Do You Know Which Supplements You Shouldn’t Take Together? (10 Pairs!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. LeGrand Peterson wants us to get the most out of our supplements, so watch out for these…
Time to split up some pairs…
In most cases these are a matter of competing for absorption; sometimes to the detriment of both, sometimes to the detriment of one or the other, and sometimes, the problem is entirely different and they just interact in a way that could potentially cause other problems. Dr. Peterson advises as follows:
- Vitamin C and vitamin B12: taking these together can reduce the absorption of Vitamin B12, as vitamin C can overpower it.
- Vitamin C and copper: high amounts of vitamin C can decrease copper absorption, especially in those who are severely copper deficient.
- Magnesium and calcium: these two minerals compete for absorption in the intestines, potentially reducing the effectiveness of both.
- Calcium and iron: calcium can decrease iron absorption, so they should not be taken together, especially if you are iron deficient.
- Calcium and zinc: calcium also competes with zinc, reducing zinc absorption; they should be taken at different times.
- Zinc and copper: zinc and copper compete for absorption, so they should be taken at separate times.
- Iron and zinc: iron can decrease zinc absorption, and thus, they should not be taken together.
- Iron and green tea: perhaps a surprising one, but green tea can reduce iron absorption, so they should not be taken simultaneously.
- Vitamin E and vitamin K: vitamin E increases bleeding risk, while vitamin K promotes clotting, making them opposites and risky to take together.
- Fish oil and ginkgo biloba: both are anticoagulants and can increase the risk of bleeding, especially if taken with blood thinners like warfarin.
If you need to take supplements that compete (or conflict or otherwise potentially adversely interact) with each other, it’s recommended to separate them by at least 4 hours, or better yet, take one in the morning and the other at night. If in doubt, do speak with your pharmacist or doctor for personalized advice
You may be thinking: half my foods contain half of these nutrients! And yes, assuming you have a nutritionally dense diet, this is probably the case. Foods typically release nutrients more slowly than supplements, and unlike supplements, do not usually contain megadoses (although they can, such as the selenium content of Brazil nuts, or vitamin A in carrots). Basically, food is in most cases safer and gentler than supplements. If concerned, do speak with your nutritionist or doctor for personalized advice.
For more information on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Do We Need Supplements, And Do They Work?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Taurine’s Benefits For Heart Health And More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Taurine: Research Review
First, what is taurine, beyond being an ingredient in many energy drinks?
It’s an amino acid that many animals, including humans, can synthesize in our bodies. Some other animals—including obligate carnivores such as cats (but not dogs, who are omnivorous by nature) cannot synthesize taurine and must get it from food.
So, as humans are very versatile omnivorous frugivores by nature, we have choices:
- Synthesize it—no need for any conscious action; it’ll just happen
- Eat it—by eating meat, which contains taurine
- Supplement it—by taking supplements, including energy drinks, which generally (but not always) use a bioidentical lab-made taurine. Basically, lab-made taurine is chemically identical to the kind found in meat, it’s just cheaper and doesn’t involve animals as a middleman.
What does it do?
Taurine does a bunch of essential things, including:
- Maintaining hydration/electrolyte balance in cells
- Regulating calcium/magnesium balance in cells
- Forming bile salts, which are needed for digestion
- Supporting the integrity of the central nervous system
- Regulating the immune system and antioxidative processes
Thus, a shortage of taurine can lead to such issues as kidney problems, eye tissue damage (since the eyes are a particularly delicate part of the CNS), and cardiomyopathy.
If you want to read more, here’s an academic literature review:
Taurine: A “very essential” amino acid
On the topic of eye health, a 2014 study found that taurine is the most plentiful amino acid in the eye, and helps protect against retinal degeneration, in which they say:
❝We here review the evidence for a role of taurine in retinal ganglion cell survival and studies suggesting that this compound may be involved in the pathophysiology of glaucoma or diabetic retinopathy. Along with other antioxidant molecules, taurine should therefore be seriously reconsidered as a potential treatment for such retinal diseases❞
Read more: Taurine: the comeback of a neutraceutical in the prevention of retinal degenerations
Taurine for muscles… In more than sports!
We’d be remiss not to mention that taurine is enjoyed by athletes to enhance athletic performance; indeed, it’s one of its main selling-points:
See: Taurine in sports and exercise
But! It’s also useful for simply maintaining skeleto-muscular health in general, and especially in the context of age-related decline and chronic disease:
Taurine: the appeal of a safe amino acid for skeletal muscle disorders
On the topic of safety… How safe is it?
There’s an interesting answer to that question. Within safe dose ranges (we’ll get to that), taurine is not only relatively safe, but also, studies that looked to explore its risks found new benefits in the process. Specifically of interest to us were that it appears to promote better long-term memory, especially as we get older (as taurine levels in the brain decline with age):
Taurine, Caffeine, and Energy Drinks: Reviewing the Risks to the Adolescent Brain
^Notwithstanding the title, we assure you, the research got there; they said:
❝Interestingly, the levels of taurine in the brain decreased significantly with age, which led to numerous studies investigating the potential neuroprotective effects of supplemental taurine in several different experimental models❞
What experimental models were those? These ones:
- Taurine protects cerebellar neurons of the external granular layer
- Effects of taurine on alterations of neurobehavior and neurodevelopment key proteins expression
- Neuroprotective role of taurine in developing offspring affected by maternal alcohol consumption
…which were all animal studies, however.
The same systematic review also noted that not only was more research needed on humans, but also, existing studies have had a strong bias to male physiology (in both human and assorted other animal studies), so more diverse study is needed too.
What are the safe dose ranges?
Before we get to toxicity, let’s look at some therapeutic doses. In particular, some studies that found that 500mg 3x daily, i.e. 1.5g total daily, had benefits for heart health:
- Taurine and atherosclerosis
- The Anti-Inflammatory Effect of Taurine on Cardiovascular Disease
- Taurine supplementation has anti-atherogenic and anti-inflammatory effects before and after incremental exercise in heart failure
- Taurine Supplementation Lowers Blood Pressure and Improves Vascular Function in Prehypertension
- Taurine improves the vascular tone through the inhibition of TRPC3 function in the vasculature
Bottom line on safety: 3g/day has been found to be safe:
Share This Post
-
No, you don’t need the ‘Barbie drug’ to tan, whatever TikTok says. Here’s why melanotan-II is so risky
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
TikTok and Instagram influencers have been peddling the “Barbie drug” to help you tan.
But melanotan-II, as it’s called officially, is a solution that’s too good to be true. Just like tanning, this unapproved drug has a dark side.
Doctors, researchers and Australia’s drug regulator have been warning about its side effects – from nausea and vomiting to brain swelling and erection problems.
There are also safer ways of getting the tanned look, if that’s what you’re after.
AtlasStudio/Shutterstock What is melanotan-II?
No, it’s not a typo. Melanotan-II is very different from melatonin, which is a hormonal supplement used for insomnia and jet lag.
Melanotan-II is a synthetic version of the naturally ocurring hormone α-melanocyte stimulating hormone. This means the drug mimics the body’s hormone that stimulates production of the pigment melanin. This is what promotes skin darkening or tanning, even in people with little melanin.
Although the drug is promoted as a way of getting a “sunless tan”, it is usually promoted for use with UV exposure, to enhance the effect of UV and kickstart the tanning process.
Melanotan-II is related to, but different from, melanotan-I (afamelanotide), an approved drug used to treat the skin condition erythropoietic protoporphyria.
Melanotan-II is not registered for use with Australia’s Therapeutic Goods Administration (TGA). It is illegal to advertise it to the public or to provide it without a prescription.
However, social media has been driving unlicensed melanotan-II sales, a study published last year confirms.
There are many black market suppliers of melanotan-II injections, tablets and creams. More recently, nasal sprays have become more popular.
What are the risks?
Just like any drug, melanotan-II comes with the risk of side effects, many of which we’ve known about for more than a decade. These include changes in the size and pigmentation of moles, rapid appearance of new moles, flushing to the face, abdominal cramps, nausea, vomiting, chest pain and brain swelling.
It can also cause rhabdomyolysis, a dangerous syndrome where muscle breaks down and releases proteins into the bloodstream that damage the kidneys.
For men, the drug can cause priapism – a painful erection that does not go away and can damage the penis, requiring emergency treatment.
Its use has been linked with melanoma developing from existing moles either during or shortly after using the drug. This is thought to be due to stimulating pigment cells and causing the proliferation of abnormal cells.
Despite reports of melanoma, according to a study of social media posts the drug is often marketed as protecting against skin cancer. In fact, there’s no evidence to show it does this.
Social media posts about melanotan-II rarely mention health risks.
There are no studies on long-term safety of melanotan-II use.
Then there’s the issue of the drug not held to the high safety standards as TGA-approved products. This could result in variability in dose, undeclared ingredients and potential microbial contamination.
Thinking about melanotan-II? The drug can cause a long-lasting painful erection needing urgent medical care. Eugenio Marongiu/Shutterstock The TGA has previously warned consumers to steer clear of the drug due to its “serious side effects that can be very damaging to your health”.
According to an ABC article published earlier this week, the TGA is cracking down on the illegal promotion of the drug on various websites. However, we know banned sellers can pop back up under a different name.
TikTok has banned the hashtags #tanningnasalspray, #melanotan and #melanotan2, but these products continue to be promoted with more generic hashtags, such as #tanning.
Part of a wider trend
Australia has some of the highest rates of skin cancer in the world. The “slip, slop, slap” campaign is a public health success story, with increased awareness of sun safety, a cultural shift and a decline in melanoma in young people.
However, the image of a bronzed beach body remains a beauty standard, especially among some young people.
Disturbingly, tan lines are trending on TikTok as a sought after summer accessory and the hashtag #sunburnttanlines has millions of views. We’ve also seen a backlash against sunscreen among some young people, again promoted on TikTok.
The Cancer Council is so concerned about the trend towards normalising tanning it has launched the campaign End the Trend.
You have other options
There are options beyond spraying an illegal, unregulated product up your nose, or risking unprotected sun exposure: fake tan.
Fake tan tends to be much safer than melanotan-II and there’s more long-term safety data. It also comes with potential side effects, albeit rare ones, including breathing issues (with spray products) and skin inflammation in some people.
Better still, you can embrace your natural skin tone.
Rose Cairns, Senior Lecturer in Pharmacy, NHMRC Emerging Leadership Fellow, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
My dance school is closed for the summer, how can I keep up my fitness?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Once the end-of-year dance concert and term wrap up for the year it is important to take a break. Both physical and mental rest are important and taking a few weeks off can help your body repair and have a mental break from dance.
If your mind and body are in need of an extended break (such as more than a few weeks), then it’s more than OK to take longer off, especially if you are training at a competitive or pre-professional level.
There is benefit in enjoying other aspects of your life outside of dance such as spending time with family, friends and enjoying hobbies.
Tatyana Vyc/Shutterstock A safe, fulfilling dancing life
Creating meaning and value in life outside of dance and expanding sense of self can make it easier to lean into other aspects when experiencing change or difficult times during dance training such as being injured.
Taking an extended break from dance training will, however, mean losing some fitness and physical capacity. When you return to dance your body will take time to return to full capacity again.
Approaches such as being “whipped back into shape” can promote sudden spikes in training load (hours and intensity of training) which can increase the risk of injury. It is advised to gradually and progressively increase training load over time to allow the body to adapt and return to full capacity safely.
A four-to-six week period of gradually progressing training load and introducing jumping has been suggested in dance settings.
For dancers wanting to maintain fitness over the summer holidays, a great place to start is focusing on building a physical foundation.
Exercise like running can help build a physical foundation. Jacek Chabraszewski/Shutterstock Building a physical foundation means focusing on targeted areas of fitness such as full body strength, cardiovascular fitness or stamina (such as skipping, cycling walking, running, swimming), flexibility, and some dance-specific conditioning (for example, calf rises for ballet).
A good physical foundation will mean an improved capacity and fitness level so your body is ready to take on more challenging dance movements and routines once you return to the studio.
Building full body strength at home or at the park
A great place to start is by choosing movements that require your muscles to work to support your own body weight.
Fundamental movements such as crawling (moving on the floor on hands and feet) and locomotion (travelling movements such as lunging, hopping, sliding) are great for developing body control, arm and leg stability and coordinated movement patterns.
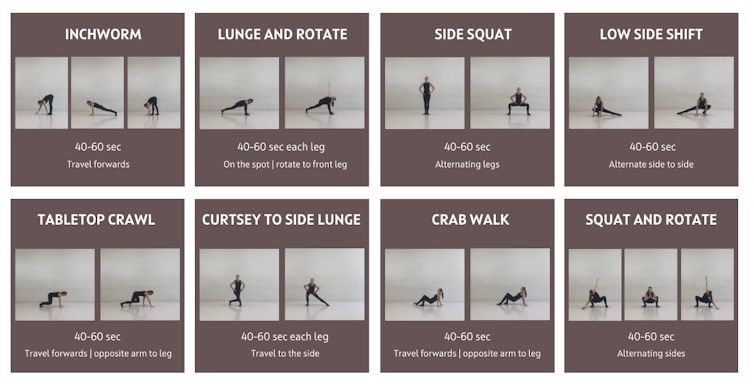
Below is a sequence that can be used as a warm up and even as a workout itself. The ten minute sequence is based on gross motor and fundamental movement patterns. It includes exercises that work through a range of joint movements and in multiple planes (forwards, sideways, rotating).
This fundamental movement sequence can be used as a warm-up or a workout. Joanna Nicholas, CC BY Once feeling comfortable with the above fundamental movements, it is time to introduce body weight resistance exercises.
Body weight resistance exercises can be beneficial for developing a strong foundation for dance movements such as jumping, landing, floorwork, partnering and aerial work.
Exercises from the above sequence can be used to form a safe and effective neuromuscular warm up.
Aim to include one exercise from each of the below movement categories (squat, horizontal push etc) to build your own workout.
Aim to complete two to three sets (or rounds) of each exercise with about one minute rest between sets. An alternative is to complete one set of each exercise with minimal rest between, then complete a second or third time.
If training with friends, you could set a timer and do each exercise for up to 50 seconds (instead of counting reps) and take ten seconds to transition to the next exercise.
Depending on your level of strength you may need to do fewer repetitions and build up sets and repetitions overtime. After you have completed the body weight exercises complete a cool down including stretches for the upper and lower body muscles. Be sure to use a sturdy bar (such as an outdoor fitness station) for horizontal row and overhead hold.
Exercises may need to be modified depending on fitness level and physical limitations such as injury.
You can build your own full body strength workout using these movements. Joanna Nicholas, CC BY How often should I train?
A common misconception in dance is that “more is better”. This belief can lead to dancers training long hours on most or all days of the week which can lead to overtraining, plateauing and increased risk of injury.
Our bodies require sufficient time between training sessions to adapt and get stronger and fitter. The time between sessions is when our muscles and tissues repair and training gains are made.
By incorporating adequate recovery (including sleep and downtime) and including rest days throughout the week, our bodies can gain the most benefits from training.
Rest days are important, too. Manop Boonpeng/Shutterstock Muscles can take up to 48–72 hours to recover from most types of strength-based exercises (the more intense the longer they’ll need to recover).
Aerobic activity at low intensity, such as a brisk walk, can be done most days (24-hour recovery) while high stress anaerobic exercise such as high intensity intervals or sprints can take three days or more to recover from.
Aim to spread training sessions out over the week and allow time to recover between sessions.
Below is an example weekly schedule based on incorporating adequate recovery between sessions, and incorporating polarised training where some days are harder and others are easier.
Seek guidance from your healthcare provider and/or an exercise professional prior to undertaking a new exercise program.
Joanna Nicholas, Lecturer in Dance and Performance Science, Edith Cowan University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Mosquitoes can spread the flesh-eating Buruli ulcer. Here’s how you can protect yourself
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Each year, more and more Victorians become sick with a flesh-eating bacteria known as Buruli ulcer. Last year, 363 people presented with the infection, the highest number since 2004.
But it has been unclear exactly how it spreads, until now. New research shows mosquitoes are infected from biting possums that carry the bacteria. Mozzies spread it to humans through their bite.
What is Buruli ulcer?
Buruli ulcer, also known as Bairnsdale ulcer, is a skin infection caused by the bacterium Mycobacterium ulcerans.
It starts off like a small mosquito bite and over many months, slowly develops into an ulcer, with extensive destruction of the underlying tissue.
While often painless initially, the infection can become very serious. If left untreated, the ulcer can continue to enlarge. This is where it gets its “flesh-eating” name.
Thankfully, it’s treatable. A six to eight week course of specific antibiotics is an effective treatment, sometimes supported with surgery to remove the infected tissue.
Where can you catch it?
The World Health Organization considers Buruli ulcer a neglected tropical skin disease. Cases have been reported across 33 countries, primarily in west and central Africa.
However, since the early 2000s, Buruli ulcer has also been increasingly recorded in coastal Victoria, including suburbs around Melbourne and Geelong.
Scientists have long known Australian native possums were partly responsible for its spread, and suspected mosquitoes also played a role in the increase in cases. New research confirms this.
Our efforts to ‘beat Buruli’
Confirming the role of insects in outbreaks of an infectious disease is achieved by building up corroborating, independent evidence.
In this new research, published in Nature Microbiology, the team (including co-authors Tim Stinear, Stacey Lynch and Peter Mee) conducted extensive surveys across a 350 km² area of Victoria.
We collected mosquitoes and analysed the specimens to determine whether they were carrying the pathogen, and links to infected possums and people. It was like contact tracing for mosquitoes.
Aedes notoscriptus was the mosquito identified as carrying the bacteria that caused Buruli ulcer.
Cameron Webb (NSW Health Pathology)Molecular testing of the mosquito specimens showed that of the two most abundant mosquito species, only Aedes notoscriptus (a widespread species commonly known as the Australian backyard mosquito) was positive for Mycobacterium ulcerans.
We then used genomic tests to show the bacteria found on these mosquitoes matched the bacteria in possum poo and humans with Buruli ulcer.
We further analysed mosquito specimens that contained blood to show Aedes notoscriptus was feeding on both possums and humans.
To then link everything together, geospatial analysis revealed the areas where human Buruli ulcer cases occur overlap with areas where both mosquitoes and possums that harbour Mycobacterium ulcerans are active.
Stop its spread by stopping mozzies breeding
The mosquito in this study primarily responsible for the bacteria’s spread is Aedes notoscriptus, a mosquito that lays its eggs around water in containers in backyard habitats.
Controlling “backyard” mosquitoes is a critical part of reducing the risk of many global mosquito-borne disease, especially dengue and now Buruli ulcer.
You can reduce places where water collects after rainfall, such as potted plant saucers, blocked gutters and drains, unscreened rainwater tanks, and a wide range of plastic buckets and other containers. These should all be either emptied at least weekly or, better yet, thrown away or placed under cover.
Mosquitoes can lay eggs in a wide range of water-filled items in the backyard.
Cameron Webb (NSW Health Pathology)There is a role for insecticides too. While residual insecticides applied to surfaces around the house and garden will reduce mosquito populations, they can also impact other, beneficial, insects. Judicious use of such sprays is recommended. But there are ecological safe insecticides that can be applied to water-filled containers (such as ornamental ponds, fountains, stormwater pits and so on).
Recent research also indicates new mosquito-control approaches that use mosquitoes themselves to spread insecticides may soon be available.
How to protect yourself from bites
The first line of defence will remain personal protection measures against mosquito bites.
Covering up with loose fitted long sleeved shirts, long pants, and covered shoes will provide physical protection from mosquitoes.
Applying topical insect repellent to all exposed areas of skin has been proven to provide safe and effective protection from mosquito bites. Repellents should include diethytolumide (DEET), picaridin or oil of lemon eucalyptus.
While the rise in Buruli ulcer is a significant health concern, so too are many other mosquito-borne diseases. The steps to avoid mosquito bites and exposure to Mycobacteriam ulcerans will also protect against viruses such as Ross River, Barmah Forest, Japanese encephalitis, and Murray Valley encephalitis.
Cameron Webb, Clinical Associate Professor and Principal Hospital Scientist, University of Sydney; Peter Mee, Adjunct Associate Lecturer, School of Applied Systems Biology, La Trobe University; Stacey Lynch, Team Leader- Mammalian infection disease research, CSIRO, and Tim Stinear, Professor of Microbiology, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
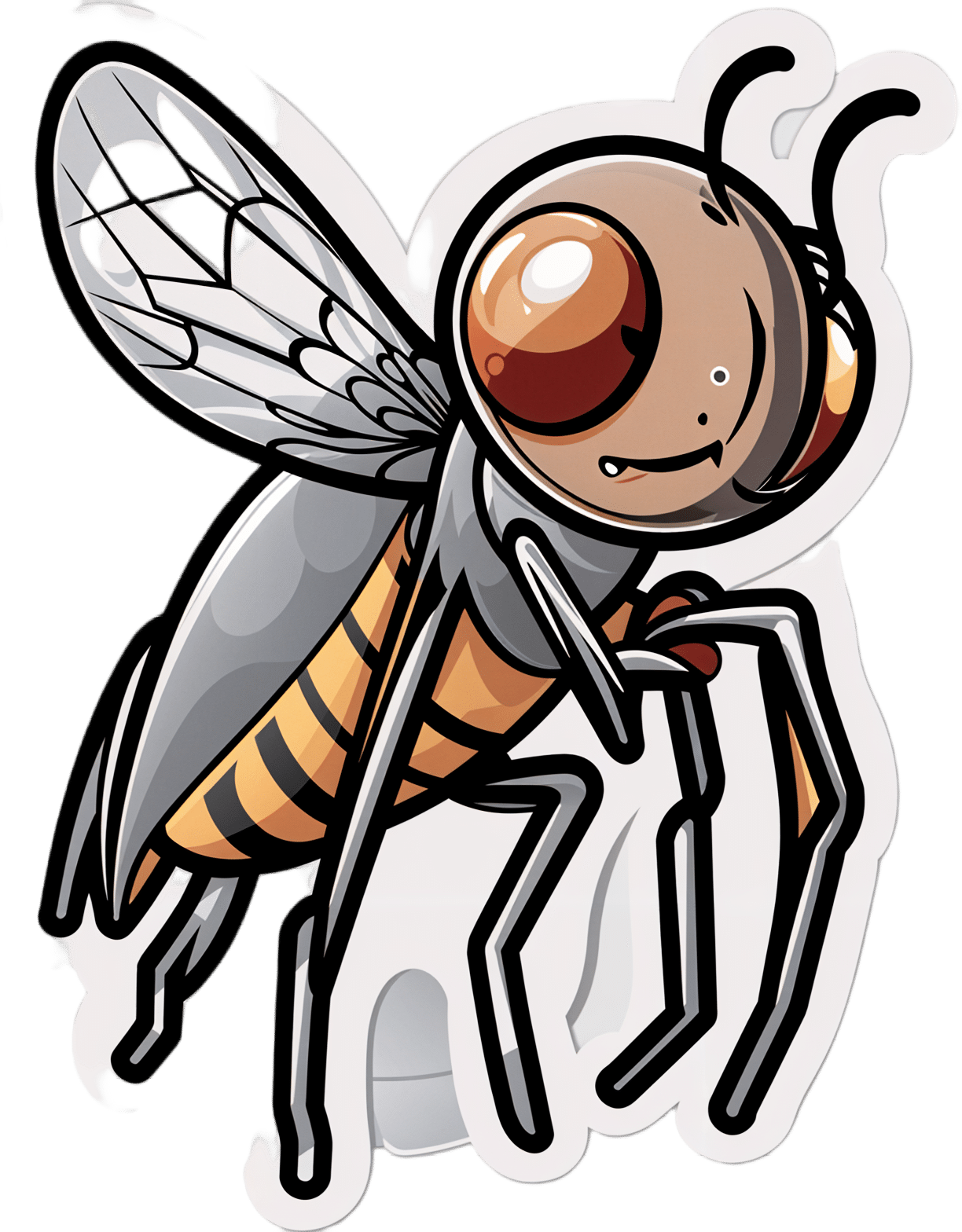
Dr. Patrick Walsh’s Guide to Surviving Prostate Cancer – by Dr. Patrick Walsh & Janet Farrar Worthington
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Prostate cancer is not glamorous or fun, and neither is this book.
Nevertheless, it’s a disease that affects 12% of men in general, and 60% of men aged 60+, with that percentage climbing every year after that.
So, if you have a prostate or love someone who has one, this book is worthwhile reading—yes, even as a preventative.
Like many cancers, prostate cancer is easy to treat if caught very early, becomes harder to treat as it goes, and almost impossible to cure if it gets as far as metastasis (i.e., it spread). Like all cancers, it’s better off avoided entirely if possible.
This book covers all the stages:
- How to avoid it
- How to check for it
- How to “nip it in the bud”
- Why some might want to delay treatment (!)
- What options are available afterwards
This latter is quite extensive, and covers not just surgery, but radiation, thermo- or cryoablation, and hormone therapy.
And as for surgery, not just “remove the tumor”, but other options like radical prostatectomy, and even orchiectomy. Not many men will choose to have their testicles removed to stop them from feeding the prostate, but the point is that this book is comprehensive.
It’s asking whenever possible “is there another option?” and exploring all options, with information and without judgment, at each stage.
The writing style (likely co-author Worthington’s influence; she is an award-winning science-writer) is very “for the layman”, and that’s really helpful in demystifying a lot of what can be quite opaque in the field of oncology.
Bottom line: absolutely not an enjoyable read, but a potentially lifesaving one, especially given the odds we mentioned up top.
Click here to check out Dr. Patrick Walsh’s Guide To Surviving Prostate Cancer, and be prepared!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Do We Need Supplements, And Do They Work?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Does our diet need a little help?
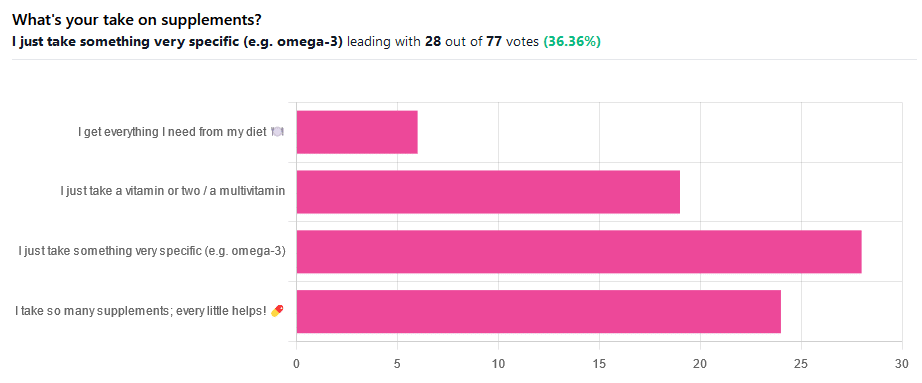
We asked you for your take on supplements, and got the above-illustrated, below-described set of results.
- The largest minority of respondents (a little over a third) voted for “I just take something very specific”
- The next most respondents voted for “I take so many supplements; every little helps!”
- Almost as many voted for “I just take a vitamin or two / a multivitamin”
- Fewest, about 8%, voted for “I get everything I need from my diet”
But what does the science say?
Food is less nutritious now than it used to be: True or False?
True or False depending on how you measure it.
An apple today and an apple from a hundred years ago are likely to contain the same amounts of micronutrients per apple, but a lower percentage of micronutrients per 100g of apple.
The reason for this is that apples (and many other food products; apples are just an arbitrary example) have been selectively bred (and in some cases, modified) for size, and because the soil mineral density has remained the same, the micronutrients per apple have not increased commensurate to the increase in carbohydrate weight and/or water weight. Thus, the resultant percentage will be lower, despite the quantity remaining the same.
We’re going to share some science on this, and/but would like to forewarn readers that the language of this paper is a bit biased, as it looks to “debunk” claims of nutritional values dropping while skimming over “yes, they really have dropped percentage-wise” in favor of “but look, the discrete mass values are still the same, so that’s just a mathematical illusion”.
The reality is, it’s no more a mathematical illusion than is the converse standpoint of saying the nutritional value is the same, despite the per-100g values dropping. After all, sometimes we eat an apple as-is; sometimes we buy a bag of frozen chopped fruit. That 500g bag of chopped fruit is going to contain less copper (for example) than one from decades past.
Here’s the paper, and you’ll see what we mean:
Supplements aren’t absorbed properly and thus are a waste of money: True or False?
True or False depending on the supplement (and your body, and the rest of your diet)
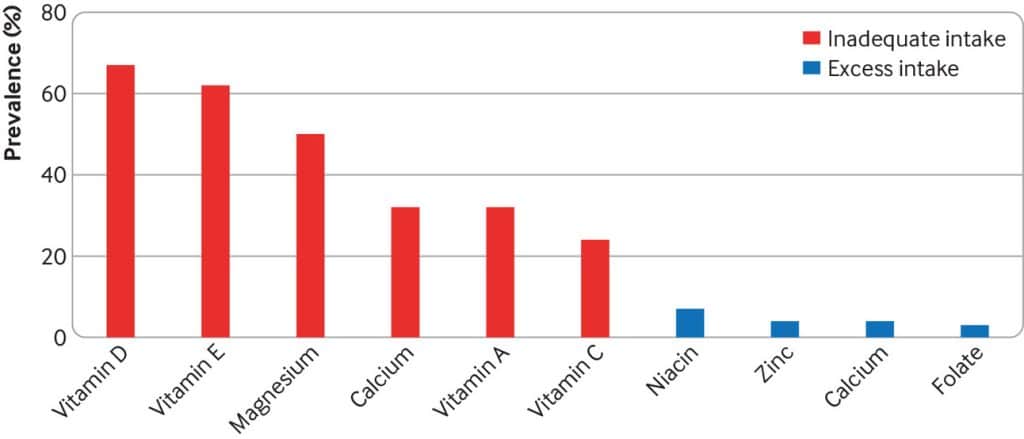
Many people are suffering from dietary deficiencies of vitamins and minerals, that could be easily correctable by supplementation:
However, as this study by Dr. Fang Fang Zhang shows, a lot of vitamin and mineral supplementation does not appear to have much of an effect on actual health outcomes, vis-à-vis specific diseases. She looks at:
- Cardiovascular disease
- Cancer
- Type 2 diabetes
- Osteoporosis
Her key take-aways from this study were:
- Randomised trial evidence does not support use of vitamin, mineral, and fish oil supplements to reduce the risk of non-communicable diseases
- People using supplements tend to be older, female, and have higher education, income, and healthier lifestyles than people who do not use them
- Use of supplements appreciably reduces the prevalence of inadequate intake for most nutrients but also increases the prevalence of excess intake for some nutrients
- Further research is needed to assess the long term effects of supplements on the health of the general population and in individuals with specific nutritional needs, including those from low and middle income countries
Read her damning report: Health effects of vitamin and mineral supplements
On the other hand…
This is almost entirely about blanket vitamin-and-mineral supplementation. With regard to fish oil supplementation, many commercial fish oil supplements break down in the stomach rather than the intestines, and don’t get absorbed well. Additionally, many people take them in forms that aren’t pleasant, and thus result in low adherence (i.e., they nominally take them, but in fact they just sit on the kitchen counter for a year).
One thing we can conclude from this is that it’s good to check the science for any given supplement before taking it, and know what it will and won’t help for. Our “Monday Research Review” editions of 10almonds do this a lot, although we tend to focus on herbal supplements rather than vitamins and minerals.
We can get everything we need from our diet: True or False?
Contingently True (but here be caveats)
In principle, if we eat the recommended guideline amounts of various macro- and micro-nutrients, we will indeed get all that we are generally considered to need. Obviously.
However, this may come with:
- Make sure to get enough protein… Without too much meat, and also without too much carbohydrate, such as from most plant sources of protein
- Make sure to get enough carbohydrates… But only the right kinds, and not too much, nor at the wrong time, and without eating things in the wrong order
- Make sure to get enough healthy fats… Without too much of the unhealthy fats that often exist in the same foods
- Make sure to get the right amount of vitamins and minerals… We hope you have your calculators out to get the delicate balance of calcium, magnesium, potassium, phosphorus, and vitamin D right.
That last one’s a real pain, by the way. Too much or too little of one or another and the whole set start causing problems, and several of them interact with several others, and/or compete for resources, and/or are needed for the others to do their job.
And, that’s hard enough to balance when you’re taking supplements with the mg/µg amount written on them, never mind when you’re juggling cabbages and sardines.
On the topic of those sardines, don’t forget to carefully balance your omega-3, -6, and -9, and even within omega-3, balancing ALA, EPA, and DHA, and we hope you’re juggling those HDL and LDL levels too.
So, when it comes to getting everything we need from our diet, for most of us (who aren’t living in food deserts and/or experiencing food poverty, or having a medical condition that restricts our diet), the biggest task is not “getting enough”, it’s “getting enough of the right things without simultaneously overdoing it on the others”.
With supplements, it’s a lot easier to control what we’re putting in our bodies.
And of course, unless our diet includes things that usually can’t be bought in supermarkets, we’re not going to get the benefits of taking, as a supplement, such things as:
Etc.
So, there definitely are supplements with strong science-backed benefits, that probably can’t be found on your plate!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: