From straight to curly, thick to thin: here’s how hormones and chemotherapy can change your hair
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Head hair comes in many colours, shapes and sizes, and hairstyles are often an expression of personal style or cultural identity.
Many different genes determine our hair texture, thickness and colour. But some people’s hair changes around the time of puberty, pregnancy or after chemotherapy.
So, what can cause hair to become curlier, thicker, thinner or grey?
Curly or straight? How hair follicle shape plays a role
Hair is made of keratin, a strong and insoluble protein. Each hair strand grows from its own hair follicle that extends deep into the skin.
Curly hair forms due to asymmetry of both the hair follicle and the keratin in the hair.
Follicles that produce curly hair are asymmetrical and curved and lie at an angle to the surface of the skin. This kinks the hair as it first grows.
The asymmetry of the hair follicle also causes the keratin to bunch up on one side of the hair strand. This pulls parts of the hair strand closer together into a curl, which maintains the curl as the hair continues to grow.
Follicles that are symmetrical, round and perpendicular to the skin surface produce straight hair.
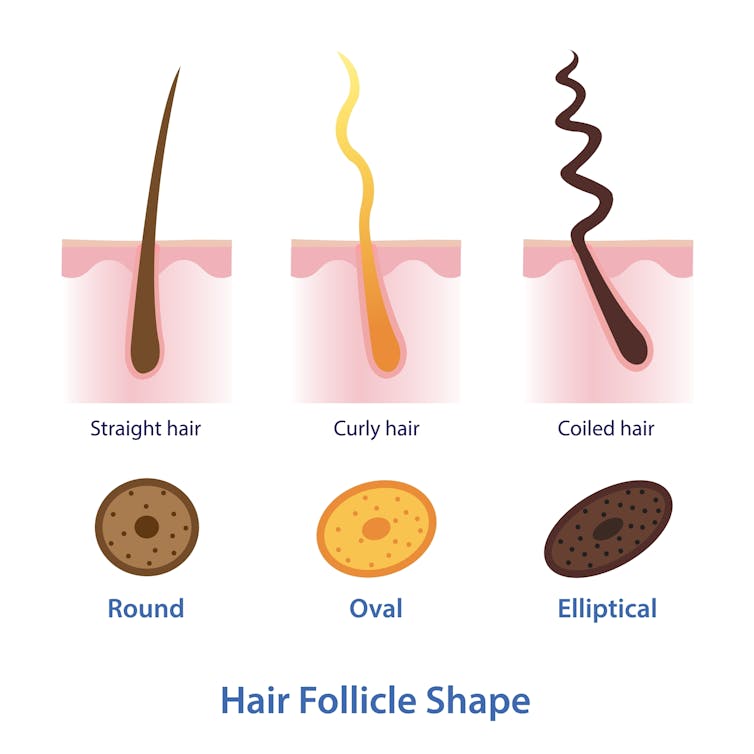
Mosterpiece/Shutterstock
Life changes, hair changes
Our hair undergoes repeated cycles throughout life, with different stages of growth and loss.
Each hair follicle contains stem cells, which multiply and grow into a hair strand.
Head hairs spend most of their time in the growth phase, which can last for several years. This is why head hair can grow so long.
Let’s look at the life of a single hair strand. After the growth phase is a transitional phase of about two weeks, where the hair strand stops growing. This is followed by a resting phase where the hair remains in the follicle for a few months before it naturally falls out.
The hair follicle remains in the skin and the stems cells grow a new hair to repeat the cycle.
Each hair on the scalp is replaced every three to five years.

Just Life/Shutterstock
Hormone changes during and after pregnancy alter the usual hair cycle
Many women notice their hair is thicker during pregnancy.
During pregnancy, high levels of oestrogen, progesterone and prolactin prolong the resting phase of the hair cycle. This means the hair stays in the hair follicle for longer, with less hair loss.
A drop in hormones a few months after delivery causes increased hair loss. This is due to all the hairs that remained in the resting phase during pregnancy falling out in a fairly synchronised way.
Hair can change around puberty, pregnancy or after chemotherapy
This is related to the genetics of hair shape, which is an example of incomplete dominance.
Incomplete dominance is when there is a middle version of a trait. For hair, we have curly hair and straight hair genes. But when someone has one curly hair gene and one straight hair gene, they can have wavy hair.
Hormonal changes that occur around puberty and pregnancy can affect the function of genes. This can cause the curly hair gene of someone with wavy hair to become more active. This can change their hair from wavy to curly.
Researchers have identified that activating specific genes can change hair in pigs from straight to curly.
Chemotherapy has very visible effects on hair. Chemotherapy kills rapidly dividing cells, including hair follicles, which causes hair loss. Chemotherapy can also have genetic effects that influence hair follicle shape. This can cause hair to regrow with a different shape for the first few cycles of hair regrowth.

Igor Ivakhno/Shutterstock
Hormonal changes as we age also affect our hair
Throughout life, thyroid hormones are essential for production of keratin. Low levels of thyroid hormones can cause dry and brittle hair.
Oestrogen and androgens also regulate hair growth and loss, particularly as we age.
Balding in males is due to higher levels of androgens. In particular, high dihydrotestosterone (sometimes shortened to DHT), which is produced in the body from testosterone, has a role in male pattern baldness.
Some women experience female pattern hair loss. This is caused by a combination of genetic factors plus lower levels of oestrogen and higher androgens after menopause. The hair follicles become smaller and smaller until they no longer produce hairs.
Reduced function of the cells that produce melanin (the pigment that gives our hair colour) is what causes greying.
Theresa Larkin, Associate professor of Medical Sciences, University of Wollongong
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Fix Your Upper Back With These Three Steps
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to back pain, the lower back gets a lot of attention, but what about when it’s nearer the neck and shoulders?
Reaching for better health
In this short video, Liv describes and shows three exercises:
Exercise 1: Thoracic Pullover (Dumbbell Pullover)
Purpose: Improves overhead reach and shoulder mobility.
Equipment: light weight, yoga block, or foam roller.
Steps:- Lie on the floor with the foam roller/block beneath the upper back.
- Hold the weight in both hands, arms extended upward.
- Inhale deeply and reach the weight toward the ceiling.
- Exhale and arc your spine over the block, moving the weight backward.
- Keep core tension to maintain a neutral lower back position.
- Perform 10 repetitions.
Exercise 2: Rotational Mobility Stretch
Purpose: enhances torso rotation, core strength, and hip mobility.
Equipment: none (or a mat)
Steps:- Lie on your side with knees stacked at 90° and arms extended in front.
- Hold a weight in the top hand.
- Inhale and lift the top arm toward the ceiling, extending the shoulder blade.
- Exhale and twist your torso, allowing the arm to move toward the floor.
- Modify by extending the bottom leg for a deeper twist if needed.
- Perform 6 reps per side, switching legs and repeating on the other side.
Exercise 3: Doorway/Pole Side Stretch
Purpose: targets multiple areas for a deep, satisfying stretch.
Equipment: door frame, pole, or wall.
Steps:- Stand at arm’s length from the wall or frame.
- Cross the outer leg (furthest from the wall) behind the inner leg.
- Place the closest hand on the wall and reach the other arm overhead.
- Grip the wall or frame with the top hand, pressing away with the bottom hand.
- Lean into a banana-shaped curve and rotate your chest upward for a deeper stretch.
- Hold for 20–30 seconds per side and repeat 2–3 times.
For more on all of these, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Take care!
Share This Post
-
Mushrooms vs Eggplant – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing mushrooms to eggplant, we picked the mushrooms.
Why?
First, you may be wondering: which mushrooms? Button mushrooms? White mushrooms? Chestnut mushrooms? Portobello mushrooms? And the answer is yes. Those (and more; it represents most mushrooms that are commonly sold fresh in western supermarkets) are all the same species at different ages; namely, Agaricus bisporus—not to be mistaken for fly agaric, which despite the name, is not even a member of the Agaricus genus, and is in fact Amanita muscari. This is an important distinction, because fly agaric is poisonous, though fatality is rare, and it’s commonly enjoyed recreationally (after some preparation, which reduces its toxicity) for its psychoactive effects. It’s the famous red one with white spots. Anyway, today we will be talking instead about Agaricus bisporus, which is most popular western varieties of “edible mushroom”.
With that in mind, let’s get down to it:
In terms of macros, mushrooms contain more than 3x the protein, while eggplant contains nearly 2x the carbs and 3x the fiber. We’ll call this a tie for macros.
As for vitamins, mushrooms contain more of vitamins B1, B2, B3, B5, B6, B7, B9, B12, D, and choline, while eggplant contains more of vitamins A, E, and K. Most notably for vegans, mushrooms are a good non-animal source of vitamins B12 and D, which nutrients are not generally found in plants. Mushrooms, of course, are not technically plants. In any case, the vitamins category is an easy win for mushrooms.
When it comes to minerals, mushrooms have more copper, iron, phosphorus, potassium, selenium, and zinc, while eggplant has more calcium, magnesium, and manganese. Another easy win for mushrooms.
One final thing worth noting is that mushrooms are a rich source of the amino acid ergothioneine, which has been called a “longevity vitamin” for its healthspan-increasing effects (see our article below).
Meanwhile, in the category of mushrooms vs eggplant, mushrooms don’t leave much room for doubt and are the clear winner here.
Want to learn more?
You might like to read:
The Magic of Mushrooms: “The Longevity Vitamin” (That’s Not A Vitamin)
Take care!
Share This Post
-
Cupping: How It Works (And How It Doesn’t)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Good Health By The Cup?
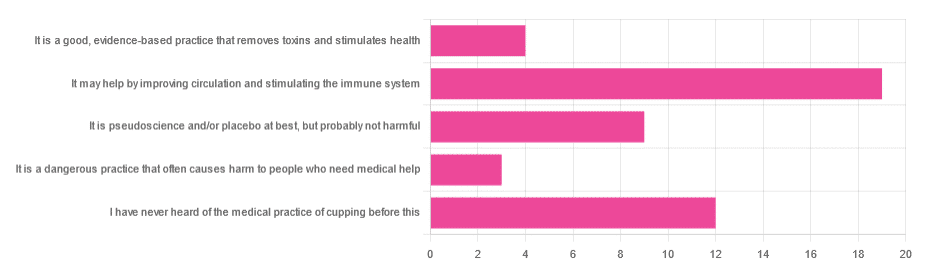
In Tuesday’s newsletter, we asked you for your opinion of cupping (the medical practice), and got the above-depicted, below-described, set of responses:
- About 40% said “It may help by improving circulation and stimulating the immune system”
- About 26% said “I have never heard of the medical practice of cupping before this”
- About 19% said “It is pseudoscience and/or placebo at best, but probably not harmful
- About 9% said “It is a good, evidence-based practice that removes toxins and stimulates health”
- About 6% said “It is a dangerous practice that often causes harm to people who need medical help”
So what does the science say?
First, a quick note for those unfamiliar with cupping: it is the practice of placing a warmed cup on the skin (open side of the cup against the skin). As the warm air inside cools, it reduces the interior air pressure, which means the cup is now (quite literally) a suction cup. This pulls the skin up into the cup a little. The end result is visually, and physiologically, the same process as what happens if someone places the nozzle of a vacuum cleaner against their skin. For that matter, there are alternative versions that simply use a pump-based suction system, instead of heated cups—but the heated cups are most traditional and seem to be most popular. See also:
National Center for Complementary and Integrative Health | Cupping
It is a dangerous practice that often causes harm to people who need medical help: True or False?
False, for any practical purposes.
- Directly, it can (and usually does) cause minor superficial harm, much like many medical treatments, wherein the benefits are considered to outweigh the harm, justifying the treatment. In the case of cupping, the minor harm is usually a little bruising, but there are other risks; see the link we gave just above.
- Indirectly, it could cause harm by emboldening a person to neglect a more impactful treatment for their ailment.
But, there’s nothing for cupping akin to the “the most common cause of death is when someone gets a vertebral artery fatally severed” of chiropractic, for example.
It is a good, evidence-based practice that removes toxins and stimulates health: True or False?
True and False in different parts. This one’s on us; we included four claims in one short line. But let’s look at them individually:
- Is it good? Well, those who like it, like it. It legitimately has some mild health benefits, and its potential for harm is quite small. We’d call this a modest good, but good nonetheless.
- Is it evidence-based? Somewhat, albeit weakly; there are some papers supporting its modest health claims, although the research is mostly only published in journals of alternative medicine, and any we found were in journals that have been described by scientists as pseudoscientific.
- Does it remove toxins? Not directly, at least. There is also a version that involves making a small hole in the skin before applying the cup, the better to draw out the toxins (called “wet cupping”). This might seem a little medieval, but this is because it is from early medieval times (wet cupping’s first recorded use being in the early 7th century). However, the body’s response to being poked, pierced, sucked, etc is to produce antibodies, and they will do their best to remove toxins. So, indirectly, there’s an argument.
- Does it stimulate health? Yes! We’ll come to that shortly. But first…
It is pseudoscience and/or placebo at best, but probably not harmful: True or False?
True in that its traditionally-proposed mechanism of action is a pseudoscience and placebo almost certainly plays a strong part, and also in that it’s generally not harmful.
On it being a pseudoscience: we’ve talked about this before, but it bears repeating; just because something’s proposed mechanism of action is pseudoscience, doesn’t necessarily mean it doesn’t work by some other mechanism of action. If you tell a small child that “eating the rainbow” will improve their health, and they believe this is some sort of magical rainbow power imbuing them with health, then the mechanism of action that they believe in is a pseudoscience, but eating a variety of colorful fruit and vegetables will still be healthy.
In the case of cupping, its proposed mechanism of action has to do withbalancing qi, yin and yang, etc (for which scientific evidence does not exist), in combination with acupuncture lore (for which some limited weak scientific evidence exists). On balancing qi, yin and yang etc, this is a lot like Europe’s historically popular humorism, which was based on the idea of balancing the four humors (blood, yellow bile, black bile, phlegm). Needless to say, humorism was not only a pseudoscience, but also eventually actively disproved with the advent of germ theory and modern medicine. Cupping therapy is not more scientifically based than humorism.
On the placebo side of things, there probably is a little more to it than that; much like with acupuncture, a lot of it may be a combination of placebo and using counter-irritation, a nerve-tricking method to use pain to reduce pain (much like pressing with one’s nail next to an insect bite).
Here’s one of the few studies we found that’s in what looks, at a glance, to be a reputable journal:
Cupping therapy and chronic back pain: systematic review and meta-analysis
It may help by improving circulation and stimulating the immune system: True or False?
True! It will improve local circulation by forcing blood into the area, and stimulate the immune system by giving it a perceived threat to fight.
Again, this can be achieved by many other means; acupuncture (or just “dry needling”, which is similar but without the traditional lore), a cold shower, and/or exercise (and for that matter, sex—which combines exercise, physiological arousal, and usually also foreign bodies to respond to) are all options that can improve circulation and stimulate the immune system.
You can read more about using some of these sorts of tricks for improving health in very well-evidenced, robustly scientific ways here:
The Stress Prescription (Against Aging!)
Take care!
Share This Post
Related Posts
-
9 Reasons To Avoid Mobility Training
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Why might someone not want to do mobility training? Here are some important reasons:
Make an informed choice
Here’s Liv’s hit-list of reasons to skip mobility training:
- Poor Circulation: Avoid mobility training if you don’t want to improve or maintain good blood circulation, which aids muscle recovery and reduces soreness.
- Low Energy Levels: Mobility training increases oxygen flow to the brain and muscles, boosting energy. Skip it if you prefer feeling sluggish!
- Digestive Health: Stretches that rotate the torso aid digestion and relieve bloating. Definitely best to avoid it if you’re uninterested in improving digestive health.
- Joint Health: Mobility work stimulates synovial fluid production, reducing joint friction and promoting longevity. You can skip it if you don’t care about comfortable movement.
- Sleep Quality: Gentle stretching triggers relaxation, aiding restful sleep. Avoid it if you enjoy restless nights!
- Pain Tolerance: Stretching trains the nervous system to handle discomfort better. Skip it if you prefer suffering 🙂
- Headache Reduction: Mobility work relieves tension in the neck and shoulders, reducing the occurrence and severity of headaches. No need to do it if you’re fine with frequent headaches.
- Immune System Support: Mobility training boosts lymphatic circulation, aiding the immune system. Avoid it if you prefer your immune system to get exciting in a bad way.
- Stress Reduction: Mobility exercises release endorphins and lower cortisol levels, reducing stress. So, it is certainly best to skip it if you prefer feeling stressed and enjoy the many harmful symptoms of high cortisol levels!
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Mobility As Though A Sporting Pursuit: Train For The Event Of Your Life!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
As The Summer Gets Hotter Still…
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I would love to see an article about heat dehydrated illness….so much of the US is under hot conditions. I had an fainting sweating episode and now trying to recoup from it. What should we do? Drink water,rest…???❞
We have done some of this, but it’s always a good one to revisit! Last summer (N. Hemisphere summer), we wrote this:
Stay Safe From Heat Exhaustion & Heatstroke!
…and this year, it’s getting hotter still (and is already the hottest summer on record), with certainly much of the US seriously affected, as you say. Next year, it will probably be worse again; climate change is getting predictable like that, and likely will continue until fixed. We are but a health science publication, so we can’t fix the world’s climate, but we can reiterate the above advice, and urge everyone to take it seriously.
Note: heat exhaustion and heatstroke kill. Yes, we’re including heat exhaustion in that, because by the time you get heat exhaustion, you’re often not in the best state of mind to take the correct steps to avoid the heatstroke that follows.
To think otherwise would be akin to thinking “falling never killed anyone; it’s only when you stop falling that it’s dangerous”.
This summer, we did also write this more niche article:
…whose advice won’t apply to everyone, but will be helpful to some, and honestly, some of that advice does go for everyone.
One thing we didn’t write about in those articles that we’ll add here:
Humidity is dangerous:
- Dry heat: you sweat, the sweat evaporates, cooling you. As well as losing heat, you’ve also now lost water and salts, which you’ll need to replenish, but your body is operating correctly.
- Humid heat: you sweat, and now you are just sweaty until further notice. It doesn’t evaporate because the surrounding humidity doesn’t provide the physics for that. Not only are you not losing heat through evaporating sweat, but also, if you’re wearing clothes, that’s now an insulating layer you’re wearing.
…so that means, watch the humidity as carefully as you watch the temperature, and when it’s high, get extra serious about finding ways to keep yourself cool (e.g. shade, rest, cooling showers etc if you can, that kind of thing).
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Obesity Code – by Dr. Jason Fung
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Firstly, if you have already read Dr. Fung’s other book, The Diabetes Code, which we reviewed a little while ago, you can probably skip this one. It has mostly the same information, presented with a different focus.
While The Diabetes Code assumes you are diabetic, or prediabetic, or concerned about avoiding/reversing those conditions, The Obesity Code assumes you are obese, or heading in that direction, or otherwise are concerned about avoiding/reversing obesity.
What it’s not, though, is a weight loss book. Will it help if you want to lose weight? Yes, absolutely. But there is no talk here of weight loss goals, nor any motivational coaching, nor week-by-week plans, etc.
Instead, it’s more an informative textbook. With exactly the sort of philosophy we like here at 10almonds: putting information into people’s hands, so everyone can make the best decisions for themselves, rather than blindly following someone else’s program.
Dr. Fung explains why various dieting approaches don’t work, and how we can work around such things as our genetics, as well as most external factors except for poverty. He also talks us through how to change our body’s insulin response, and get our body working more like a lean machine and less like a larder for hard times.
Bottom line: this is a no-frills explanation of why your body does what it does when it comes to fat storage, and how to make it behave differently about that.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: