Elderhood – by Dr. Louise Aronson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Where does “middle age” end, and “old age” begin? By the United States’ CDC’s categorization, human life involves:
- 17 stages of childhood, deemed 0–18
- 5 stages of adulthood, deemed 18–60
- 1 stage of elderhood, deemed 60+
Isn’t there something missing here? Do we just fall off some sort of conveyor belt on our sixtieth birthdays, into one big bucket marked “old”?
Yesterday you were 59 and enjoying your middle age; today you have, apparently, the same medical factors and care needs as a 114-year-old.
Dr. Louise Aronson, a geriatrician, notes however that medical science tends to underestimate the differences found in more advanced old age, and underresearch them. That elders consume half of a country’s medicines, but are not required to be included in clinical trials. That side effects not only are often different than for younger adults, but also can cause symptoms that are then dismissed as “Oh she’s just old”.
She explores, mostly through personal career anecdotes, the well-intentioned disregard that is frequently given by the medical profession, and—importantly—how we might overcome that, as individuals and as a society.
Bottom line: if you are over the age of 60, love someone over the age of 60, this is a book for you. Similarly if you and/or they plan to live past the age of 60, this is also a book for you.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Get Well, Stay Well – by Dr. Gemma Newman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Gemma Newman is a GP (British equivalent of what in America is called a “family doctor”) who realized she was functioning great as a diagnostic flowchart interpreter and pill dispensary, but not actually doing much of what she got into the job to do: helping people.
Her patients were getting plenty of treatments, but not getting better. Often, they were getting worse. And she knew why: they come in for treatment for one medical problem, when they have six and a half medical problems probably a stack of non-medical problems that contributed to them,
So, this book sets out to do what she tries to do in her office, but often doesn’t have the time: treat the whole person.
In it, she details what areas of life to look at, what things are most likely to contribute to wellness/unwellness (be those things completely in your power or not), and how to—bit by bit—make all the parts better, and keep them that way.
The writing style is conversational, and while it’s heavily informed by her professional competence, there’s no arcane science here; it’s more about the system of bringing everything together harmoniously.
Bottom line: if you think there’s more to wellness than can be represented on an annual physicals chart, then this is the book to help you get/keep on top of things.
Click here to check out Get Well, Stay Well, and do just that!
Share This Post
-
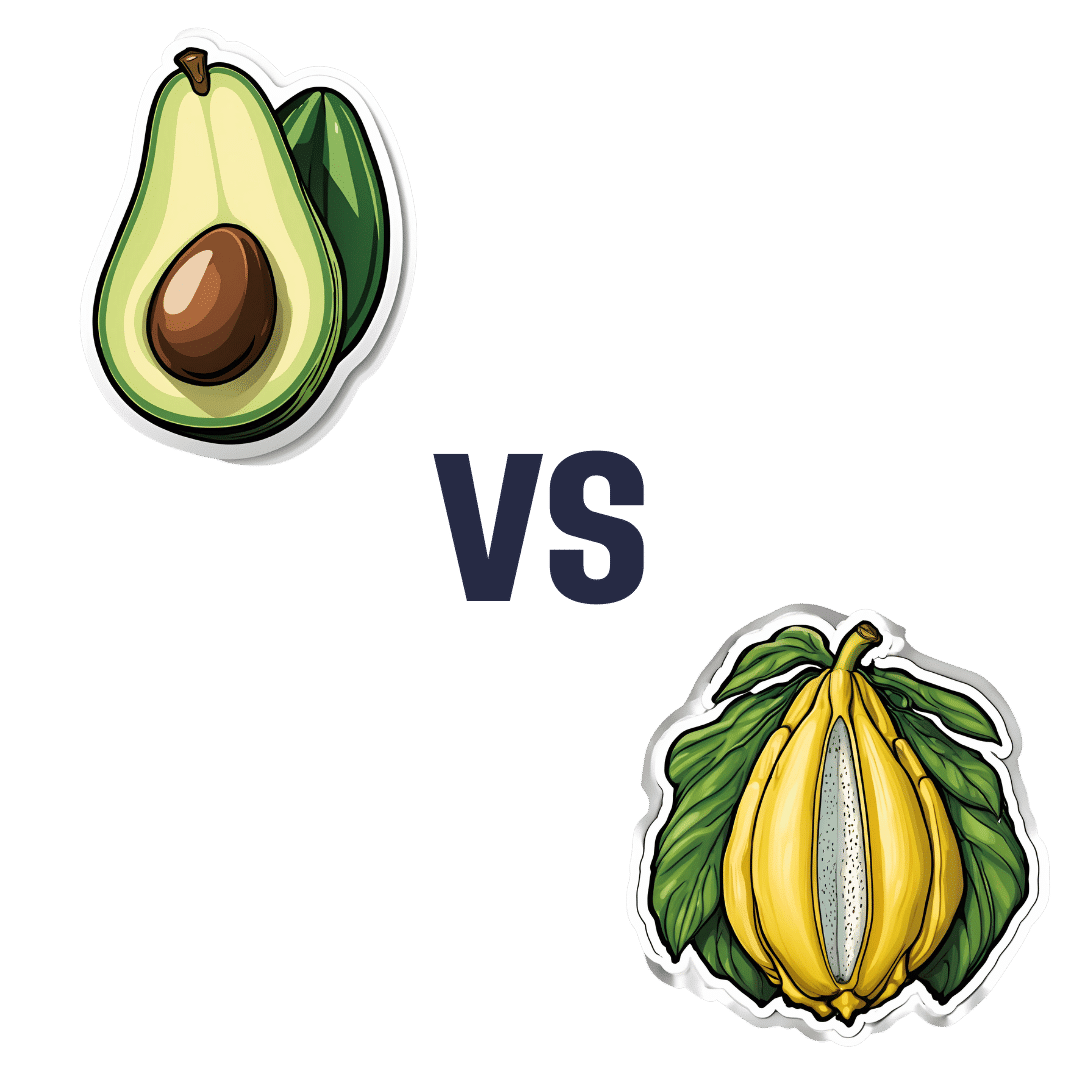
Avocado vs Jackfruit – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing avocado to jackfruit, we picked the avocado.
Why?
In terms of macros, avocado is higher in fats (famously healthy ones, including a good dose of omega-3), fiber (nearly 5x more), and protein (despite jackfruit being more often used as a meaty element in recipes, avocado has slightly more). Meanwhile, jackfruit is about 3x higher in carbs. All in all, a clear win for avocado.
Looking at vitamins, avocado has more of vitamins A, B2, B3, B5, B7, B9, E, K, and choline, while jackfruit has more of vitamins B1, B6, and C. Another win for avocado in this category.
In the category of minerals, avocado has more copper, iron, manganese, phosphorus, potassium, selenium, and zinc, while jackfruit has more calcium. One more win for avocado.
Adding up the sections makes for an easy overall win for avocado, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
Jackfruit vs Durian – Which is Healthier? ← including some fun durian facts (such as how to pick a good one, and what happens if you eat durian and drink alcohol)
Enjoy!
Share This Post
-
To Pee Or Not To Pee
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Is it “strengthening” to hold, or are we doing ourselves harm if we do? Dr. Heba Shaheed explains in this short video:
A flood of reasons not to hold
Humans should urinate 4–6 times daily, but for many people, the demands of modern life often lead to delaying urination, raising questions about its effects on the body.
So first, let’s look at how it all works: the bladder is part of the urinary system, which includes the kidneys, ureters, urethra, and sphincters. Urine is produced by the kidneys and transported via the ureters into the bladder, a hollow organ with a muscular wall. This muscle (called the detrusor) allows the bladder to inflate as it fills with urine (bearing in mind, the main job of any muscle is to be able to stretch and contract).
As the bladder fills, stretch receptors in that muscle signal fullness to the spinal cord. This triggers the micturition reflex, causing the detrusor to contract and the internal urethral sphincter to open involuntarily. Voluntary control over the external urethral sphincter allows a person to delay or release urine as needed.
So, at what point is it best to go forth and pee?
For most people, bladder fullness is first noticeable at around 150-200ml, with discomfort occurring at 400-500ml (that’s about two cups*). Although the bladder can stretch to hold up to a liter, exceeding this capacity can cause it to rupture, a rare but serious condition requiring surgical intervention.
*note, however, that this doesn’t necessarily mean that drinking two cups will result in two cups being in your bladder; that’s not how hydration works. Unless you are already perfectly hydrated, most if not all of the water will be absorbed into the rest of your body where it is needed. Your bladder gets filled when your body has waste products to dispose of that way, and/or is overhydrated (though overhydration is not very common).
Habitually holding urine and/or urinating too quickly (note: not “too soon”, but literally, “too quickly”, we’re talking about the velocity at which it exits the body) can weaken pelvic floor muscles over time. This can lead to bladder pain, urgency, incontinence, and/or a damaged pelvic floor.
In short: while the body’s systems are equipped to handle occasional delays, holding it regularly is not advisable. For the good of your long-term urinary health, it’s best to avoid straining the system and go whenever you feel the urge.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Keeping your kidneys happy: it’s more than just hydration!
Take care!
Share This Post
Related Posts
-
Easing Lower Back Pain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Lower back pain often originates from an unexpected culprit: your pelvis. Similar to how your psoas can contribute to lower back pain, when your pelvis tilts forward due to tight hip flexors, it can misalign your spine, leading to discomfort and pain. As WeShape shows us in the below video, one simple stretch can help realign your pelvis and significantly ease lower back pain.
Why Your Pelvis Matters
Sitting for long periods causes your hip flexors to shorten, leading to an anterior pelvic tilt. This forward tilt puts pressure on your spine and SI joint, causing pain and discomfort in the lower back. To help resolve this, you can work on correcting your pelvic alignment, helping to significantly reduce this pressure and alleviate related pain. And no, this doesn’t require any spinal cord stimulation.
Easy Variations for All
A lot of you recognise the stretch in this video; it’s quite a well-known kneeling stretch. But, unlike other guides, WeShape also provides a fantastic variation for those who aren’t mobile enough for the kneeling variation
So, if you can’t comfortably get down on the ground, WeShape outlines a brilliant standing variation. So, regardless of your mobility, there’s an option for you!
See both variations here:
Excited to reduce your lower back pain? We hope so! Let us know if you have any tips that you’d like to share with us.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why STIs Are On The Rise In Older Adults
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Three Little Words
Sexually Transmitted Infections (STIs) are often thought of as something that predominantly plagues younger people… The truth, however, is different:
❝Rising divorce rates, forgoing condoms as there is no risk of pregnancy, the availability of drugs for sexual dysfunction, the large number of older adults living together in retirement communities, and the increased use of dating apps are likely to have contributed to the growing incidence of STIs in the over-50s.
These data likely underestimate the true extent of the problem as limited access to sexual health services for the over 50s, and trying to avoid the stigma and embarrassment both on the part of older people and healthcare professionals, is leading to this age group not seeking help for STIs.❞
Read more: Managing The Rise In STIs Among Older Adults
That said, there is a gender gap when it comes to the increased risk, for example:
❝A retrospective study from the USA involving 420,790 couples aged 67 to 99 years, found that widowhood was associated with an increased risk of STIs in older men, but not women❞
~ US Dept of Health & Human Services
Source: CDC: | Sexually Transmitted Disease Surveillance
Is abstinence the best preventative, then?
It is inarguably the most effective, but not necessarily the best for everyone.
This is because for most adults, a healthy sex life is an important part of overall wellbeing.
See also: Mythbusting The Big O
Even in this case there is a gender gap in:
- the level of importance placed on frequency of sexual interactions
- what act(s) of sexuality are held to be most important:
❝Among sexually active men, frequent (≥2 times a month) sexual intercourse (P < .001) and frequent kissing, petting, or fondling (P < .001) were associated with greater enjoyment of life.
Among sexually active women, frequent kissing, petting, or fondling was also associated with greater enjoyment of life (P < .001), but there was no significant association with frequent intercourse (P = .101).
Concerns about one’s sex life and problems with sexual function were strongly associated with lower levels of enjoyment of life in men and to a lesser extent in women.❞
Source: Sexual Activity is Associated with Greater Enjoyment of Life in Older Adults
If you have the time to go into it much more deeply, this paper from the Journal of Gerontology is much more comprehensive, looking also at related lifestyle factors, religious/political backgrounds, views on monogamy or non-monogamy (of various kinds), hormonal considerations, the impact of dementia or other long-term disabilities that may affect things, widowhood, and many other elements:
The National Social Life, Health, and Aging Project: An Introduction
What’s the best preventative, then?
Regular health screening for yourself and your partner(s) is an important key to preventative health when it comes to STIs.
You can Google search for a local STI clinic, and worry not, they are invariably discreet and are well-used to everybody coming in. They’re just glad you’re being responsible about things. It’s also not their job to judge your sexual activities, even if it’s something you might have reason to wish to be secretive about, try to be honest there.
Secondly, most of the usual advice about safe sex still goes, even when there’s no risk of pregnancy. For example, if there’s at least one penis involved, then condoms remain the #1 barrier to all manner of potential infections (we know, almost nobody likes condoms, but sometimes the truth isn’t what we want to hear).
Lastly, if there’s at least one vagina involved, then please for the love of all that is holey, do not put anything there that could cause a yeast infection.
What can cause a yeast infection? Pretty much anything with sugar, which includes but is not limited to:
- Most kinds of food that Cosmo-style “liven things up in the bedroom” advice columns might suggest using (including fruit, honey, chocolate sauce, whipped cream, etc)
- Hands that are not clean (watch out for bacteria too)
- A mouth that has recently been eating or drinking anything with sugar in it, and that includes many kinds of alcohol, as well as milk or hot drinks that had milk in
Yeast infections are not nearly so serious as the STIs the other measures are there to avoid, but they’re not fun either, so some sensible policies in that regard are always good!
On a related note, see also: How To Avoid UTIs
Recap on the single most important part of this article:
At all ages, it remains a good health practice—unless one is absolutely celibate—to regularly get oneself and one’s partner(s) checked for STIs.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
More research shows COVID-19 vaccines are safe for young adults
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What you need to know
- Myocarditis, or inflammation of the heart muscle, is most commonly caused by a viral infection like COVID-19, not by vaccination.
- In line with previous research, a recent CDC study found no association between COVID-19 vaccination and sudden cardiac death in previously healthy young people.
- A COVID-19 infection is much more likely to cause inflammation of the heart muscle than a COVID-19 vaccine, and those cases are typically more severe.
Since the approval of the first COVID-19 vaccines, anti-vaccine advocates have raised concerns about heart muscle inflammation, also called myocarditis, after vaccination to suggest that vaccines are unsafe. They’ve also used concerns about myocarditis to spread false claims that vaccines cause sudden deaths, which is not true.
Research has consistently shown that cases of myocarditis after vaccination are extremely rare and usually mild, and a new study from the CDC found no association between sudden cardiac death and COVID-19 vaccination in young adults.
Read on to learn more about myocarditis and what the latest research says about COVID-19 vaccine safety.
What is myocarditis?
Myocarditis is inflammation of the myocardium, or the middle muscular layer of the heart wall. This inflammation weakens the heart’s ability to pump blood. Symptoms may include fatigue, shortness of breath, chest pain, rapid or irregular heartbeat, and flu-like symptoms.
Myocarditis may resolve on its own. In rare cases, it may lead to stroke, heart failure, heart attack, or death.
What causes myocarditis?
Myocarditis is typically caused by a viral infection like COVID-19. Bacteria, parasites, fungi, chemicals, and certain medications can also cause myocarditis.
In very rare cases, some people develop myocarditis after receiving a COVID-19 vaccine, but these cases are usually mild and resolve on their own. In contrast, a COVID-19 infection is much more likely to cause myocarditis, and those cases are typically more severe.
Staying up to date on vaccines reduces your risk of developing myocarditis from a COVID-19 infection.
Are COVID-19 vaccines safe for young people?
Yes. COVID-19 vaccines have been rigorously tested and monitored over the past three years and have been determined to be safe for everyone 6 months and older. A recent CDC study found no association between COVID-19 vaccination and sudden cardiac death in previously healthy young adults.
The benefits of vaccination outweigh any potential risks. Staying up to date on COVID-19 vaccines reduces your risk of severe illness, hospitalization, death, long COVID, and COVID-19-related complications, such as myocarditis.
The CDC recommends people 65 and older and immunocompromised people receive an additional dose of the updated COVID-19 vaccine this spring—if at least four months have passed since they received a COVID-19 vaccine.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: