Exercises for Aging-Ankles
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Can Ankles Deterioration be Stopped?
As we all know (or have experienced!), Ankle mobility deteriorates with age.
We’re here to argue that it’s not all doom and gloom!
(In fact, we’ve written about keeping our feet, and associated body parts, healthy here).
This video by “Livinleggings” (below) provides a great argument that yes, ankle deterioration can be stopped, or even reversed. It’s a must-watch for anyone from yoga enthusiasts to gym warriors who might be unknowingly crippling their ankle-health.
How We Can Prioritise Our Ankles
Poor ankle flexibility isn’t just an inconvenience – it’s a direct route to knee issues, hip hiccups, and back pain. More importantly, ankle strength is a core component of building overall mobility.
With 12 muscles in the ankle, it can be overwhelming to work out which to strengthen – and how. But fear not, we can prioritise three of the twelve: the calf duo (gastrocnemius and soleus) and the shin’s main muscle, the tibialis anterior.
The first step is to test yourself! A simple wall test reveals any hidden truths about your ankle flexibility. Go to the 1:55 point in the video to see how it’s done.
If you can’t do it, you’ve got work to be done.
If you read the book we recommended on great functional exercises for seniors, then you may already be familiar with some super ankle exercises.
Otherwise, these four ankle exercises are a great starting point:
How did you find that video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Problem With Active Listening
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The problem with active listening
Listening is an important skill to keep well-trained at any age. It’s important in romantic relationships, parent-child relationships, friendships, and more.
First, for any unfamiliar or hazy-of-memory: active listening is the practice of listening, actively. The “active” side of this comes in several parts:
- Asking helpful questions
- Giving feedback to indicate that the answer has been understood
- Prompting further information-giving
This can look like:
- A: How did you feel when that happened?
- B: My heart was racing and I felt panicked, it really shocked me
- A: It really shocked you?
- B: Yes, because it was so unexpected; I’d never imagined something like this happening
- A: You’d never expect something like that
- B: No, I mean, I had no reason to
And… As a superficial listening technique, it’s not terrible, and it has its place
But unfortunately, if it’s one’s only listening technique, one will very quickly start sounding like a Furby—that children’s toy from the 90s that allegedly randomly parroted fragments of things that had been said to it. In fact this was a trick of programming, but that’s beyond the scope of this article.
The point is: the above technique, if used indiscriminately and/or too often, starts to feel like talking to a very basic simulacrum.
Which is the opposite of feeling like being listened to!
A better way to listen
Start off similarly, but better.
Ask open questions, or otherwise invite sharing of information.
People can be resistant to stock phrases like “How did that make you feel?”, but this can be got around by simply changing it up, e.g.:
- “What was your reaction?” ← oblique but often elicits the same information
- “I’m not sure how I’d feel about that, in your shoes” ← not even a question, but shows active attention much better than the “mmhmm” noises of traditional active listening, and again prompts the same information
Express understanding… But better
People have been told “I understand” a lot, and often it’s code for “Stop talking”. So, avoid “I understand”. Instead, try:
- “I can understand that”
- “Understandable”
- “That makes sense”
Ask clarifying questions… Better
Sometimes, a clarifying question doesn’t have to have its own point, beyond prompting more sharing, and sometimes, an “open question” can be truly wide open, meaning that vaguer is better, such as:
- “Oh?”
- “How so?” ← this is the heavy artillery that can open up a lot
Know when to STFU
Something that good therapists (and also military interrogators) know: when to STFU
If someone is talking, don’t interrupt them. If you do, they might not start again, or might skip what they were going to say.
Interruption says “I think you’ve said all that needs to be said there”, or else, if the interruption was to ask one of the above questions, it says “you’re not doing a good enough job of talking”, and neither of those sentiments encourage people to share, nor do they make someone feel listened-to!
Instead, just listen. Passive listening has its place too! When there’s a break, then you can go to one of the above questions/prompts/expressions of understanding, as appropriate.
Judge not, lest they feel judged
Reserve judgement until the conversation is over, at the earliest. If asked for your judgement of some aspect, be as reassuring as you can. People feel listened-to when they don’t feel judged.
If they feel judged, conversely, they can often feel you didn’t listen properly, or else you’d be in agreement with them. So instead, just sit on it for as long as you can.
Note: that goes for positive judgements too! Sit on it. Expressing a positive judgement too soon can seem that you were simply eager to please, and can suggest insincerity.
If this seems simple, that’s because it is. But, try it, and see the difference.
Share This Post
-
Head Over Hips
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about managing osteoarthritis (or ideally: avoiding it, but that’s not always an option on the table, of course), so here’s a primer/refresher before we get into the meat of today’s article:
Avoiding/Managing Osteoarthritis
When the head gets in the way
Research shows that the problem with recovery in cases of osteoarthritis of the hip is in fact often not the hip itself, but rather, the head:
❝In fact, the stronger your muscles are, the more protected your joint is, and the less pain you will experience.
Our research has shown that people with hip osteoarthritis were unable to activate their muscles as efficiently, irrespective of strength.
Basically, people with hip arthritis are unable to activate their muscles properly because the brain is actively putting on the brake to stop them from using the muscle.❞
This is a case of a short-term protective response being unhelpful in the long-term. If you injure yourself, your brain will try to inhibit you from exacerbating that injury, such as by (for example) disobliging you from putting weight on an injured joint.
This is great if you merely twisted an ankle and just need to sit back and relax while your body works its healing magic, but it’s counterproductive if it’s a chronic issue like osteoarthritis. In such (i.e. chronic) cases, avoidance of use of the joint will simply cause atrophy of the surrounding muscle and other tissues, leading to more of the very wear-and-tear that led to the osteoarthritis in the first place.
So… How to deal with that?
You probably can exercise
It’s easy to get caught between the dichotomy of “exercise and inflame your joints” vs “rest and your joints seize up”, which is not pleasant.
However, the trick lies in how you exercise, per joint type:
When Bad Joints Stop You From Exercising (5 Things To Change)
…which to be clear, isn’t a case of “avoid using the joint that’s bad”, but is rather “use it in this specific way, so that it gets stronger without doing it more damage in the process”.
Which is exactly what is needed!
Further resources
For those who like learning from short videos, here’s a trio of helpers (along with our own text-based overview for each):
- The Most Underrated Hip Mobility Exercise (Not Stretching)
- Overcome Front-Of-Hip Pain
- 10 Tips To Reduce Morning Pain & Stiffness With Arthritis
And for those who prefer just reading, here’s a book we reviewed on the topic:
11 Minutes to Pain-Free Hips – by Melinda Wright
Take care!
Share This Post
-
Long-acting contraceptives seem to be as safe as the pill when it comes to cancer risk
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Many women worry hormonal contraceptives have dangerous side-effects including increased cancer risk. But this perception is often out of proportion with the actual risks.
So, what does the research actually say about cancer risk for contraceptive users?
And is your cancer risk different if, instead of the pill, you use long-acting reversible contraceptives? These include intrauterine devices or IUDs (such as Mirena), implants under the skin (such as Implanon), and injections (such as Depo Provera).
Our new study, conducted by the University of Queensland and QIMR Berghofer Medical Research Institute and published by the Journal of the National Cancer Institute, looked at this question.
We found long-acting contraceptives seem to be as safe as the pill when it comes to cancer risk (which is good news) but not necessarily any safer than the pill.
Peakstock/Shutterstock Some hormonal contraceptives take the form of implants under the skin. WiP-Studio/Shutterstock How does the contraceptive pill affect cancer risk?
The International Agency for Research on Cancer, which compiles evidence on cancer causes, has concluded that oral contraceptives have mixed effects on cancer risk.
Using the oral contraceptive pill:
- slightly increases your risk of breast and cervical cancer in the short term, but
- substantially reduces your risk of cancers of the uterus and ovaries in the longer term.
Our earlier work showed the pill was responsible for preventing far more cancers overall than it contributed to.
In previous research we estimated that in 2010, oral contraceptive pill use prevented over 1,300 cases of endometrial and ovarian cancers in Australian women.
It also prevented almost 500 deaths from these cancers in 2013. This is a reduction of around 25% in the deaths that could have occurred that year if women hadn’t taken the pill.
In contrast, we calculated the pill may have contributed to around 15 deaths from breast cancer in 2013, which is less than 0.5% of all breast cancer deaths in that year.
Previous work showed the pill was responsible for preventing far more cancers overall than it contributed to. Image Point Fr What about long-acting reversible contraceptives and cancer risk?
Long-acting reversible contraceptives – which include intrauterine devices or IUDs, implants under the skin, and injections – release progesterone-like hormones.
These are very effective contraceptives that can last from a few months (injections) up to seven years (intrauterine devices).
Notably, they don’t contain the hormone oestrogen, which may be responsible for some of the side-effects of the pill (including perhaps contributing to a higher risk of breast cancer).
Use of these long-acting contraceptives has doubled over the past decade, while the use of the pill has declined. So it’s important to know whether this change could affect cancer risk for Australian women.
Our new study of more than 1 million Australian women investigated whether long-acting, reversible contraceptives affect risk of invasive cancers. We compared the results to the oral contraceptive pill.
We used de-identified health records for Australian women aged 55 and under in 2002.
Among this group, about 176,000 were diagnosed with cancer between 2004 and 2013 when the oldest women were aged 67. We compared hormonal contraceptive use among these women who got cancer to women without cancer.
We found that long-term users of all types of hormonal contraception had around a 70% lower risk of developing endometrial cancer in the years after use. In other words, the risk of developing endometrial cancer is substantially lower among women who took hormonal contraception compared to those who didn’t.
For ovarian cancer, we saw a 50% reduced risk (compared to those who took no hormonal contraception) for women who were long-term users of the hormone-containing IUD.
The risk reduction was not as marked for the implants or injections, however few long-term users of these products developed these cancers in our study.
As the risk of endometrial and ovarian cancers increases with age, it will be important to look at cancer risk in these women as they get older.
What about breast cancer risk?
Our findings suggest that the risk of breast cancer for current users of long-acting contraceptives is similar to users of the pill.
However, the contraceptive injection was only associated with an increase in breast cancer risk after five years of use and there was no longer a higher risk once women stopped using them.
Our results suggested that the risk of breast cancer also reduces after stopping use of the contraceptive implants.
We will need to follow-up the women for longer to determine whether this is also the case for the IUD.
It is worth emphasising that the breast cancer risk associated with all hormonal contraceptives is very small.
About 30 in every 100,000 women aged 20 to 39 years develop breast cancer each year, and any hormonal contraceptive use would only increase this to around 36 cases per 100,000.
What about other cancers?
Our study did not show any consistent relationships between contraceptive use and other cancers types. However, we only at looked at invasive cancers (meaning those that start at a primary site but have the potential to spread to other parts of the body).
A recent French study found that prolonged use of the contraceptive injection increased the risk of meningioma (a type of benign brain tumour).
However, meningiomas are rare, especially in young women. There are around two cases in every 100,000 in women aged 20–39, so the extra number of cases linked to contraceptive injection use was small.
The French study found the hormonal IUD did not increase meningioma risk (and they did not investigate contraceptive implants).
Benefits and side-effects
There are benefits and side-effects for all medicines, including contraceptives, but it is important to know most very serious side-effects are rare.
A conversation with your doctor about the balance of benefits and side-effects for you is always a good place to start.
Susan Jordan, Professor of Epidemiology, The University of Queensland; Karen Tuesley, Postdoctoral Research Fellow, School of Public Health, The University of Queensland, and Penny Webb, Distinguished Scientist, Gynaecological Cancers Group, QIMR Berghofer Medical Research Institute
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
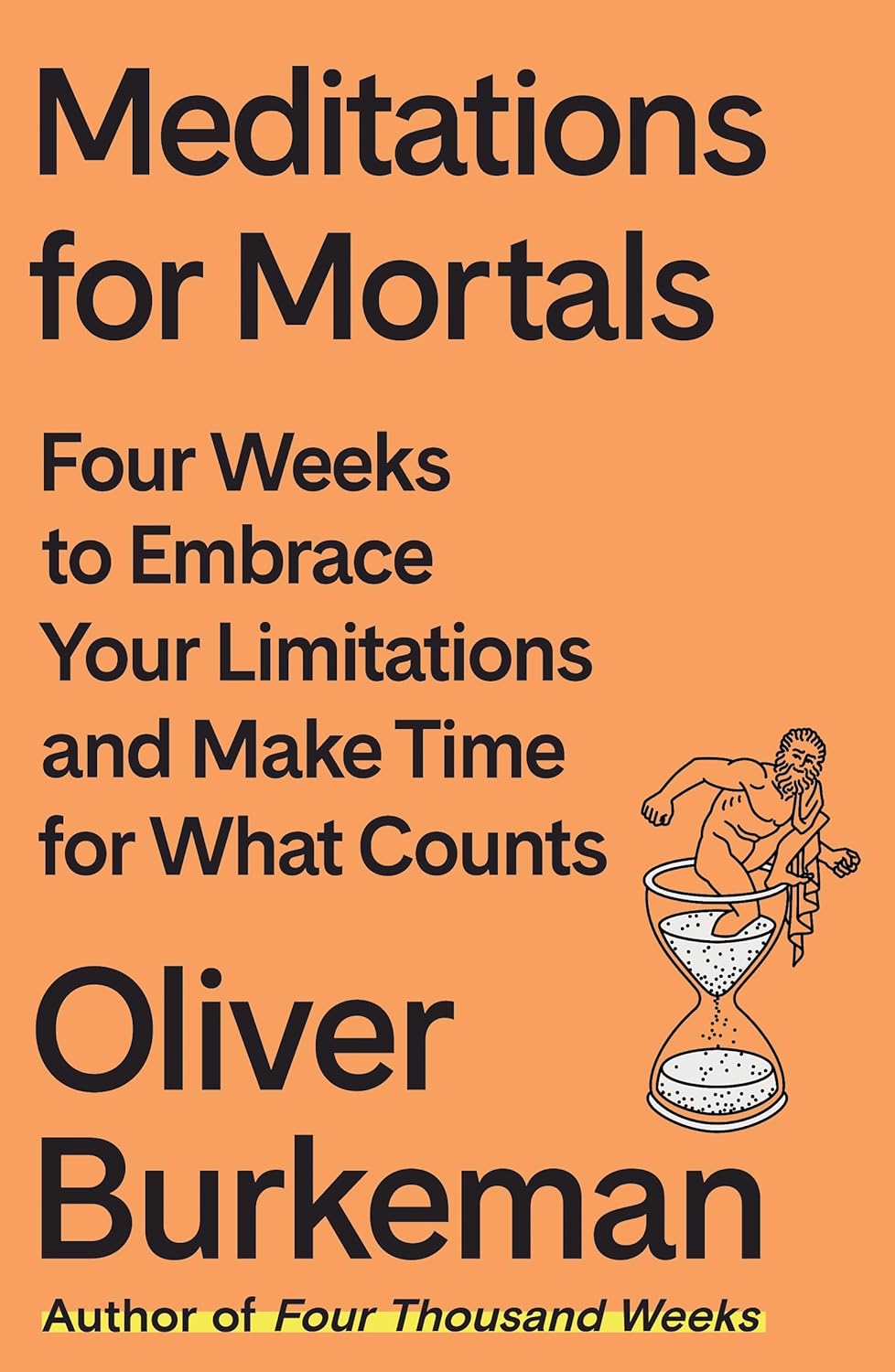
Meditations for Mortals – by Oliver Burkeman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We previously reviewed this author’s “Four Thousand Weeks”, but for those who might have used a lot of those four thousand weeks already, and would like to consider things within a smaller timeframe for now, this work is a 28-day daily reader.
Now, daily readers are usually 366 days, but the chapters here are not the single page chapters that 366-page daily readers usually have. So, expect to invest a little more time per day (say, about 6 pages for each daily chapter).
Burkeman does not start the way we might expect, by telling us to take the time to smell the roses. Instead, he starts by examining the mistakes that most of us make most of the time, often due to unexamined assumptions about the world and how it works. Simply put, we’ve often received bad lessons in life (usually not explicitly, but rather, from our environments), and it takes some unpacking first to deal with that.
Nor is the book systems-based, as many books that get filed under “time management” may be, but rather, is simply principles-based. This is a strength, because principles are a lot easier to keep to than systems.
The writing style is direct and conversational, and neither overly familiar nor overly academic. It strikes a very comfortably readable balance.
Bottom line: if you’d like to get the most out of your days, this book can definitely help improve things a lot.
Click here to check out Meditations For Mortals, and live fulfilling days!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
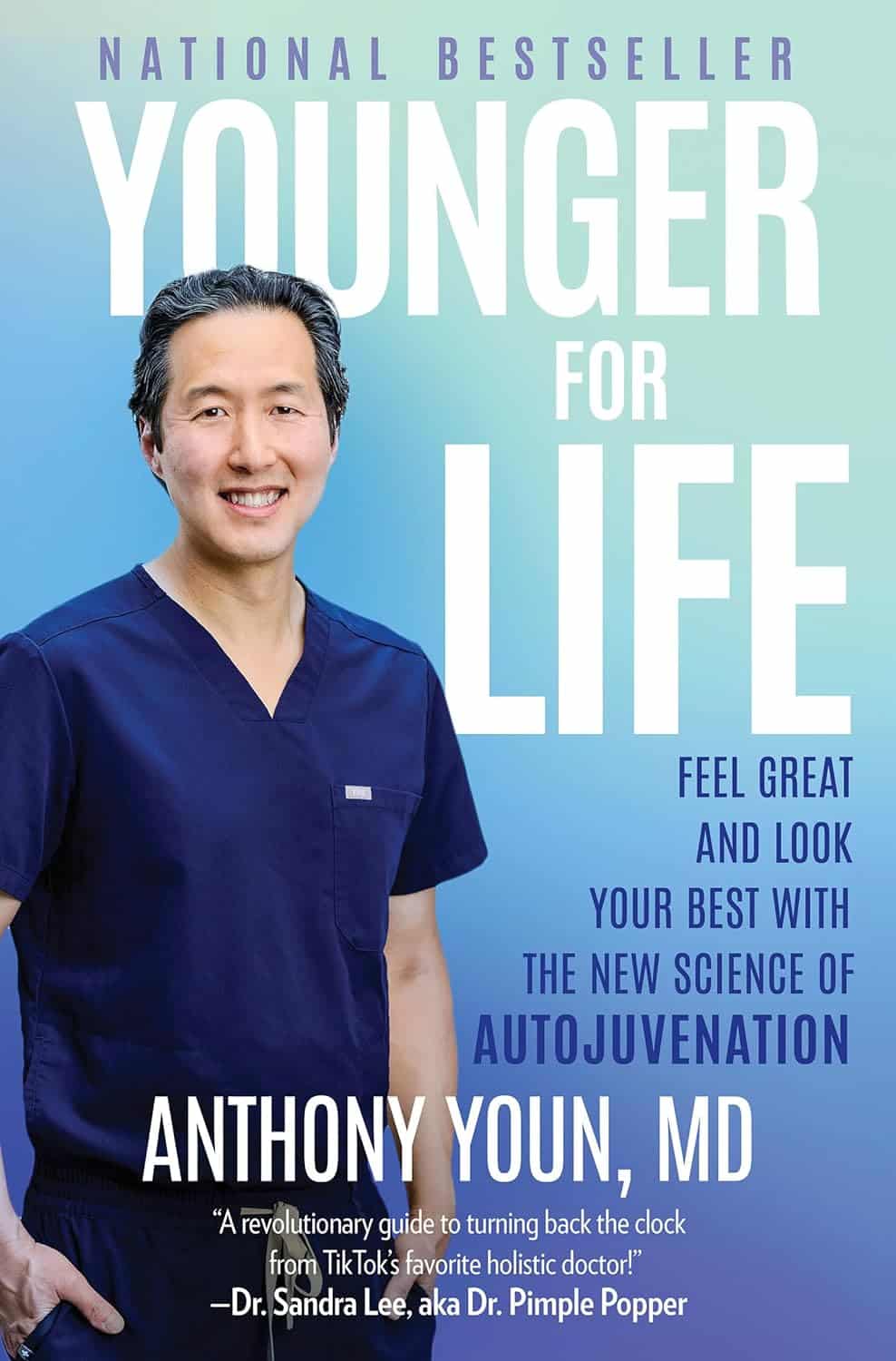
Younger For Life – by Dr. Anthony Youn
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed anti-aging books before, so what makes this one different? Mostly, it’s the very practical focus.
Which is not to say there’s not also good science in here; there is. But the focus is on what everything means for the reader, not what happened with a certain cohort of lab mice. Instead, he looks at the causes of aging, the process of aging, and what interventions to implement to address those, and reverse many of them.
Some parts are more general lifestyle interventions that 10almonds readers will know well already, but other parts are very specific advices, protocols, and regimes; in particular his skincare section is well worth reading. As for nutrition, there’s even a respectable recipes section, so this book does have it all!
The final section of the book is dedicated to plastic surgeries (the author is a plastic surgeon who believes that most people should not need those, and would do well to stick to the advices in the rest of the book). We suspect this last part of the book will be of least interest to 10almonds readers.
Bottom line: if you’re of the view that getting older should come with as little as possible physical deterioration along the way, then this book can help a lot with that.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Life Extension Multivitamins vs Centrum Multivitamins – Which is Healthier
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing Life Extension Multivitamins to Centrum Multivitamins, we picked the Life Extension.
Why?
The clue here was on the label: “two per day”. It’s not so that they can sell extra filler! It’s because they couldn’t fit it all into one.
While the Centrum Multivitamins is a (respectably) run-of-the-mill multivitamin (and multimineral) containing reasonable quantities of most vitamins and minerals that people supplement, the Life Extension product has the same plus more:
- More of the vitamins and minerals; i.e. more of them are hitting 100%+ of the RDA
- More beneficial supplements, including:
- Inositol, Alpha lipoic acid, Bio-Quercetin phytosome, phosphatidylcholine complex, Marigold extract, Apigenin, Lycopene, and more that we won’t list here because it starts to get complicated if we do.
We’ll have to write some main features on some of those that we haven’t written about before, but suffice it to say, they’re all good things.
Main take-away for today: sometimes more is better; it just necessitates then reading the label to check.
Want to get some Life Extension Multivitamins (and/or perhaps just read the label on the back)? Here they are on Amazon
PS: it bears mentioning, since we are sometimes running brands against each other head-to-head in this section: nothing you see here is an advertisement/sponsor unless it’s clearly marked as such. We haven’t, for example, been paid by Life Extension or any agent of theirs, to write the above. It’s just our own research and conclusion.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: