Fast Exercise – by Dr. Michael Mosley & Peta Bee
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about the benefits of High-Intensity Interval Training (HIIT), but there’s more to say than we can fit in a short article!
Dr. Michael Mosley, who hates exercise but knows his stuff when it comes to the benefits, teamed up with Peta Bee, who loves exercise and is a science journalist with degrees in sports science and nutrition, to bring us this book.
In it, we learn a lot about:
- the science of HIIT
- what makes it so different from most kinds of exercise
- exactly what benefits one can expect
…in a very detailed clinical fashion (while still remaining very readable).
By “very detailed clinical fashion”, here we mean “one minute of this kind of exercise this many times per week over this period of time will give this many extra healthy life-years”, for example, along with lots of research to back numbers, and explanations of the mechanisms of action (e.g. reducing inflammatory biomarkers of aging, increasing cellular apoptosis, improving cardiometabolic stats for reduced CVD risk, and many things)
There’s also time/space given over to exactly what to do and how to do it, giving enough options to suit personal tastes/circumstances.
Bottom line: if you’d like to make your exercise work a lot harder for you while you spend a lot less time working out, then this book will help you do just that!
Click here to check out Fast Exercise, and enjoy the benefits!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What I Wish People Knew About Dementia – by Dr. Wendy Mitchell
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We hear a lot from doctors who work with dementia patients; sometimes we hear from carers too. In this case, the author spent 20 years working for the NHS, before being diagnosed with young-onset dementia, at the age of 58. Like many health industry workers who got a life-changing diagnosis, she quickly found it wasn’t fun being on the other side of things, and vowed to spend her time researching, and raising awareness about, dementia.
Many people assume that once a person has dementia, they’re basically “gone before they’re gone”, which can rapidly become a self-fulfilling prophecy as that person finds themself isolated and—though this word isn’t usually used—objectified. Talked over, viewed (and treated) more as a problem than a person. Cared for hopefully, but again, often more as a patient than a person. If doctors struggle to find the time for the human side of things with most patients most of the time, this is only accentuated when someone needs more time and patience than average.
Instead, Dr. Mitchell—an honorary doctorate, by the way, awarded for her research—writes about what it’s actually like to be a human with dementia. Everything from her senses, how she eats, the experience of eating in care homes, the process of boiling an egg… To relationships, how care changes them, to the challenges of living alone. And communication, confusion, criticism, the language used by professionals, or how things are misrepresented in popular media. She also talks about the shifting sense of self, and brings it all together with gritty optimism.
The style is deeply personal, yet lucid and clear. While dementia is most strongly associated with memory loss and communication problems, this hasn’t affected her ability to write well (7 years into her diagnosis, in case you were wondering).
Bottom line: if you’d like to read a first-person view of dementia, then this is an excellent opportunity to understand it from the view of, as the subtitle goes, someone who knows.
Click here to check out What I Wish People Knew About Dementia, and then know those things!
Share This Post
-
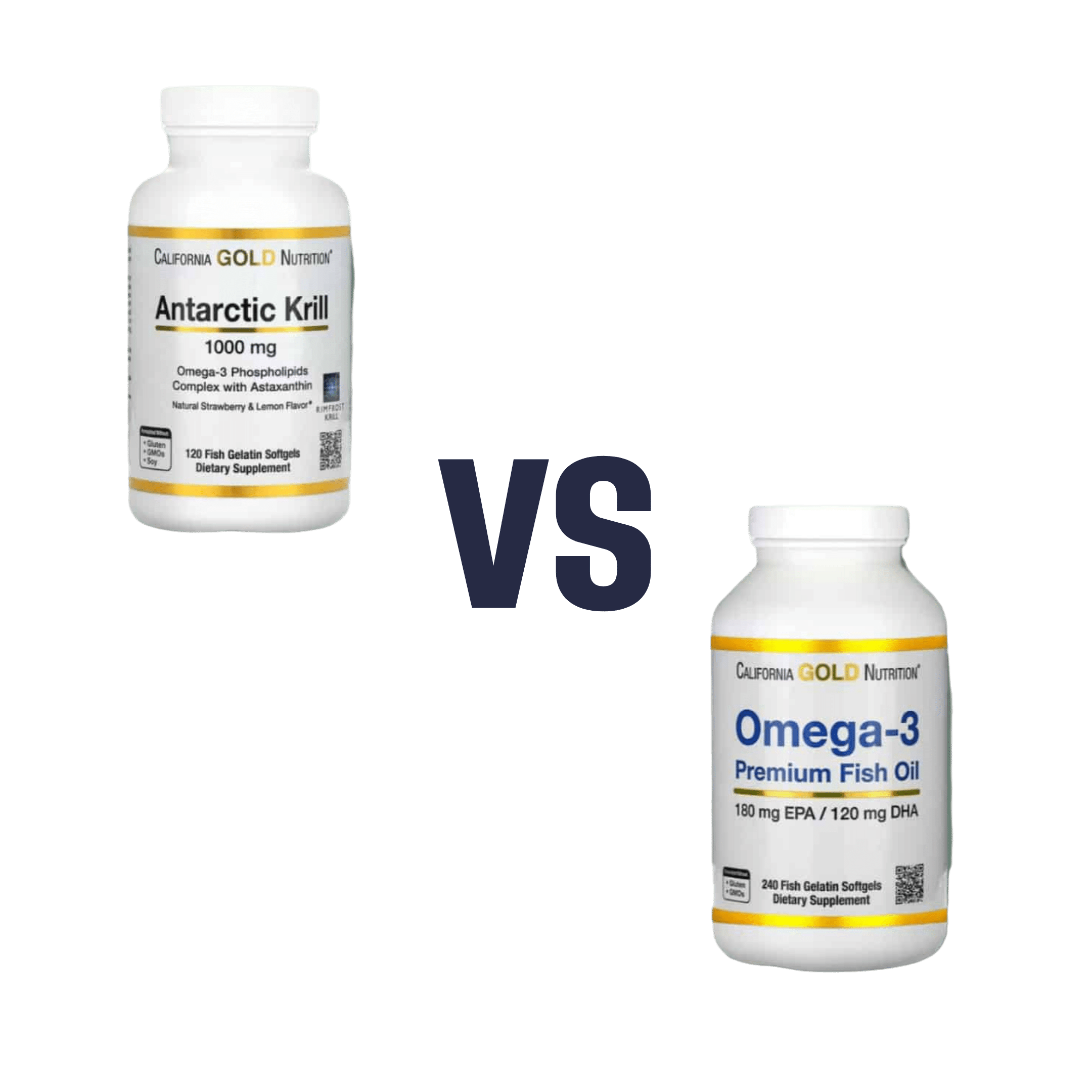
Krill Oil vs Fish Oil – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing krill oil to fish oil, we picked the krill oil.
Why?
Both of these products are good sources of omega-3 fatty acids EPA and DHA, and for the specific brand depicted above, in both cases 2 softgels will give you the recommended daily amount (which is generally held to be 250–500mg combined omega-3s per day).
This brand’s fish oil gives more (640mg combined omega-3s per 2 softgels, to the same brand’s krill oil’s 480mg per 2 softgels), but since the krill oil is already in the high end of RDA territory, the excess beyond the RDA is not helpful, and not a huge factor. More quantity is not always better, when the body can only process so much at a time.
However, the krill oil gives some extra things that the fish oil doesn’t:
- Astaxanthin, a “super-antioxidant”
- and neuroprotectant, heart-healthy phospholipids
Additional considerations
We have declared “the winner” based on health considerations only. That’s a sticking point for us in all our writings; we’ll occasionally look at and mention other factors, but we know that health is what you’re here for, so that’s what we’ll always treat as most critical.
However, in case these factors may interest you and/or influence you to one or the other:
• The fish oil is about 30% cheaper financially
• The krill oil is a lot more sustainable environmentallyBack to the health science…
Read more:
• What Omega-3 Fatty Acids Really Do For Us
• Astaxanthin: Super-Antioxidant & NeuroprotectantWant some? Here for your convenience are some example products on Amazon:
(brands available will vary per region, but now you know what to look out for on the labels!)
Share This Post
-
Beetroot vs Cucumber – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing beetroot to cucumber, we picked the beetroot.
Why?
While they’re both mostly-water vegetables that can go in salads, soups, and sauces, they have some notable differences:
In terms of macros, beetroot has nearly 3x the carbs and/but also nearly 6x the fiber, so we say beetroot wins this category.
On the vitamins front, beetroot has more of vitamins B1, B2, B3, B6, B7, B9, C, and E, while cucumber has more of vitamins A, B5, and K. In short, a clear win for beetroot.
In the category of minerals, beetroot has more copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while cucumber is not richer in any minerals.
When it comes to beneficial phytochemicals, both have good things to offer, though we say beetroot has more. Notably, cucumber extract beats glucosamine and chondroitin for reducing joint inflammation, at 1/135th of the dose. On the other hand, beetroot’s phytochemical benefits are so numerous we’ll not list them here, and just recommend checking out the link below!
In short, a win in all categories for beetroot, but cucumbers are great too, so by all means enjoy either or both!
Want to learn more?
You might like to read:
Beetroot For More Than Just Your Blood Pressure
Enjoy!
Share This Post
Related Posts
-
Regular Nail Polish vs Gel Nail Polish – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing regular nail polish to gel nail polish, we picked the regular.
Why?
This one’s less about what’s in the bottle, and more about what gets done to your hands:
- Regular nail polish application involves carefully brushing it on.
- Regular nail polish removal involves wiping with acetone.
…whereas:
- Gel nail polish application involves deliberately damaging (roughing up) the nail to allow the color coat to adhere, then when the top coat is applied, holding the nails (and thus, the attached fingers) under a UV light to set it. That UV lamp exposure is very bad for the skin.
- Gel nail polish removal involves soaking in acetone, which is definitely worse than wiping with acetone. Failure to adequately soak it will result in further damage to the nail while trying to get the base coat off the nail that you already deliberately damaged when first applying it.
All in all, regular nail polish isn’t amazing for nail health (healthiest is for nails to be free and naked), but for those of us who like a little bit of color there, regular is a lot better than gel.
Gel nail polish damages the nail itself by necessity, and presents a cumulative skin cancer risk and accelerated aging of the skin, by way of the UV lamp use.
For your interest, here are the specific products that we compared, but the above goes for any of this kind:
Regular nail polish | Gel nail polish
If you’d like to read more about nail health, you might enjoy reading:
The Counterintuitive Dos and Don’ts of Nail Health
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Pain Clinics Made Millions From ‘Unnecessary’ Injections Into ‘Human Pin Cushions’
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
McMINNVILLE, Tenn. — Each month, Michelle Shaw went to a pain clinic to get the shots that made her back feel worse — so she could get the pills that made her back feel better.
Shaw, 56, who has been dependent on opioid painkillers since she injured her back in a fall a decade ago, said in both an interview with KFF Health News and in sworn courtroom testimony that the Tennessee clinic would write the prescriptions only if she first agreed to receive three or four “very painful” injections of another medicine along her spine.
The clinic claimed the injections were steroids that would relieve her pain, Shaw said, but with each shot her agony would grow. Shaw said she eventually tried to decline the shots, then the clinic issued an ultimatum: Take the injections or get her painkillers somewhere else.
“I had nowhere else to go at the time,” Shaw testified, according to a federal court transcript. “I was stuck.”
Shaw was among thousands of patients of Pain MD, a multistate pain management company that was once among the nation’s most prolific users of what it referred to as “tendon origin injections,” which normally inject a single dose of steroids to relieve stiff or painful joints. As many doctors were scaling back their use of prescription painkillers due to the opioid crisis, Pain MD paired opioids with monthly injections into patients’ backs, claiming the shots could ease pain and potentially lessen reliance on painkillers, according to federal court documents.
Now, years later, Pain MD’s injections have been proved in court to be part of a decade-long fraud scheme that made millions by capitalizing on patients’ dependence on opioids. The Department of Justice has successfully argued at trial that Pain MD’s “unnecessary and expensive injections” were largely ineffective because they targeted the wrong body part, contained short-lived numbing medications but no steroids, and appeared to be based on test shots given to cadavers — people who felt neither pain nor relief because they were dead.
Four Pain MD employees have pleaded guilty or been convicted of health care fraud, including company president Michael Kestner, who was found guilty of 13 felonies at an October trial in Nashville, Tennessee. According to a transcript from Kestner’s trial that became public in December, witnesses testified that the company documented giving patients about 700,000 total injections over about eight years and said some patients got as many as 24 shots at once.
“The defendant, Michael Kestner, found out about an injection that could be billed a lot and paid well,” said federal prosecutor James V. Hayes as the trial began, according to the transcript. “And they turned some patients into human pin cushions.”
The Department of Justice declined to comment for this article. Kestner’s attorneys either declined to comment or did not respond to requests for an interview. At trial, Kestner’s attorneys argued that he was a well-intentioned businessman who wanted to run pain clinics that offered more than just pills. He is scheduled to be sentenced on April 21 in a federal court in Nashville.
According to the transcript of Kestner’s trial, Shaw and three other former patients testified that Pain MD’s injections did not ease their pain and sometimes made it worse. The patients said they tolerated the shots only so Pain MD wouldn’t cut off their prescriptions, without which they might have spiraled into withdrawal.
“They told me that if I didn’t take the shots — because I said they didn’t help — I would not get my medication,” testified Patricia McNeil, a former patient in Tennessee, according to the trial transcript. “I took the shots to get my medication.”
In her interview with KFF Health News, Shaw said that often she would arrive at the Pain MD clinic walking with a cane but would leave in a wheelchair because the injections left her in too much pain to walk.
“That was the pain clinic that was supposed to be helping me,” Shaw said in her interview. “I would come home crying. It just felt like they were using me.”
‘Not Actually Injections Into Tendons at All’
Pain MD, which sometimes operated under the name Mid-South Pain Management, ran as many as 20 clinics in Tennessee, Virginia, and North Carolina throughout much of the 2010s. Some clinics averaged more than 12 injections per patient each month, and at least two patients each received more than 500 shots in total, according to federal court documents.
All those injections added up. According to Medicare data filed in federal court, Pain MD and Mid-South Pain Management billed Medicare for more than 290,000 “tendon origin injections” from January 2010 to May 2018, which is about seven times that of any other Medicare biller in the U.S. over the same period.
Tens of thousands of additional injections were billed to Medicaid and Tricare during those same years, according to federal court documents. Pain MD billed these government programs for about $111 per injection and collected more than $5 million from the government for the shots, according to the court documents.
More injections were billed to private insurance too. Christy Wallace, an audit manager for BlueCross BlueShield of Tennessee, testified that Pain MD billed the insurance company about $40 million for more than 380,000 injections from January 2010 to March 2013. BlueCross paid out about $7 million before it cut off Pain MD, Wallace said.
These kinds of enormous billing allegations are not uncommon in health care fraud cases, in which fraudsters sometimes find a legitimate treatment that insurance will pay for and then overuse it to the point of absurdity, said Don Cochran, a former U.S. attorney for the Middle District of Tennessee.
Tennessee alone has seen fraud allegations for unnecessary billing of urine testing, skin creams, and other injections in just the past decade. Federal authorities have also investigated an alleged fraud scheme involving a Tennessee company and hundreds of thousands of catheters billed to Medicare, according to The Washington Post, citing anonymous sources.
Cochran said the Pain MD case felt especially “nefarious” because it used opioids to make patients play along.
“A scheme where you get Medicare or Medicaid money to provide a medically unnecessary treatment is always going to be out there,” Cochran said. “The opioid piece just gives you a universe of compliant people who are not going to question what you are doing.”
“It was only opioids that made those folks come back,” he said.
The allegations against Pain MD became public in 2018 when Cochran and the Department of Justice filed a civil lawsuit against the company, Kestner, and several associated clinics, alleging that Pain MD defrauded taxpayers and government insurance programs by billing for “tendon origin injections” that were “not actually injections into tendons at all.”
Kestner, Pain MD, and several associated clinics have each denied all allegations in that lawsuit, which is ongoing.Scott Kreiner, an expert on spine care and pain medicine who testified at Kestner’s criminal trial, said that true tendon origin injections (or TOIs) typically are used to treat inflamed joints, like the condition known as “tennis elbow,” by injecting steroids or platelet-rich plasma into a tendon. Kreiner said most patients need only one shot at a time, according to the transcript.
But Pain MD made repeated injections into patients’ backs that contained only lidocaine or Marcaine, which are anesthetic medications that cause numbness for mere hours, Kreiner testified. Pain MD also used needles that were often too short to reach back tendons, Kreiner said, and there was no imaging technology used to aim the needle anyway. Kreiner said he didn’t find any injections in Pain MD’s records that appeared medically necessary, and even if they had been, no one could need so many.
“I simply cannot fathom a scenario where the sheer quantity of TOIs that I observed in the patient records would ever be medically necessary,” Kreiner said, according to the trial transcript. “This is not even a close call.”
Jonathan White, a physician assistant who administered injections at Pain MD and trained other employees to do so, then later testified against Kestner as part of a plea deal, said at trial that he believed Pain MD’s injection technique was based on a “cadaveric investigation.”
According to the trial transcript, White said that while working at Pain MD he realized he could find no medical research that supported performing tendon origin injections on patients’ backs instead of their joints. When he asked if Pain MD had any such research, White said, an employee responded with a two-paragraph letter from a Tennessee anatomy professor — not a medical doctor — that said it was possible to reach the region of back tendons in a cadaver by injecting “within two fingerbreadths” of the spine. This process was “exactly the procedure” that was taught at Pain MD, White said.
During his own testimony, Kreiner said it was “potentially dangerous” to inject a patient as described in the letter, which should not have been used to justify medical care.
“This was done on a dead person,” Kreiner said, according to the trial transcript. “So the letter says nothing about how effective the treatment is.”
Over-Injecting ‘Killed My Hand’
Pain MD collapsed into bankruptcy in 2019, leaving some patients unable to get new prescriptions because their medical records were stuck in locked storage units, according to federal court records.
At the time, Pain MD defended the injections and its practice of discharging patients who declined the shots. When a former patient publicly accused the company of treating his back “like a dartboard,” Pain MD filed a defamation lawsuit, then dropped the suit about a month later.
“These are interventional clinics, so that’s what they offer,” Jay Bowen, a then-attorney for Pain MD, told The Tennessean newspaper in 2019. “If you don’t want to consider acupuncture, don’t go to an acupuncture clinic. If you don’t want to buy shoes, don’t go to a shoe store.”
Kestner’s trial told another story. According to the trial transcript, eight former Pain MD medical providers testified that the driving force behind Pain MD’s injections was Kestner himself, who is not a medical professional and yet regularly pressured employees to give more shots.
One nurse practitioner testified that she received emails “every single workday” pushing for more injections. Others said Kestner openly ranked employees by their injection rates, and implied that those who ranked low might be fired.
“He told me that if I had to feed my family based on my productivity, that they would starve,” testified Amanda Fryer, a nurse practitioner who was not charged with any crime.
Brian Richey, a former Pain MD nurse practitioner who at times led the company’s injection rankings, and has since taken a plea deal that required him to testify in court, said at the trial that he “performed so many injections” that his hand became chronically inflamed and required surgery.
“‘Over injecting killed my hand,’” Richey said on the witness stand, reading a text message he sent to another Pain MD employee in 2017, according to the trial transcript. “‘I was in so much pain Injecting people that didnt want it but took it to stay a patient.’”
“Why would they want to stay there?” a prosecutor asked.
“To keep getting their narcotics,” Richey responded, according to the trial transcript.
Throughout the trial, defense attorney Peter Strianse argued that Pain MD’s focus on injections was a result of Kestner’s “obsession” with ensuring that the company “would never be called a pill mill.”
Strianse said that Kestner “stayed up at night worrying” about patients coming to clinics only to get opioid prescriptions, so he pushed his employees to administer injections, too.
“Employers motivating employees is not a crime,” Strianse said at closing arguments, according to the court transcript. “We get pushed every day to perform. It’s not fraud; it’s a fact of life.”
Prosecutors insisted that this defense rang hollow. During the trial, former employees had testified that most patients’ opioid dosages remained steady or increased while at Pain MD, and that the clinics did not taper off the painkillers no matter how many injections were given.
“Giving them injections does not fix the pill mill problem,” federal prosecutor Katherine Payerle said during closing arguments, according to the trial transcript. “The way to fix being a pill mill is to stop giving the drugs or taper the drugs.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Hearing voices is common and can be distressing. Virtual reality might help us meet and ‘treat’ them
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Have you ever heard something that others cannot – such as your name being called? Hearing voices or other noises that aren’t there is very common. About 10% of people report experiencing auditory hallucinations at some point in their life.
The experience of hearing voices can be very different from person to person, and can change over time. They might be the voice of someone familiar or unknown. There might be many voices, or just one or two. They can be loud or quiet like a whisper.
For some people these experiences are positive. They might represent a spiritual or supernatural experience they welcome or a comforting presence. But for others these experiences are distressing. Voices can be intrusive, negative, critical or threatening. Difficult voices can make a person feel worried, frightened, embarrassed or frustrated. They can also make it hard to concentrate, be around other people and get in the way of day-to-day activities.
Although not everyone who hears voices has a mental health problem, these experiences are much more common in people who do. They have been considered a hallmark symptom of schizophrenia, which affects about 24 million people worldwide.
However, such experiences are also common in other mental health problems, particularly in mood- and trauma-related disorders (such as bipolar disorder or depression and post-traumatic stress disorder) where as many as half of people may experience them.
Rawpixel/Shutterstock Why do people hear voices?
It is unclear exactly why people hear voices but exposure to prolonged stress, trauma or depression can increase the chances.
Some research suggests people who hear voices might have brains that are “wired” differently, particularly between the hearing and speaking parts of the brain. This may mean parts of our inner speech can be experienced as external voices. So, having the thought “you are useless” when something goes wrong might be experienced as an external person speaking the words.
Other research suggests it may relate to how our brains use past experiences as a template to make sense of and make predictions about the world. Sometimes those templates can be so strong they lead to errors in how we experience what is going on around us, including hearing things our brain is “expecting” rather than what is really happening.
What is clear is that when people tell us they are hearing voices, they really are! Their brain perceives voice experiences as if someone were talking in the room. We could think of this “mistake” as working a bit like being susceptible to common optical tricks or visual illusions.
There may be differences in the brains of people who hear voices. Triff/Shutterstock Coping with hearing voices
When hearing voices is getting in the way of life, treatment guidelines recommend the use of medications. But roughly a third of people will experience ongoing distress. As such, treatment guidelines also recommend the use of psychological therapies such as cognitive behavioural therapy.
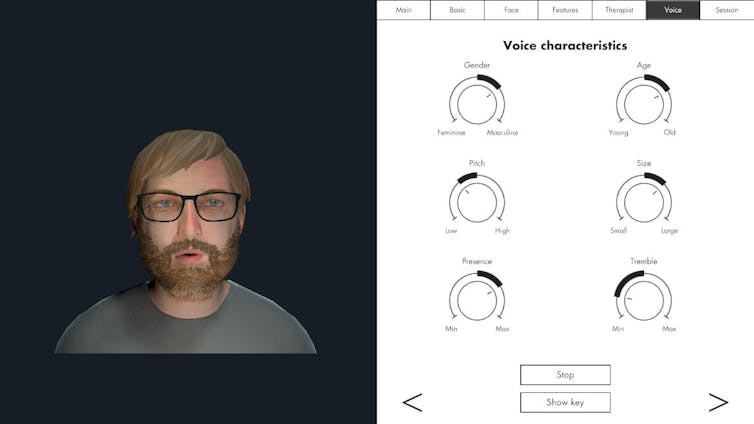
The next generation of psychological therapies are beginning to use digital technologies and virtual reality offers a promising new medium.
Avatar therapy allows a person to create a virtual representation of the voice or voices, which looks and sounds like what they are experiencing. This can help people regain power in the “relationship” as they interact with the voice character, supported by a therapist.
Jason’s experience
Aged 53, Jason (not his real name) had struggled with persistent voices since his early 20s. Antipsychotic medication had helped him to some extent over the years, but he was still living with distressing voices. Jason tried out avatar therapy as part of a research trial.
He was initially unable to stand up to the voices, but he slowly gained confidence and tested out different ways of responding to the avatar and voices with his therapist’s support.
Jason became more able to set boundaries, such as not listening to them for periods throughout the day. He also felt more able to challenge what they said and make his own choices.
Over a couple of months, Jason started to experience some breaks from the voices each day and his relationship with them started to change. They were no longer like bullies, but more like critical friends pointing out things he could consider or be aware of.
A screenshot from HekaVR, the software used in the Australian AMETHYST trial. HekaVR, CC BY-ND Gaining recognition
Following promising results overseas and its recommendation by the United Kingdom’s National Institute for Health and Care Excellence, our team has begun adapting the therapy for an Australian context.
We are trialling delivering avatar therapy from our specialist voices clinic via telehealth. We are also testing whether avatar therapy is more effective than the current standard therapy for hearing voices, based on cognitive behavioural therapy.
As only a minority of people with psychosis receive specialist psychological therapy for hearing voices, we hope our trial will support scaling up these new treatments to be available more routinely across the country.
We would like to acknowledge the advice and input of Dr Nadine Keen (consultant clinical psychologist at South London and Maudsley NHS Foundation Trust, UK) on this article.
Leila Jameel, Trial Co-ordinator and Research Therapist, Swinburne University of Technology; Imogen Bell, Senior Research Fellow and Psychologist, The University of Melbourne; Neil Thomas, Professor of Clinical Psychology, Swinburne University of Technology, and Rachel Brand, Senior Lecturer in Clinical Psychology, University of the Sunshine Coast
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: