the avocado.
Why?
It takes a special non-dried food to beat a dried food for nutritional density, but avocado manages it!
In terms of macros, avocados have more (famously health) fat; mostly monounsaturated with some polyunsaturated and a little bit of saturated, with some omega-3 and omega-6, in a healthy ratio. Meanwhile, goji berries have more fiber, carbs, and protein. As for glycemic indices, avocados are low GI (40), but goji berries are zero-GI, or, functionally, a negative glycemic index as (notwithstanding their sugar content!) they have an overall lowering effect on blood sugars. In short, both of these fruits have very different things to offer in the macros category, so we’re declaring this round a tie.
In the category of vitamins, avocados have more of vitamins A, B1, B2, B3, B5, B6, B7, B9, E, K, and choline, while goji berries have more vitamin C. A clear win for avocados!
When it comes to minerals, avocados have more copper, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while goji berries have more calcium and iron. Another win for avocados!
In short, enjoy either or both (diversity is good), but for overall nutritional density, avocados win this superfood showdown today.
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Enjoy!
Share This Post
-
The Natural Facelift – by Sophie Perry
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this book isn’t: it’s mostly not about beauty, and it’s certainly not about ageist ideals of “hiding” aging.
The author herself discusses the privilege that is aging (not everyone gets to do it) and the importance of taking thankful pride in our lived-in bodies.
The title and blurb belie the contents of the book rather. Doubtlessly the publisher felt that extrinsic beauty would sell better than intrinsic wellbeing. As for what it’s actually more about…
Ever splashed your face in cold water to feel better? This book’s about revitalising the complex array of facial muscles (there are anatomical diagrams) and the often-tired and very diverse tissues that cover them, complete with the array of nerve endings very close to your CNS (not to mention the vagus nerve running just behind your jaw), and some of the most important blood vessels of your body, serving your brain.
With all that in mind, this book, full of useful therapeutic techniques, is a very, very far cry from “massage like this and you’ll look like you got photoshopped”.
The style varies, as some parts of explanation of principles, or anatomy, and others are hands-on (literally) guides to the exercises, but it is all very clear and easy to understand/follow.
Bottom line: aspects of conventional beauty may be a side-effect of applying the invigorating exercises described in this book. The real beauty is—literally—more than skin-deep.
Click here to check out The Natural Facelift, and order yours!
Share This Post
-
The Bee’s Knees?
If you’d like to pre-empt that runny nose, some say that local honey is the answer. The rationale is that bees visiting the local sources of pollen and making honey will introduce the same allergens to you in a non allergy-inducing fashion (the honey). The result? Inoculation against the allergens in question.
But does it work?
Researching this, we found a lot of articles saying there was no science to back it up.
And then! We found one solitary study from 2013, and the title was promising:
But we don’t stop at titles; that’s not the kind of newsletter we are. We pride ourselves on giving good information!
And it turned out, upon reading the method and the results, that:
- Both the control and test groups also took loratadine for the first 4 weeks of the study
- The test group additionally took 1g/kg bodyweight of honey, daily—so for example if you’re 165lb (75kg), that’s about 4 tablespoons per day
- The control group took the equivalent amount of honey-flavored syrup
- Both groups showed equal improvements by week 4
- The test group only showed continued improvements (over the control group) by week 8
The researchers concluded from this:
❝Honey ingestion at a high dose improves the overall and individual symptoms of AR, and it could serve as a complementary therapy for AR.❞
We at 10almonds concluded from this:
❝That’s a lot of honey to eat every day for months!❞
We couldn’t base an article on one study from a decade ago, though! Fortunately, we found a veritable honeypot of more recent research, in the form of this systematic review:
Read: The Potential Use Of Honey As A Remedy For Allergic Diseases
…which examines 13 key studies and 43 scientific papers over the course of 21 years. That’s more like it! This was the jumping-off point we needed into more useful knowledge.
We’re not going to cite all those here—we’re a health and productivity newsletter, not an academic journal of pharmacology, but we did sift through them so that you don’t have to, and:
The researchers (of that review) concluded:
❝Although there is limited evidence, some studies showed remarkable improvements against certain types of allergic illnesses and support that honey is an effective anti-allergic agent.❞
Our (10almonds team) further observations included:
- The research review notes that a lot of studies did not confirm which phytochemical compounds specifically are responsible for causing allergic reactions and/or alleviating such (so: didn’t always control for what we’d like to know, i.e. the mechanism of action)
- Some studies showed results radically different from the rest. The reviewers put this down to differences that were not controlled-for between studies, for example:
- Some studies used very different methods to others. There may be an important difference between a human eating a tablespoon of honey, and a rat having aerosolized honey shot up its nose, for instance. We put more weight to human studies than rat studies!
- Some kinds of honey (such as manuka) contain higher quantities of gallic acid which itself can relieve allergies by chemically inhibiting the release of histamine. In other words, never mind pollen-based inoculations… it’s literally an antihistamine.
- Certain honeys (such as tualang, manuka and gelam) contain higher quantities of quercetin. What’s quercetin? It’s a plant flavonoid that a recent study has shown significantly relieves symptoms of seasonal allergies. So again, it works, just not for the reason people say!
In summary:
The “inoculation by local honey” thing specifically may indeed remain “based on traditional use only” for now.
But! Honey as a remedy for allergies, especially manuka honey, has a growing body of scientific evidence behind it.
Bottom line:
If you like honey, go for it (manuka seems best)! It may well relieve your symptoms.
If you don’t, off-the-shelf antihistamines remain a perfectly respectable option.
Share This Post
Related Posts
-
The Myth of Normal – by Dr. Gabor Maté and Daniel Maté
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of popular beliefs (and books!) start with the assumption that everyone is, broadly speaking, “normal”. That major diversions from “normal” happen only to other people… And that minor diversions from “normal” are just something to suck up and get over—magically effecting a return to “normalcy”.
Dr. Maté, however, will have none of these unhelpful brush-offs, and observes that in fact most if not all of us have been battered by the fates one way or another. We just:
- note that we have more similarities than differences, and
- tend to hide our own differences (to be accepted) or overlook other people’s (to make them more acceptable).
How is this more helpful? Well, the above approach isn’t always, but Mate has an improvement to offer:
We must see flawed humans (including ourselves) as the product of our environments… and/but see this a reason to look at improving those environments!
Beyond that…
The final nine chapters of the books he devotes to “pathways to wholeness” and, in a nutshell, recovery. Recovery from whatever it was for you. And if you’ve had a life free from anything that needs recovering from, then congratulations! You doubtlessly have at least one loved one who wasn’t so lucky, though, so this book still makes for excellent reading.
Dr. Maté was awarded the Order of Canada for his medical work and writing. His work has mostly been about addiction, trauma, stress, and childhood development. He co-wrote this book with his son, Daniel.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Retrain Your Brain – by Dr. Seth Gillihan
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
15-Minute Arabic”, “Sharpen Your Chess Tactics in 24 Hours”, “Change Your Life in 7 Days”, “Cognitive Behavioral Therapy in 7 weeks”—all real books from this reviewer’s shelves.
The thing with books with these sorts of time periods in the titles is that the time period in the title often bears little relation to how long it takes to get through the book. So what’s the case here?
You’ll probably get through it in more like 7 days, but the pacing is more important than the pace. By that we mean:
Dr. Gillihan starts by assuming the reader is at best “in a rut”, and needs to first pick a direction to head in (the first “week”) and then start getting one’s life on track (the second “week”).
He then gives us, one by one, an array of tools and power-ups to do increasingly better. These tools aren’t just CBT, though of course that features prominently. There’s also mindfulness exercises, and holistic / somatic therapy too, for a real “bringing it all together” feel.
And that’s where this book excels—at no point is the reader left adrift with potential stumbling-blocks left unexamined. It’s a “whole course”.
Bottom line: whether it takes you 7 hours or 7 months, “Cognitive Behavioral Therapy in 7 Weeks” is a CBT-and-more course for people who like courses to work through. It’ll get you where you’re going… Wherever you want that to be for you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
An Addiction Expert’s Insights On Festive Drinking
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
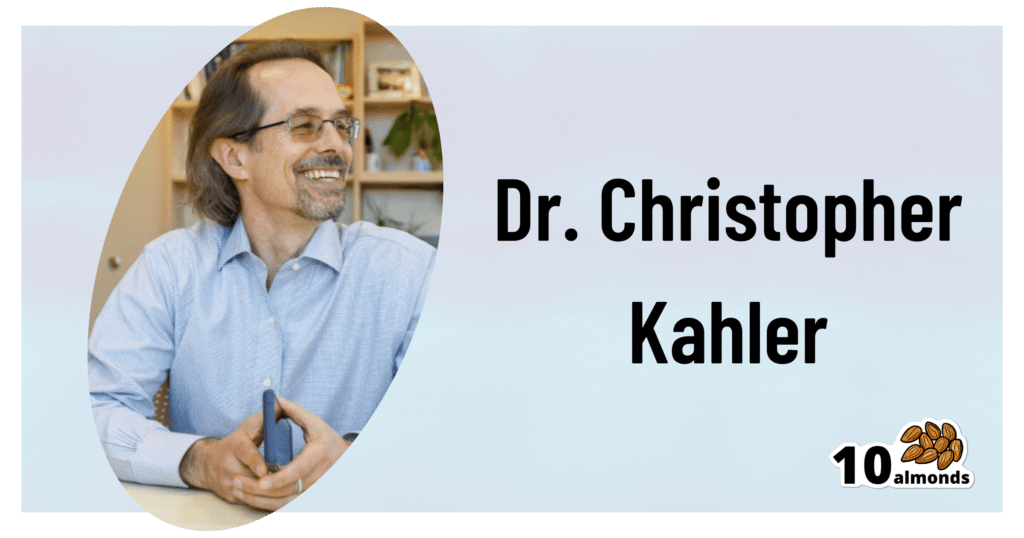
This is Dr. Christopher Kahler. He’s Professor of Behavioral and Social Sciences, Director of Alcohol and Addiction Studies, Professor of Psychiatry and Human Behavior, all at Brown University.
What does he want us to know?
It’s the trickiest time of the year
Per stats, alcohol sales peak in December, with the heaviest drinking being from mid-December (getting an early start on the Christmas cheer) to New Year’s Eve. As for why, there’s a collection of reasons, as he notes:
❝The main challenge is there’s an extra layer of stress, with a lot of obligations and expectations from friends and family. We’re around people who maybe we’re not usually around, and in larger groups. It’s also a time of heightened emotion and, for some people, loneliness.
On top of that, alcohol use is built into a lot of our winter holiday traditions. It’s often marketed as part of the “good life.” We’re expected to have alcohol when we celebrate.❞
As for how much alcohol is safe to drink… According to the World Health Organization, the only safe amount of alcohol is zero:
Dr. Kahler acknowledges, however, that many people will wish to imbibe anyway, and indeed, he himself does drink a little, but endeavours to do so mindfully, and as such, he recommends that we…
HALT!
Dr. Kahler counsels us against making decisions (including the decision to drink alcohol), on occasions when we are one or more of the following:
- Hungry
- Angry
- Lonely
- Tired
He also notes that around this time of year, often our normal schedules and habits are disrupted, which introduces more microdecisions to our daily lives, which in turn means more “decision fatigue”, and the greater chance of making bad decisions.
We share some practical tips on how to reduce the chances of thusly erring, here:
Set your intentions now
He bids us figure out what our goal is, and really think it through, including not just “how many drinks to have” if we’re drinking, but also such things as “what feelings are likely to come up”. Because, if we’ve historically used alcohol as a maladaptive coping mechanism, we’re going to need a different, better, healthier coping mechanism (we talked more about that in our above-linked article about reducing or quitting alcohol, too, with some examples).
He also suggests that we memorize our social responses—exactly what we’re going to say if offered a drink, for example:
❝It’s important to know what you’re going to say about your alcohol use. If someone asks if they can get you a drink, good responses could be: “A glass of water would be great” or “Do you have any non-alcoholic cider?” You don’t have to explain yourself. Just ask for what you want, because saying no to someone can be difficult.❞
See also:
December’s Traps To Plan Around
Mix it up and slow it down
No, that doesn’t mean mix yourself a sloe gin cocktail. But rather, it’s about alternating alcoholic and non-alcoholic drinks, to give your body half a chance to process the alcohol, and also to rehydrate a little along the way.
We talk about this and other damage-limitation methods, here:
How To Reduce The Harm Of Festive Drinking (Without Abstaining)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: