Food Expiration Dates Don’t Mean What Most People Think They Mean
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Have you ever wondered why rock salt that formed during the Precambrian era has a label on it saying that it expires next month? To take something more delicate, how about eggs that expire next Thursday; isn’t that oddly specific for something that is surely affected by many variables? What matters, and what doesn’t?
Covering their assets
The US in particular wastes huge amounts of food, with 37% of food waste coming from households. Confusion over date labels is a major contributor, accounting for 20% of household food waste. Many people misinterpret these labels, often discarding food that is still safe to eat—which is good for the companies selling the food, because then they get to sell you more.
Date labels were introduced in the 70s with the “open dating” system to indicate optimal freshness, not safety. These dates are often conservative, set by manufacturers to ensure food is consumed at its best quality and encourage repeat purchases. However, many foods remain safe well past their labeled dates, including shelf-stable items like pasta, rice, and canned goods, as well as frozen foods stored properly.
Some foods do pose safety risks, especially meat and dairy products, as well as many grain-based foods, all of which which can harbor harmful bacteria. Infant formula labels are strictly regulated for safety. However, most date labels are not linked to health risks, leading to unnecessary waste.
When it comes down to it, our senses of sight, smell, and taste are more reliable than dates on packaging. Some quick pointers and caveats:
- If it has changed color in some way that’s not associated with a healthily ripening fruit or vegetable, that’s probably bad
- If it is moldy, that’s probably bad (but the degree of badness varies from food to food; see the link beneath today’s video for more on that)
- If a container has developed droplets of water on the inside when it didn’t have those before, that’s probably bad (it means something is respiring, and is thus alive, that probably shouldn’t be)
- If it smells bad, that’s probably bad—however this is not a good safety test, because a bad smell may often mean you are inhaling mold spores, which are not good for your lungs.
- If it tastes different than that food usually does, that’s probably bad (especially if it became bitter, pungent, tangy, sour, or cheesy, and does nor normally taste that way).
Some places have trialled clearer labelling, for example a distinction between “expires” and merely “best before”, but public awareness about the distinction is low. Some places have trialled removing dates entirely, to oblige the consumer to use their own senses instead. This is good for the seller in a different way than household food waste is, because it means the seller will have less in-store waste (because they can still sell something that might previously have been labelled as expired).
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Broccoli vs Cabbage – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing broccoli to cabbage, we picked the broccoli.
Why?
Here we go once again pitting two different cultivars of the same species (Brassica oleracea) against each other, and/but once again, there is one that comes out as nutritionally best.
In terms of macros, broccoli has more protein, carbs, and fiber, while they are both low glycemic index foods. The differences are small though, so it’s fairest to call this category a tie.
When it comes to vitamins, broccoli has more of vitamins A, B1, B2, B3, B5, B6, B7, B9, C, E, K, and choline, while cabbage is not higher in any vitamins. It should be noted that cabbage is still good for these, especially vitamins C and K, but broccoli is simply better.
In the category of minerals, broccoli has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while cabbage is not higher in any minerals. Again though, cabbage is still good, especially in calcium, iron, and manganese, but again, broccoli is simply better.
Of course, enjoy either or both! But if you want the nutritionally densest option, it’s broccoli.
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Take care!
Share This Post
-
The Sleep Solution – by Dr. Chris Winter
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book’s blurb contains a bold claim:
❝If you want to fix your sleep problems, Internet tips and tricks aren’t going to do it for you. You need to really understand what’s going on with your sleep—both what your problems are and how to solve them.❞
So, how well does it deliver, on the strength of being a whole book rather than an Internet article?
Well, for sure we wouldn’t have the room to include all the information that Dr. Winter does, in one of our main feature articles here (we’d need to spread it out over several weeks, at least).
He examines very thoroughly what is going on with sleep, sleep disturbance, and sleep deprivation. What’s going on with the different phases of sleep (far more than your phone’s sleep app will), and how imbalances in these can cause problems.
While the usual sleep hygiene tips do get a mention, he broadly assumes we know that part already. Instead, he focuses on aligning as many components as possible of our rich and interesting circadian rhythm. Yes, even if that means clawing our way out of insomnia and/or a bad sleep schedule (or lack of coherent sleep schedule) first. He gives plenty of practical advice on how to do that.
Bottom line: if you’d like to more deeply understand sleep, what is or isn’t wrong with yours, and how you can fix it, this book is a great resource.
Click here to check out The Sleep Solution, and enjoy the benefits of better rest!
Share This Post
-
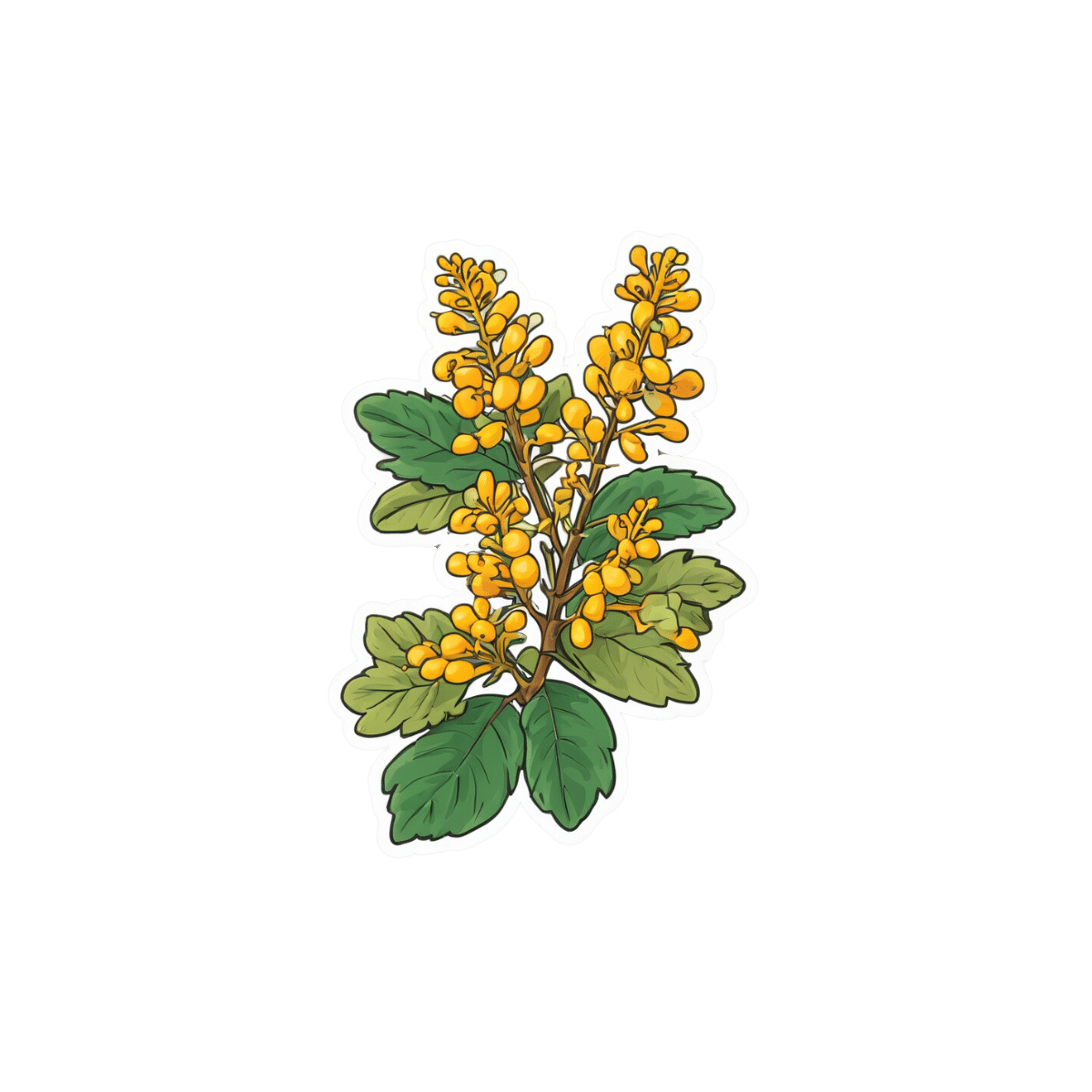
Take These To Lower Cholesterol! (Statin Alternatives)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Ada Ozoh, a diabetes specialist, took an interest in this upon noting the many-headed beast that is metabolic syndrome means that neither diabetes nor cardiovascular disease exist in a vacuum, and there are some things that can help a lot against both. Here she shares some of her top recommendations:
Statin-free options
Dr. Ozoh recommends:
- Bergamot: lowers LDL (“bad” cholesterol) by about 30% and slightly increases HDL (“good” cholesterol), at 500–1000mg/day, seeing results in 1–6 months
- Berberine: prevents fat absorption and helps burn stored fat, as well as reducing blood sugar levels and blood pressure, at 1,500mg/day
- Silymarin: protects the liver, and lowers cholesterol in type 2 diabetes, at 280–420mg/day
- Phytosterols: lower cholesterol by about 10%; found naturally in many plants, but it takes supplementation to read the needed (for this purpose) dosage of 2g/day
- Red yeast rice: this is white rice fermented with yeast, and it lowers LDL cholesterol by about 25%, seeing results in around 3 months
For more information on all of the above (including more details on the biochemistry, as well as potential issues to be aware of), enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Statins: His & Hers? Very Different For Men & Women
- Berberine For Metabolic Health
- Milk Thistle For The Brain, Bones, & More ← this is about silymarin, which is extracted from Silybum marianum, the milk thistle plant
Take care!
Share This Post
Related Posts
-
The Four Pillar Plan – by Dr. Rangan Chatterjee
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Rangan Chatterjee, a medical doctor, felt frustrated with how many doctors in his field focus on treating the symptoms of disease, rather than the cause. Sometimes, of course, treating the symptom is necessary too! But neglecting the cause is a recipe for long-term woes.
What he does differently is take lifestyle as a foundation, and even that, he does differently than many authors on the topic. How so, you may wonder?
Rather than look first at exercise and diet, he starts with “relax”. His rationale is reasonable: diving straight in with marathon training or a whole new diet plan can be unsustainable without this as a foundation to fall back on.
Many sources look first at exercise (because it can be a very simple “prescription”) before diet (often more complex)… but how does one exercise well with the wrong fuel in the tank? So Dr. Chatterjee’s titular “Four Pillars” come in the following order:
- Relax
- Eat
- Move
- Sleep
He also goes for “move” rather than “exercise” as the focus here is more on minimizing time spent sitting, and thus involving a lot of much more frequent gentle activities… rather than intensive training programs and the like.
And as for sleep? Yes, that comes last because—no matter how important it is—the other things are easier to directly control. After all, one can improve conditions for sleep, but one cannot simply choose to sleep better! So with the other three things covered first, good sleep is the fourth and final thing to fall into place.
All in all, this is a great book to cut through the catch-22 problem of lifestyle factors negatively impacting each other.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Banana vs Goji Berries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing banana to goji berries, we picked the goji berries.
Why?
Both are great! But…
In terms of macros, goji berries have much more fiber, carbs, and protein, thus making it the most nutrient-dense option, as we might expect from a dried fruit being compared to a non-dried fruit—since the non-dried fruit has water weight that the dried fruit doesn’t, its percentages of other things will be proportionally lower, because the percentages must still add up to 100%, and if 75% is water (as is the case for bananas, compared to goji berries’ 7.5% water), then that only leaves 25% to work with, while goji berries have 92.5% to work with. In short, an easy and expected win for goji berries.
In the category of vitamins, bananas have more of vitamin B6, while goji berries have more of vitamins A, B1, B3, B5, B9, C, E, and K. A clear win for goji berries.
When it comes to minerals, bananas are not higher in any minerals, while goji berries have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. Another easy win for goji berries.
As for polyphenols, you may well imagine that the brightly-colored bitter-tasting berries have more, and you’d be right; you can read more about the exciting phytochemical properties of goji berries in the links below.
Meanwhile, adding up the sections show a clear overall win for goji berries, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
- The Top Micronutrient Deficiency In High Blood Pressure ← it’s potassium, and because of some popular mentions in TV shows, people get hung up on bananas being a good source of potassium. Which they are, but they’re not even in the top 10 of fruits for potassium. Here’s a non-exhaustive list of fruits that have more potassium than bananas, portion for portion
- Goji Berries: Which Benefits Do They Really Have? ← many!
- The Sugary Food That Lowers Blood Sugars ← it’s goji berries!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The BAT-pause!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Cold Weather & The Menopause Battle It Out
You may know that (moderate, safe) exposure to the cold allows our body to convert our white and yellow fat into the much healthier brown fat—also called brown adipose tissue, or “BAT” to its friends.
If you didn’t already know that, then well, neither did scientists until about 15 years ago:
The Changed Metabolic World with Human Brown Adipose Tissue: Therapeutic Visions
You can read more about it here:
Cool Temperature Alters Human Fat and Metabolism
This is important, especially because the white fat that gets converted is the kind that makes up most visceral fat—the kind most associated with all-cause mortality:
Visceral Belly Fat & How To Lose It ← this is not the same as your subcutaneous fat, the kind that sits directly under your skin and keeps you warm; this is the fat that goes between your organs and of which we should only have a small amount!
The BAT-pause
It’s been known (since before the above discovery) that BAT production slows considerably as we get older. Not too shocking—after all, many metabolic functions slow as we get older, so why should fat regulation be any different?
But! Rodent studies found that this was tied less to age, but to ovarian function: rats who underwent ovariectomies suffered reduced BAT production, regardless of their age.
Naturally, it’s been difficult to recreate such studies in humans, because it’s difficult to find a large sample of young adults willing to have their ovaries whipped out (or even suppressed chemically) to see how badly their metabolism suffers as a result.
Nor can an observational study (for example, of people who incidentally have ovaries removed due to ovarian cancer) usefully be undertaken, because then the cancer itself and any additional cancer treatments would be confounding factors.
Perimenopausal study to the rescue!
A recent (published last month, at time of writing!) study looked at women around the age of menopause, but specifically in cohorts before and after, measuring BAT metabolism.
By dividing the participants into groups based on age and menopausal status, and dividing the post-menopausal group into “takes HRT” and “no HRT” groups, and dividing the pre-menopausal group into “normal ovarian function” and “ovarian production of estrogen suppressed to mimic slightly early menopause” groups (there’s a drug for that), and then having groups exposed to warm and cold temperatures, and measuring BAT metabolism in all cases, they were able to find…
It is about estrogen, not age!
You can read more about the study here:
“Good” fat metabolism changes tied to estrogen loss, not necessarily to aging, shows study
…and the study itself, here:
Brown adipose tissue metabolism in women is dependent on ovarian status
What does this mean for men?
This means nothing directly for (cis) men, sorry.
But to satisfy your likely curiosity: yes, testosterone does at least moderately suppress BAT metabolism—based on rodent studies, anyway, because again it’s difficult to find enough human volunteers willing to have their testicles removed for science (without there being other confounding variables in play, anyway):
Testosterone reduces metabolic brown fat activity in male mice
So, that’s bad per se, but there isn’t much to be done about it, since the rest of your (addressing our male readers here) metabolism runs on testosterone, as do many of your bodily functions, and you would suffer many unwanted effects without it.
However, as men do typically have notably less body fat in general than women (this is regulated by hormones), the effects of changes in BAT metabolism are rather less pronounced in men (per testosterone level changes) than in women (per estrogen level changes), because there’s less overall fat to convert.
In summary…
While menopausal HRT is not necessarily a silver bullet to all metabolic problems, its BAT-maintaining ability is certainly one more thing in its favor.
See also:
Dr. Jen Gunter | What You Should Have Been Told About The Menopause Beforehand
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: