How (And Why) To Train Your Pre-Frontal Cortex
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Chapman’s Keys For Mental Focus
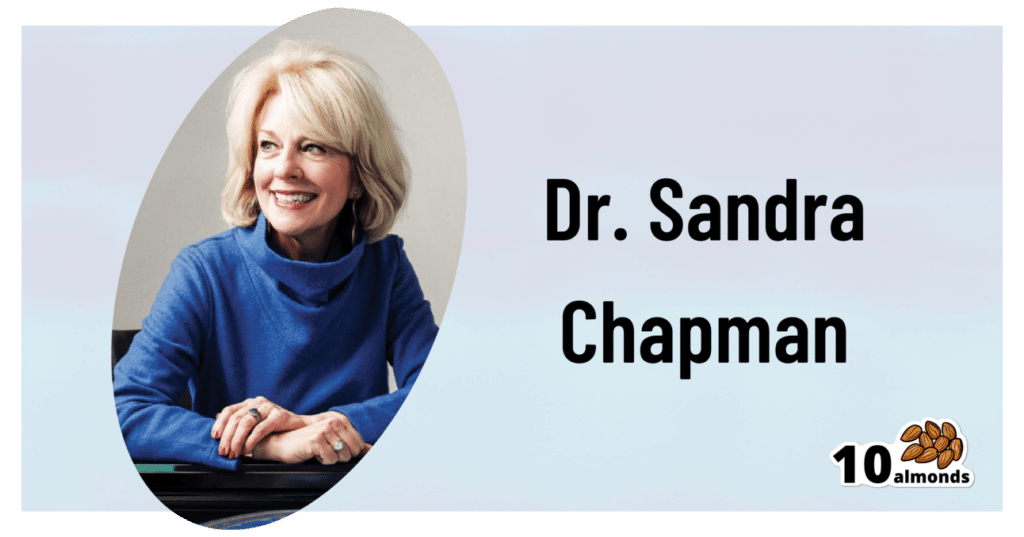
This is Dr. Sandra Chapman; she’s a cognitive neuroscientist, on a mission to, in her words, further our understanding of:
- what makes the brain stronger, faster and last longer
- what enhances human cognitive capacity, and
- what enhances the underlying brain systems across the lifespan.
To this end, she’s also the founder and Chief Director of the Center For Brain Health, where she has worked on her mission for the past 25 years (clocking up hundreds of peer-reviewed publications to her name), as well as being a professor of Behavioral and Brain Sciences at UT Dallas.
What does she want us to know?
Get your brain into gear
When it comes to your brainpower, it is “use it or lose it”, but it is also perfectly possible to use it and lose it.
Why?
Very often, what we are using our brains for is high-strain, low-yield stuff, such as multitasking, overthinking, or overthinking while multitasking. And to make it worse, we often do it without sufficient rest.
This is the equivalent of owning a Ferrari but trying to drive it in second and third gear at once by switching between the two as rapidly as possible. And doing that for 18 hours each day.
Suffice it to say, you’ll be going nowhere quickly.
An alternative “use” of brainpower is low-strain, low-yield stuff, such as having to pay close attention to a boring conversation. It’s enough to stop your mind from doing anything else, but not enough to actually stimulate you.
This is the equivalent of owning a Ferrari but keeping it idling. The wear and tear is minimal this time, but you’re not actually going anywhere either.
Better, of course, are the other two quadrants:
- low-strain, high-yield: consistently using our brain in relatively non-taxing ways that encourage its development
- high-strain, high-yield: here the Ferrari metaphor definitely fails, because unlike cars, our bodies (including our brains) are machines that benefit from judicious regular progressive overloading (but just by a bit, and with adequate recovery time between overloads).
See also: 12 Weeks To Measurably Boost Your Brain
How to do the “low-strain, low-yield” part
When it comes to “what’s the most important part of the brain to help in the face of cognitive decline?” the usual answer is either to focus on memory (hippocampi) or language (various parts, but for example Wernicke’s area and Broca’s area), since people most fear losing memory, and language is very important both socially and practically.
Those are indeed critical, and we at 10almonds stand by them, but Dr. Chapman (herself having originally trained as speech and language pathologist!) makes a strong case for adding a third brain part to the list.
Specifically, she advocates for strengthening the pre-frontal cortex, which is responsible for inhibition, task-switching, working memory, and cognitive flexibility. If that seems like a lot, do remember it’s a whole cortex and not one of the assorted important-but-small brain bits we mentioned above.
How? She has developed training programs for this, based on what she calls Strategic Memory Advanced Reasoning Tactics (SMART), to support support attention, planning, judgment and emotional management.
You can read more about those programs here:
Center For Brain Health | Our Programs
Participation in those is mostly not free, however, if you join their…
Center For Brain Health | BrainHealth Project
…then they will periodically invite you to join pilot programs, research programs, and the like, which will either be free or they-pay-you affairs—because this is how science is done, and you can read about yourself (anonymized, of course) later in peer-reviewed papers of the kind we often cite here.
If you’re not interested in any of that though, we will say that according to Dr. Chapman, the keys are:
Inhibition: be conscious of this function of your brain, and develop it. This is the function of your brain that stops you from making mistakes—or put differently: stops you from saying/doing something stupid.
Switching: do this consciously; per “I am now doing this task, now I am switching to this other task”, rather than doing the gear-grinding thing we discussed earlier
Working memory: this is effectively your brain’s RAM. Unlike the RAM of a computer (can be enhanced by adding another chip or replacing with a bigger chip), our brain’s RAM can be increased by frequent use, and especially by judicious use of progressive overloading (with rests between!) which we’ll discuss in the high-strain, high-yield section.
Flexibility: this is about creative problem-solving, openness to new ideas, and curiosity
See also: Curiosity Kills The Neurodegeneration
How to do the “high-strain, high-yield” part
Delighting this chess-playing writer, Dr. Chapman recommends chess. Although, similar games such as go (a Chinese game that looks simpler than chess but actually requires more calculation) work equally well too.
Why?
Games like chess and go cause structural changes that are particularly helpful, in terms of engaging in such foundational tasks as learning, abstract reasoning, problem-solving and self-control:
Chess Practice as a Protective Factor in Dementia
Basically, it checks (so to speak) a lot of boxes, especially for the pre-frontal cortex. Some notes:
- Focusing on the game is required for brain improvement; simply pushing wood casually will not do it. Ideally, calculating several moves ahead will allow for strong working memory use (because to calculate several moves ahead, one will have to hold increasingly many possible positions in the mind while doing so).
- The speed of play must be sufficiently slow as to allow not only for thinking, but also for what in chess is called “blunder-checking”, in other words, having decided on one’s move, pausing to consider whether it is a mistake, and actively trying to find evidence that it is. This is the crucial “inhibition habit”, and when one does it reflexively, one will make fewer mistakes. Tying this to dementia, see for example how one of the common symptoms of dementia is falling for scams that one wouldn’t have previously. How did cognitive decline make someone naïve? It didn’t, per se; it just took away their ability to, having decided what to do, pause to consider whether it was a mistake, and actively trying to find evidence that it is.
- That “conscious switching” that we talked about, rather than multitasking? In chess, there is a difference between strategy and tactics. Don’t worry about what that difference is for now (learn it if you want to take up chess), but know that strong players will only strategize while it is their opponent’s turn, and only calculate (tactics) while it is their own turn. It’s very tempting to flit constantly between one and the other, but chess requires players to have the mental discipline be able to focus on one task or the other and stick with that task until it’s the appointed time to switch.
If you feel like taking up chess, this site (and related app, if you want it) is free (it’s been funded by voluntary donations for a long time now) and good and even comes with free tuition and training tools: LiChess.org
Here’s another site that this writer (hi, it’s me) personally uses—it has great features too, but many are paywalled (I’m mostly there just because I’ve been there nearly since its inception, so I’m baked into the community now): Chess.com
Want to know more?
You might like this book by Dr. Chapman, which we haven’t reviewed yet but it did inform large parts of today’s article:
Make Your Brain Smarter: Increase Your Brain’s Creativity, Energy, and Focus – by Dr. Sandra Chapman
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Great Cholesterol Myth, Revised and Expanded – by Dr. Jonny Bowden and Dr. Stephen Sinatra
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The topic of cholesterol, and saturated fat for that matter, is a complex and often controversial one. How does this book treat it?
With strong opinions, is how—but backed by good science. The authors, a nutritionist and a cardiologist, pull no punches about outdated and/or cherry-picked science, and instead make the case for looking at what, statistically speaking, appear to be the real strongest risk factors.
So, are they advocating for Dave Asprey-style butter-guzzling, or “the carnivore diet”? No, no they are not. Those things remain unhealthy, even if they give some short-term gains (of energy levels, weight loss, etc).
They do advocate, however, for enjoying saturated fats in moderation, and instead of certain polyunsaturated seed oils that do far worse. They also advocate strongly for avoiding sugar, stress, and (for different reasons) statins (in most people’s cases).
They also demystify in clear terms, and often with diagrams and infographics, the various kinds of fats and their components, broken down in far more detail than any other pop-science source this reviewer has seen.
Bottom line: if you want to take a scientific approach to heart health, this book can help you to focus on what will actually make the biggest difference.
Share This Post
-
A Planet of Viruses – by Carl Zimmer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed numerous books on the immune system before, and this one’s mostly not about that.
Instead, this one focuses on the viruses themselves, and the part they play in our world, for good and for ill. Popular awareness tends to focus on the ill, of course.
But, there’s a lot that viruses do for us too, including:
- Weak/harmless viruses that keep our immune systems on their toes and ready
- Bacteriophage viruses that kill and consume pathogens that, left unchecked, would do the same to us
- Endogenous retroviruses that have become symbiotic with the human organism, without which our species would quickly go extinct
He also talks about biological warfare, and how we cannot bury our heads in the sand by avoiding research on those grounds, because someone will always do it anyway, so (as the motto of the immune system itself might say), best to be prepared.
The author is a science journalist, by the way, and has no PhD, but does have a flock of Fellowships and assorted scientific awards and honors, so he appears to be doing good work so far as the scientific community is concerned.
Bottom line: if you’d like to know more about viruses than “they’re very small and can cause harm”, then this book will open a whole new world.
Click here to check out A Planet of Viruses, and upgrade your knowledge!
Share This Post
-
Starfruit vs Soursop – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing starfruit to soursop, we picked the soursop.
Why?
First, by starfruit, we also mean carambola, which is a different name for the same fruit, and by soursop we also mean graviola/guyabano/guanábana, which are different namers for the same fruit. Now, as for their health qualities:
In terms of macros, the soursop has more carbs and fiber, the ratio of which also give it the lower glycemic index. So, a win for soursop here.
When it comes to vitamins, starfruit has more of vitamins A, B5, C, and E, while soursop has more of vitamins B1, B2, B3, B6, B7, B9, and K. Another win for soursop.
In the category of minerals, starfruit has slightly more copper, manganese, and zinc, while soursop has much more calcium, iron, magnesium, phosphorus, and potassium. One more win for soursop!
Adding up the sections makes for a clear and overwhelming win for soursop, but let’s address to quick safety considerations while we’re here:
- Soursop extract has been claimed to be an effective cancer treatment. It isn’t. There is no evidence for this at all; just one unscrupulous company that spread the claims.
- Soursop contains annonacin, a neurotoxin. That sounds scary, but much like with apple seeds and cyanide, the quantities you’d have to consume to suffer ill effects are absurd. Remember how capsaicin (as found in hot peppers) is also a neurotoxin, too and has many health benefits. Humans have a long and happy tradition of enjoying things that are toxic at high doses, but in small doses are neutral or even beneficial. Pretty much all things we can consume (including oxygen, and water) are toxic at sufficient doses.
In short, both of these fruits are fine and good, neither will treat cancer, but both will help to keep you in good health. As for nutritional density, the soursop wins in every category.
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer ← soursop has no special cancer treatment properties, but actual evidence shows these fruits are beneficial (being good as a preventative, and also definitely a worthy adjunct to—but not a replacement for—mainstream anticancer therapies if you have cancer).
Take care!
Share This Post
Related Posts
-
Celery vs Cucumber – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing celery to cucumber, we picked the celery.
Why?
They are both great, of course! But celery came out on top:
Their macros are very comparable; they’re both 95% water with just enough other things to hold them together, and those other things are in approximately the same proportions in both celery and cucumber.
In the category of vitamins, however, celery has a lot more of vitamins A, B2, B3, B6, B9, E, and K, as well as slightly more vitamin C. Cucumber, meanwhile, only boasts slightly higher vitamin B1.
An easy win for celery on the vitamin front!
Minerals are closer, but celery still comes out on top with its notably higher calcium and potassium content. Cucumber has more iron and zinc, but the margin is smaller.
As a point in cucumber’s favor, it has been noted for its anti-inflammatory effect in ways that celery hasn’t, but we don’t think this is enough to say it wins over celery sweeping the vitamins category and coming out top for minerals too.
However! They are both great, so enjoy them both, of course.
Want to learn more?
You might like to read:
- Cucumber Extract Beats Glucosamine & Chondroitin… At 1/135th Of The Dose?!
- Some Surprising Truths About Hunger And Satiety ← both celery and cucumber are great for this
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why a common asthma drug will now carry extra safety warnings about depression
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Australia’s Therapeutic Goods Administration (TGA) recently issued a safety alert requiring extra warnings to be included with the asthma and hay fever drug montelukast.
The warnings are for users and their families to look for signs of serious behaviour and mood-related changes, such as suicidal thoughts and depression. The new warnings need to be printed at the start of information leaflets given to both patients and health-care providers (sometimes called a “boxed” warning).
So why did the TGA issue this warning? And is there cause for concern if you or a family member uses montelukast? Here’s what you need to know.
First, what is montelukast?
Montelukast is a prescription drug also known by its brand names which include Asthakast, Lukafast, Montelair and Singulair. It’s used to manage the symptoms of mild-to-moderate asthma and seasonal hay fever in children and adults.
Asthma occurs when the airways tighten and produce extra mucus, which makes it difficult to get air into the lungs. Likewise, the runny nose characteristic of hay fever occurs due to the overproduction of mucus.
Leukotrienes are an important family of chemicals found throughout the airways and involved in both mucus production and airway constriction. Montelukast is a cysteinyl leukotriene receptor antagonist, meaning it blocks the site in the airways where the leukotrienes work.
Montelukast can’t be used to treat acute asthma (an asthma attack), as it takes time for the tablet to be broken down in the stomach and for it to be absorbed into the body. Rather, it’s taken daily to help prevent asthma symptoms or seasonal hay fever.
It can be used alongside asthma puffers that contain corticosteriods and drugs like salbutamol (Ventolin) in the event of acute attacks.
What is the link to depression and suicide?
The possibility that this drug may cause behavioural changes is not new information. Manufacturers knew this as early as 2007 and issued warnings for possible side-effects including depression, suicidality and anxiousness.
The United Kingdom’s Medicines and Healthcare products Regulatory Agency has required a warning since 2008 but mandated a more detailed warning in 2019. The United States’ Food and Drug Administration has required boxed warnings for the drug since 2020.
Montelukast can help children and adults with asthma. adriaticfoto/Shutterstock Montelukast is known to potentially induce a number of behaviour and mood changes, including agitation, anxiety, depression, irritability, obsessive-compulsive symptoms, and suicidal thoughts and actions.
Initially a 2009 study that analysed data from 157 clinical trials involving more than 20,000 patients concluded there were no completed suicides due to taking the drug, and only a rare risk of suicide thoughts or attempts.
The most recent study, published in November 2024, examined data from more than 100,000 children aged 3–17 with asthma or hay fever who either took montelukast or used only inhaled corticosteroids.
It found montelukast use was associated with a 32% higher incidence of behavioural changes. The behaviour change with the strongest association was sleep disturbance, but montelukast use was also linked to increases in anxiety and mood disorders.
In the past ten years, around 200 incidences of behavioural side-effects have been reported to the TGA in connection with montelukast. This includes 57 cases of depression, 60 cases of suicidal thoughts and 17 suicide attempts or incidents of intentional self-injury. There were seven cases where patients taking the drug did complete a suicide.
This is of course tragic. But these numbers need to be seen in the context of the number of people taking the drug. Over the same time period, more than 200,000 scripts for montelukast have been filled under the Pharmaceutical Benefits Scheme.
Overall, we don’t know conclusively that montelukast causes depression and suicide, just that it seems to increase the risk for some people.
We’re still not sure how the drug can act on the brain to lead to behaviour changes. Elif Bayraktar/Shutterstock And if it does change behaviour, we don’t fully understand how this happens. One hypothesis is that the drug and its breakdown products (or metabolites) affect brain chemistry.
Specifically, it might interfere with how the brain detoxifies the antioxidant glutathione or alter the regulation of other brain chemicals, such as neurotransmitters.
Why is the TGA making this change now?
The new risk warning requirement comes from a meeting of the Australian Advisory Committee on Medicines where they were asked to provide advice on ways to minimise the risk for the drug given current international recommendations.
Even though the 2024 review didn’t highlight any new risks, to align with international recommendations, and help address consumer concerns, the advisory committee recommended a boxed warning be added to drug information sheets.
If you have asthma and take montelukast (or your child does), you should not just stop taking the drug, because this could put you at risk of an attack that could be life threatening. If you’re concerned, speak to your doctor who can discuss the risks and benefits of the medication for you, and, if appropriate, prescribe a different medication.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14.
Nial Wheate, Professor of Pharmaceutical Chemistry, Macquarie University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Reading At Night: Good Or Bad For Sleep? And Other Questions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Would be interested in your views about “reading yourself to sleep”. I find that current affairs magazines and even modern novels do exactly the opposite. But Dickens – ones like David Copperfield and Great Expectations – I find wonderfully effective. It’s like entering a parallel universe where none of your own concerns matter. Any thoughts on the science that may explain this?!❞
Anecdotally: this writer is (like most writers) a prolific reader, and finds reading some fiction last thing at night is a good way to create a buffer between the affairs of the day and the dreams of night—but I could never fall asleep that way, unless I were truly sleep-deprived. The only danger is if I “one more chapter” my way deep into the night! For what it’s worth, bedtime reading for me means a Kindle self-backlit with low, soft lighting.
Scientifically: this hasn’t been a hugely researched area, but there are studies to work from. But there are two questions at hand (at least) here:
- one is about reading, and
- the other is about reading from electronic devices with or without blue light filters.
Here’s a study that didn’t ask the medium of the book, and concluded that reading a book in bed before going to sleep improved sleep quality, compared to not reading a book in bed:
Here’s a study that concluded that reading on an iPad (with no blue light filter) that found no difference in any metrics except EEG (so, there was no difference on time spent in different sleep states or sleep onset latency), but advised against it anyway because of the EEG readings (which showed slow wave activity being delayed by approximately 30 minutes, which is consistent with melatonin production mechanics):
Here’s another study that didn’t take EEG readings, and/but otherwise confirmed no differences being found:
We’re aware this goes against general “sleep hygiene” advice in two different ways:
- General advice is to avoid electronic devices before bedtime
- General advice is to not do activities besides sleep (and sex) in bed
…but, we’re committed to reporting the science as we find it!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: