For women with antenatal depression, micronutrients might help them and their babies – new study
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.

Julia J Rucklidge, University of Canterbury; Elena Moltchanova, University of Canterbury; Roger Mulder, University of Otago, and Siobhan A Campbell, University of Canterbury
Antenatal depression affects 15% to 21% of pregnant women worldwide. It can influence birth outcomes and children’s development, as well as increase the risk of post-natal depression.
Current treatments like therapy can be inaccessible and antidepressants can carry risks for developing infants.
Over the past two decades, research has highlighted that poor nutrition is a contributing risk factor to mental health challenges. Most pregnant women in New Zealand aren’t adhering to nutritional guidelines, according to a longitudinal study. Only 3% met the recommendations for all food groups.
Another cohort study carried out in Brazil shows that ultra-processed foods (UPF) accounted for at least 30% of daily dietary energy during pregnancy, displacing healthier options.
UPFs are chemically manufactured and contain additives to improve shelf life, as well as added sugar and salt. Importantly, they are low in essential micronutrients (vitamins and minerals).
The consumption of these foods is concerning because a nutrient-poor diet during pregnancy has been linked to poorer mental health outcomes in children. This includes depression, anxiety, hyperactivity, and inattention.
Increasing nutrients in maternal diets and reducing consumption of UPFs could improve the mental health of the mother and the next generation. Good nutrition can have lifelong benefits for the offspring.
However, there are multiple factors that mean diet change alone may not in itself be sufficient to address mental health challenges. Supplementing with additional nutrients may also be important to address nutritional needs during pregnancy.
Micronutrients as treatment for depression
Our earlier research suggests micronutrient supplements for depression have benefits outside pregnancy.
But until now there have been no published randomised controlled trials specifically designed to assess the efficacy and safety of broad-spectrum micronutrients on antenatal depression and overall functioning.
The NUTRIMUM trial, which ran between 2017 and 2022, recruited 88 women in their second trimester of pregnancy who reported moderate depressive symptoms. They were randomly allocated to receive either 12 capsules (four pills, three times a day) of a broad-spectrum micronutrient supplement or an active placebo containing iodine and riboflavin for a 12-week period.
Micronutrient doses were generally between the recommended dietary allowance and the tolerable upper level.
Based on clinician ratings, micronutrients significantly improved overall psychological functioning compared to the placebo. The findings took into account all noted changes based on self-assessment and clinician observations. This includes sleep, mood regulation, coping, anxiety and side effects.

Both groups reported similar reductions in symptoms of depression. More than three quarters of participants were in remission at the end of the trial. But 69% of participants in the micronutrient group rated themselves as “much” or “very much” improved, compared to 39% in the placebo group.
Participants taking the micronutrients also experienced significantly greater improvements in sleep and overall day-to-day functioning, compared to participants taking the placebo. There were no group differences on measures of stress, anxiety and quality of life.
Importantly, there were no group differences in reported side effects, and reports of suicidal thoughts dropped over the course of the study for both groups. Blood tests confirmed increased vitamin levels (vitamin C, D, B12) and fewer deficiencies in the micronutrient group.
Micronutrients were particularly helpful for women with chronic mental health challenges and those who had taken psychiatric medications in the past. Those with milder symptoms improved with or without the micronutrients, suggesting general care and monitoring might suffice for some women.
The benefits of micronutrients were comparable to psychotherapy but with less contact. There are no randomised controlled trials of antidepressant medication to compare these results.
Retention in the study was good (81%) and compliance excellent (90%).
Beyond maternal mental health
We followed the infants of mothers enrolled in the NUTRIMUM trial (who were therefore exposed to micronutrients during pregnancy) for 12 months, alongside infants from the general population of Aotearoa New Zealand.
This second group of infants from the general population contained a smaller sub-group who were exposed to antidepressant medication for the treatment of antenatal depression.
We assessed the neuro-behavioural development of each infant within the first four weeks of life, and temperament up to one year after birth.
These observational follow-ups showed positive effects of micronutrients on the infants’ ability to regulate their behaviour. These results were on par with or better than typical pregnancies, and better than treatments with antidepressants.

Infants exposed to micronutrients during pregnancy were significantly better at attending to external stimuli. They were also better able to block out external stimuli during sleep. They showed fewer signs of stress and had better muscle tone compared to infants not exposed to micronutrients.
They also displayed greater ability to interact with their environment. They were better at regulating their emotional state and had fewer abnormal muscle reflexes than infants exposed to antidepressant medication in pregnancy.
Reassuringly, micronutrients had no negative impact on infant temperament.
These findings highlight the potential of micronutrients as a safe and effective alternative to traditional medication treatments for antenatal depression.
The prenatal environment sets the foundation for a child’s future. Further investigation into the benefits of micronutrient supplementation would gives us more confidence in their use for other perinatal (from the start of pregnancy to a year after birth) mental health issues. This could provide future generations with a better start to life.
We would like to acknowledge the contribution of Dr Hayley Bradley to this research project.
Julia J Rucklidge, Professor of Psychology, University of Canterbury; Elena Moltchanova, Professor of Statistics, University of Canterbury; Roger Mulder, Professor of Psychiatry, University of Otago, and Siobhan A Campbell, Intern Psychologist, Researcher – Te Puna Toiora (Mental Health and Nutrition Research Lab), University of Canterbury
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
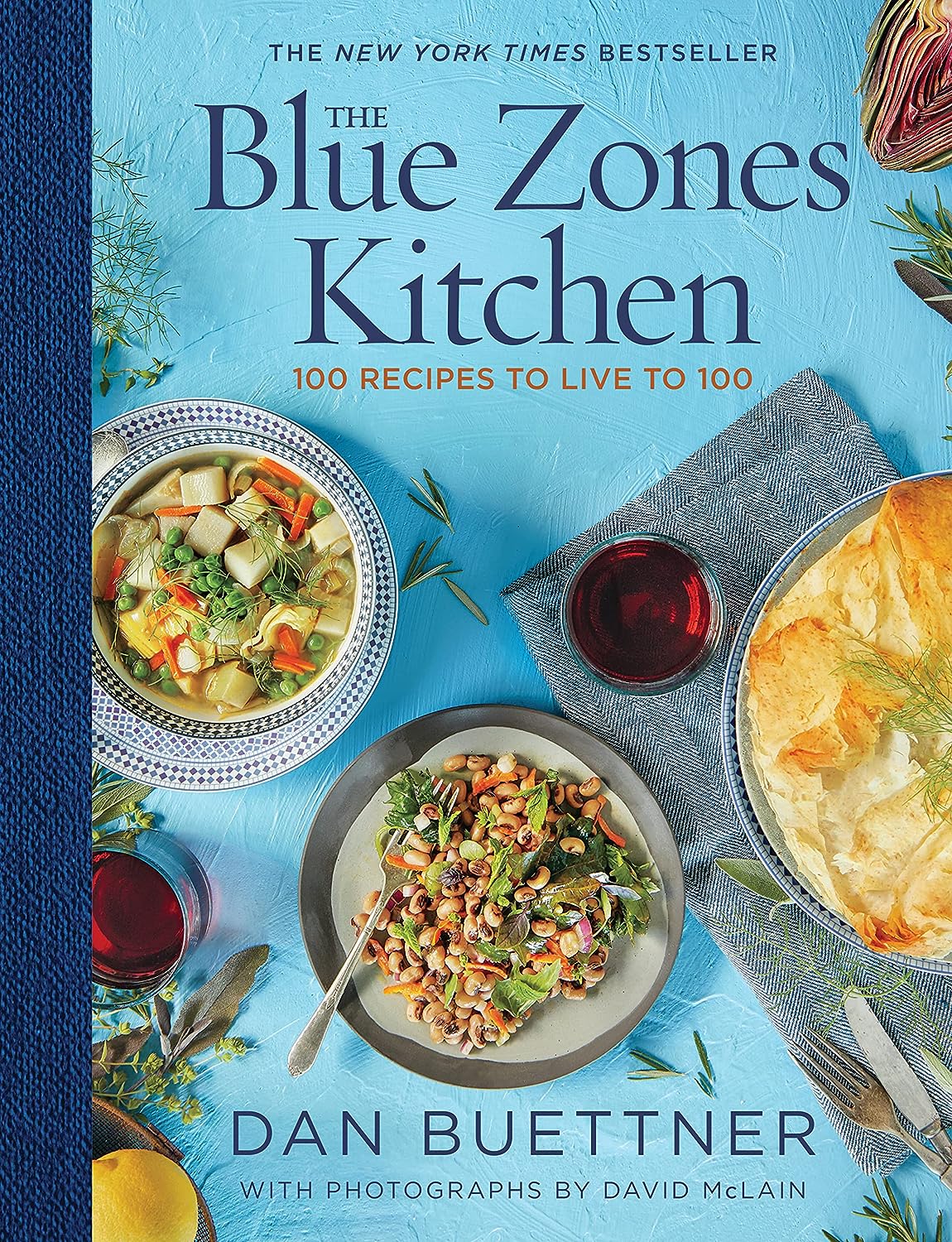
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Somatic Exercises For Nervous System Regulation – by Rose Kilian
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about the vagus nerve, its importance, and how to make use of it, but it’s easy to let it slip from one’s mind when it comes to exercises. This book fixes that!
The promised 35 exercises are quite a range, and are organized into sections:
- Revitalizing through breath
- Stress and tension release
- Spinal and postural health
- Mindfulness and grounding
- Movements for flexibility
- Graceful balance and focus
While it’s not necessary to do all 35 exercises, it’s recommended to do at least some from each section, to “cover one’s bases”, and enjoy the best of all worlds.
The exercises are drawn from many sources, but tai chi and yoga are certainly the most well-represented. Others, meanwhile, are straight from physiotherapy or are things one might expect to be advised at a neurology consultation.
Bottom line: if you’d like to take better care of your vagus nerve, the better for it to take care of you, this book can certainly help with that.
Click here to check out Somatic Exercises For Nervous System Regulation, and take care of yourself!
Share This Post
-
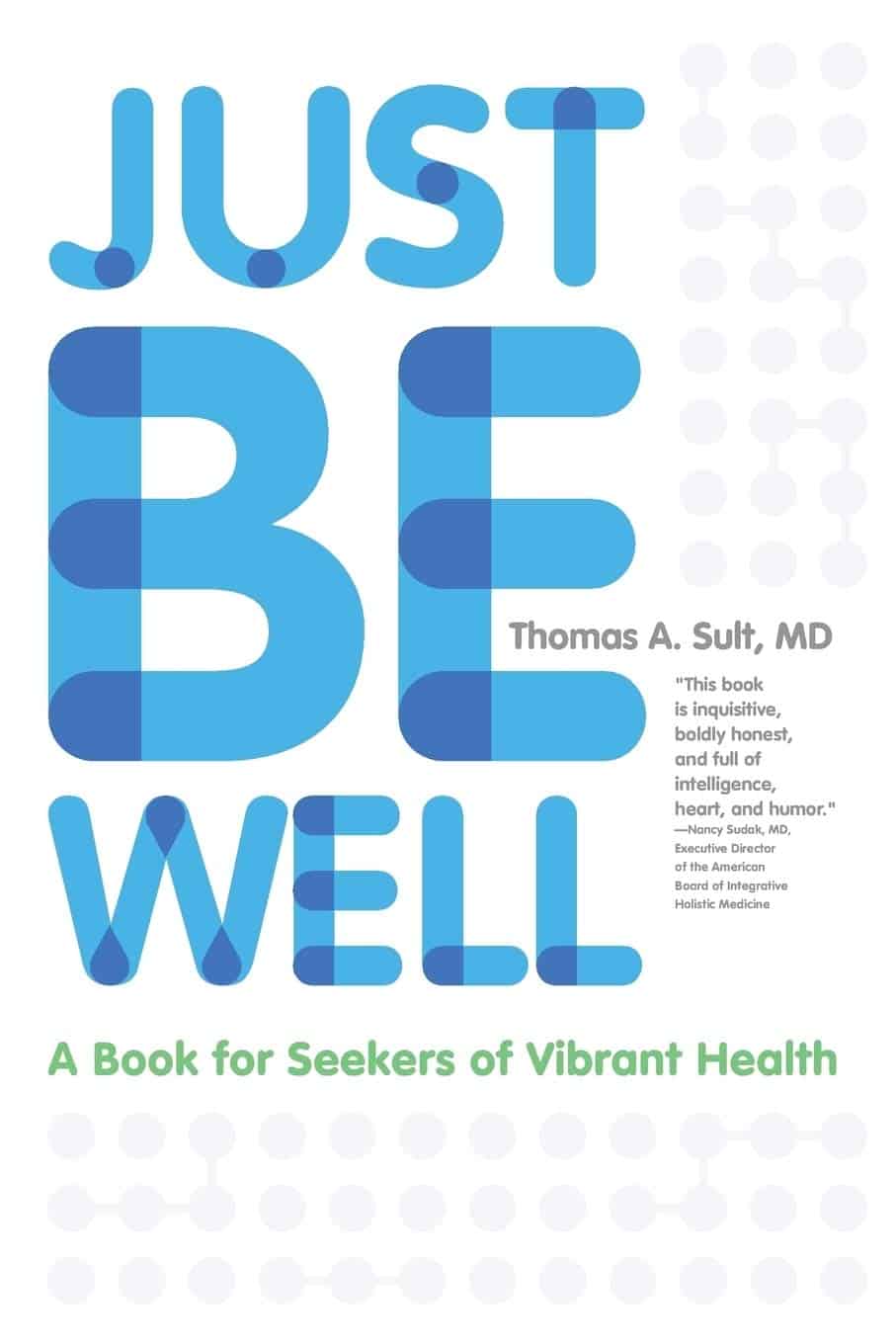
Just Be Well – by Dr. Thomas Sult
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Firstly, what this is not: a “think yourself well” book. It’s not about just deciding to be well.
Rather, it’s about ensuring the foundations of wellness, from which the rest of good health can spring, and notably, an absence of chronic illness. In essence: enjoying chronic good health.
The prescription here is functional medicine, which stands on the shoulders of lifestyle medicine. This latter is thus briefly covered and the basics presented, but most of the book is about identifying the root causes of disease and eliminating them one by one, by taking into account the functions of the body’s processes, both in terms of pathogenesis (and thus, seeking to undermine that) and in terms of correct functioning (i.e., good health).
While the main focus of the book is on health rather than disease, he does cover a number of very common chronic illnesses, and how even in those cases where they cannot yet be outright cured, there’s a lot more that can be done for them than “take two of these and call your insurance company in the morning”, when the goal is less about management of symptoms (though that is also covered) and more about undercutting causes, and ensuring that even if one thing goes wrong, it doesn’t bring the entire rest of the system down with it (something that often happens without functional medicine).
The style is clear, simple, and written for the layperson without unduly dumbing things down.
Bottom line: if you would like glowingly good health regardless of any potential setbacks, this book can help your body do what it needs to for you.
Share This Post
-
LGBTQ+ People Relive Old Traumas as They Age on Their Own
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Bill Hall, 71, has been fighting for his life for 38 years. These days, he’s feeling worn out.
Hall contracted HIV, the virus that can cause AIDS, in 1986. Since then, he’s battled depression, heart disease, diabetes, non-Hodgkin lymphoma, kidney cancer, and prostate cancer. This past year, Hall has been hospitalized five times with dangerous infections and life-threatening internal bleeding.
But that’s only part of what Hall, a gay man, has dealt with. Hall was born into the Tlingit tribe in a small fishing village in Alaska. He was separated from his family at age 9 and sent to a government boarding school. There, he told me, he endured years of bullying and sexual abuse that “killed my spirit.”
Because of the trauma, Hall said, he’s never been able to form an intimate relationship. He contracted HIV from anonymous sex at bath houses he used to visit. He lives alone in Seattle and has been on his own throughout his adult life.
“It’s really difficult to maintain a positive attitude when you’re going through so much,” said Hall, who works with Native American community organizations. “You become mentally exhausted.”
It’s a sentiment shared by many older LGBTQ+ adults — most of whom, like Hall, are trying to manage on their own.
Of the 3 million Americans over age 50 who identify as gay, bisexual, or transgender, about twice as many are single and living alone when compared with their heterosexual counterparts, according to the National Resource Center on LGBTQ+ Aging.
This slice of the older population is expanding rapidly. By 2030, the number of LGBTQ+ seniors is expected to double. Many won’t have partners and most won’t have children or grandchildren to help care for them, AARP research indicates.
They face a daunting array of problems, including higher-than-usual rates of anxiety and depression, chronic stress, disability, and chronic illnesses such as heart disease, according to numerous research studies. High rates of smoking, alcohol use, and drug use — all ways people try to cope with stress — contribute to poor health.
Keep in mind, this generation grew up at a time when every state outlawed same-sex relations and when the American Psychiatric Association identified homosexuality as a psychiatric disorder. Many were rejected by their families and their churches when they came out. Then, they endured the horrifying impact of the AIDS crisis.
“Dozens of people were dying every day,” Hall said. “Your life becomes going to support groups, going to visit friends in the hospital, going to funerals.”
It’s no wonder that LGBTQ+ seniors often withdraw socially and experience isolation more commonly than other older adults. “There was too much grief, too much anger, too much trauma — too many people were dying,” said Vincent Crisostomo, director of aging services for the San Francisco AIDS Foundation. “It was just too much to bear.”
In an AARP survey of 2,200 LGBTQ+ adults 45 or older this year, 48% said they felt isolated from others and 45% reported lacking companionship. Almost 80% reported being concerned about having adequate social support as they grow older.
Embracing aging isn’t easy for anyone, but it can be especially difficult for LGBTQ+ seniors who are long-term HIV survivors like Hall.
Related Links
- Americans With HIV Are Living Longer. Federal Spending Isn’t Keeping Up. Jun 17, 2024
- ‘Stonewall Generation’ Confronts Old Age, Sickness — And Discrimination May 22, 2019
- Staying Out Of The Closet In Old Age Oct 17, 2016
Of 1.2 million people living with HIV in the United States, about half are over age 50. By 2030, that’s estimated to rise to 70%.
Christopher Christensen, 72, of Palm Springs, California, has been HIV-positive since May 1981 and is deeply involved with local organizations serving HIV survivors. “A lot of people living with HIV never thought they’d grow old — or planned for it — because they thought they would die quickly,” Christensen said.
Jeff Berry is executive director of the Reunion Project, an alliance of long-term HIV survivors. “Here people are who survived the AIDS epidemic, and all these years later their health issues are getting worse and they’re losing their peers again,” Berry said. “And it’s triggering this post-traumatic stress that’s been underlying for many, many years. Yes, it’s part of getting older. But it’s very, very hard.”
Being on their own, without people who understand how the past is informing current challenges, can magnify those difficulties.
“Not having access to supports and services that are both LGBTQ-friendly and age-friendly is a real hardship for many,” said Christina DaCosta, chief experience officer at SAGE, the nation’s largest and oldest organization for older LGBTQ+ adults.
Diedra Nottingham, a 74-year-old gay woman, lives alone in a one-bedroom apartment in Stonewall House, an LGBTQ+-friendly elder housing complex in New York City. “I just don’t trust people,“ she said. “And I don’t want to get hurt, either, by the way people attack gay people.”
When I first spoke to Nottingham in 2022, she described a post-traumatic-stress-type reaction to so many people dying of covid-19 and the fear of becoming infected. This was a common reaction among older people who are gay, bisexual, or transgender and who bear psychological scars from the AIDS epidemic.
Nottingham was kicked out of her house by her mother at age 14 and spent the next four years on the streets. The only sibling she talks with regularly lives across the country in Seattle. Four partners whom she’d remained close with died in short order in 1999 and 2000, and her last partner passed away in 2003.
When I talked to her in September, Nottingham said she was benefiting from weekly therapy sessions and time spent with a volunteer “friendly visitor” arranged by SAGE. Yet she acknowledged: “I don’t like being by myself all the time the way I am. I’m lonely.”
Donald Bell, a 74-year-old gay Black man who is co-chair of the Illinois Commission on LGBTQ Aging, lives alone in a studio apartment in subsidized LGBTQ+-friendly senior housing in Chicago. He spent 30 years caring for two elderly parents who had serious health issues, while he was also a single father, raising two sons he adopted from a niece.
Bell has very little money, he said, because he left work as a higher-education administrator to care for his parents. “The cost of health care bankrupted us,” he said. (According to SAGE, one-third of older LGBTQ+ adults live at or below 200% of the federal poverty level.) He has hypertension, diabetes, heart disease, and nerve damage in his feet. These days, he walks with a cane.
To his great regret, Bell told me, he’s never had a long-term relationship. But he has several good friends in his building and in the city.
“Of course I experience loneliness,” Bell said when we spoke in June. “But the fact that I am a Black man who has lived to 74, that I have not been destroyed, that I have the sanctity of my own life and my own person is a victory and something for which I am grateful.”
Now he wants to be a model to younger gay men and accept aging rather than feeling stuck in the past. “My past is over,” Bell said, “and I must move on.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
Plum vs Persimmon – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing plum to persimmon, we picked the plum.
Why?
Looking at the macros first, persimmon has 3x the carbs for only the same amount of fiber, on account of which plum has the lower glycemic index, so we’ll go with plum here, though your opinion could vary.
In terms of vitamins, it’s much less subjective: plums have more of vitamins A, B1, B2, B3, B5, B6, B7, B9, E, K, and choline, while persimmon has more vitamin C. So, unless you have scurvy, plums will be the best choice for most people.
In the category of minerals, plums have more copper, magnesium, manganese, and zinc, while persimmon has more calcium, iron, phosphorus, and potassium—thus, a 4:4 tie on minerals.
Adding up the sections gives an overall win for plums, but of course, enjoy either or both; diversity is good!
PS: plums have an extra bonus too; check out the link below…
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer ← plums kill cancer cells while sparing healthy ones
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Plant vs Animal Protein
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Plant vs Animal Protein: Head to Head
Some people will obviously have strong ideological opinions here—for vegetarians and vegans, it’s no question, and for meat-eaters, it’s easy to be reactive to that and double-down on the bacon. But, we’re a health science newsletter, so we’ll be sticking to the science.
Which is better, healthwise?
First, it depends on how you go about it. Consider these options:
- A piece of salmon
- A steak
- A hot dog
- A hot dog, but plant-based
- Textured soy protein (no additives)
- Edamame (young soy) beans
Three animal-based protein sources, three plant-based. We could render the competition simple (but very unfair) by pitting the hotdog against the edamame beans, or the plant-based hot dog against the piece of salmon. So let’s kick this off by saying:
- There are good and bad animal-based protein sources
- There are good and bad plant-based protein sources
Whatever you choose, keep that in mind while you do. Less processed is better in either case. And if you do go for red meat, less is better, period.
Picking the healthiest from each, how do the nutritional profiles look?
They look good in both cases! One factor of importance is that in either case, our bodies will reduce the proteins we consume to their constituent amino acids, and then rebuild them into the specific proteins we actually need. Our bodies will do that regardless of the source, because we are neither a salmon nor a soybean, for example.
We need 20 specific amino acids, for our bodies to make the proteins we will use in our bodies. Of these, 9 are considered “essential”, meaning we cannot synthesize them and must get them from our diet,
Animal protein sources contain all 9 of those (just like we do). Plant based sources often don’t, individually, but by eating soy for example (which does contain them all) and/or getting multiple sources of protein from different plants, the 9 can be covered quite easily with little thought, just by having a varied diet.
Meats are #1!
- They’re number 1 for nutritional density
- They’re number 1 for health risks, too
So while plant-based diet adherents may need to consume more varied things to get all the nutrients necessary, meat-eaters won’t have that problem.
Meat-eaters will instead have a different problem, of more diet-related health risks, e.g.
- Cardiovascular disease
- Metabolic disorders
- Cancers
So again, if eating (especially processed and/or red) meat, moderation is good. The Mediterranean Diet that we so often recommend, by default contains small amounts of lean animal protein.
Which is better for building muscle?
Assuming a broadly healthy balanced diet, and getting sufficient protein from your chosen source, they’re pretty equal:
- Vegan and Omnivorous High Protein Diets Support Comparable Daily Myofibrillar Protein Synthesis Rates and Skeletal Muscle Hypertrophy in Young Adults
- A mycoprotein-based high-protein vegan diet supports equivalent daily myofibrillar protein synthesis rates compared with an isonitrogenous omnivorous diet in older adults: a randomised controlled trial
(both studies showed that both dietary approaches yielded results that showed no difference in muscle synthesis between the two)
The bottom line is…
Healthwise, what’s more important than whether you get your protein from animals or plants is that you eat foods that aren’t processed, and are varied.
And if you want to do a suped-up Mediterranean Diet with less red meat, you might want to try:
A Pesco-Mediterranean Diet With Intermittent Fasting: JACC Review Topic of the Week
^This is from a review in the Journal of the American College of Cardiology, and in few words, they recommend it very highly
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Low-Dose Aspirin & Anemia
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We recently wrote about…
How To Survive A Heart Attack When You’re Alone
…and one of the items was “if you have aspirin readily available, then after calling an ambulance is the time to take it—but don’t exert yourself trying to find some”.
But what of aspirin as a preventative?
Many people take low-dose aspirin daily as a way to reduce the risk of atherothrombosis specifically (and thus, indirectly, they hope to reduce the risk of heart attacks).
The science of how helpful this is both clear and complicated—that is to say, the stats are not ambiguous*, but there are complicating factors of which many people are unaware.
*it will reduce the overall risk of cardiovascular events, but will not affect CVD mortality; in other words, it may improve your recovery from minor cardiac events, but is not likely to save you from major ones.
And also, it has unwanted side effects that can constitute a more relevant threat for many people. We’ll share more on that at the end of today’s article, but first…
A newly identified threat from daily aspirin use
A large (n=313,508) study of older adults (median age 73) were sorted into those who used low-dose aspirin as a preventative, and those who did not.
The primary outcome was incidence of anemia sufficient to require treatment, and the secondary outcome was major bleeding. And, at least 1 in 5 of those who experienced anemia also experienced bleeding.
The bleeding issue was not “newly identified” and will not surprise many people; after all, the very reason that aspirin is taken as a CVD preventative is for its anti-clotting property of allowing blood to flow more freely.
The anemia, however, has been getting increasing scientific scrutiny lately, after long going unnoticed in the wild. Given that anemia also gives the symptom “dizziness”, this is also a significant threat for increasing the incidence of falls in the older population, too, which can of course lead to serious complications and ultimately death.
Here’s the paper itself:
Want to know more?
As promised, here’s what we wrote previously about some of aspirin’s other risks:
Aspirin, CVD Risk, & Potential Counter-Risks
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: