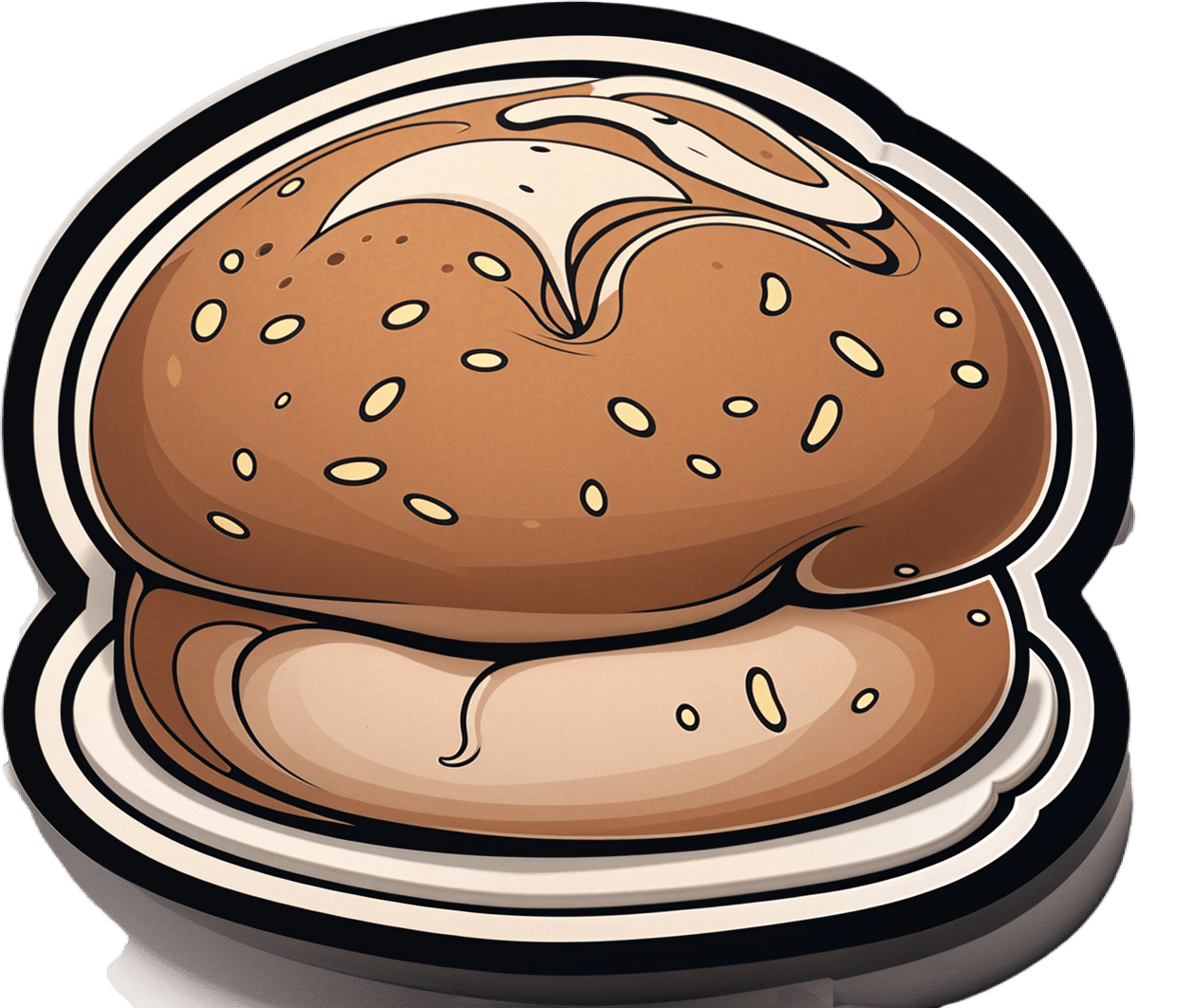
Delicious Quinoa Avocado Bread
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
They’re gluten-free, full of protein and healthy fats, generous with the fiber, easy to make, and tasty too! What’s not to love? Keep this recipe (and its ingredients) handy for next time you want healthy burger buns or similar:
You will need
- 2½ cups quinoa flour
- 2 cups almond flour (if allergic, just substitute more quinoa flour)
- 1 avocado, peeled, pitted, and mashed
- zest and juice of 1 lime
- 2 tbsp ground flaxseed
- 1 tsp baking powder
- ½ tsp MSG or 1 tsp low-sodium salt
- Optional: seeds, oats, or similar for topping the buns
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 350℉/175℃.
2) Mix the flaxseed with ⅓ cup warm water and set aside.
3) Mix, in a large bowl, the quinoa flour and almond flour with the baking powder and the MSG or salt.
4) Mix, in a separate smaller bowl, the avocado and lime.
5) Add the wet ingredients to the dry, slowly, adding an extra ½ cup water as you do, and knead into a dough.
6) Divide the dough into 4 equal portions, each shaped into a ball and then slightly flattened, to create a burger bun shape. If you’re going to add any seeds or similar as a topping, add those now.
7) Bake them in the oven (on a baking sheet lined with baking paper) for 20–25 minutes. You can check whether they’re done the same way you would a cake, by piercing them to the center with a toothpick and seeing whether it comes out clean.
8) Serve when sufficiently cooled.

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Gluten: What’s The Truth?
- Why You Should Diversify Your Nuts!
- Monosodium Glutamate: Sinless Flavor-Enhancer Or Terrible Health Risk?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Holy Basil: What Does (And Doesn’t) It Do?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, a quick clarification:
- Ocimum sanctum is the botanical name given to what in English we call holy basil, and is what we will be discussing today. It’s also called “tulsi“, so if you see that name around, it is the same plant.
- Ocimum basilicum is the botanical name given to culinary basil, the kind you will find in your local supermarket. This one looks similar, but it has a different taste (culinary basil is sweeter) and a different phytochemical profile, and is certainly not the same plant.
We have touched on holy basil before, in our article:
Herbs For Evidence-Based Health & Healing
…where we listed that it helps boost immunity, per:
It’s popularly also consumed in the hopes of getting many other benefits, including:
- Calming effects on the mood (anti-stress)
- Accelerated wound-healing
- Anticancer activity
So, does it actually do those things?
Against stress
We literally couldn’t find anything. It’s often listed as being adaptogenic (reduces stress) in the preamble part of a given paper’s abstract, but we could find no study in any reputable journal that actually tested its effects against stress, and any citations for the claim just link to other papers that also include it in the preamble—and while “no original research” is a fine policy for, say, Wikipedia, it’s not a great policy when it comes to actual research science.
So… It might! There’s also no research (that we could find) showing that it doesn’t work. But one cannot claim something works on the basis of “we haven’t proved it doesn’t”.
For wound healing
Possibly! We found one (1) paper with a small (n=29) sample, and the results were promising, but that sample size of 29 was divided between three groups: a placebo control, holy basil, and another herb (which latter worked less well). So the resultant groups were tiny, arguably to the point of statistical insignificance. However, taking the study at face value and ignoring the small sample size, the results were very promising, as the holy basil group enjoyed a recovery in 4 weeks, rather than the 5 weeks recovery time of the control group:
Herbal remedies for mandibular fracture healing
An extra limitation that’s worth noting, though, is that healing bone is not necessarily the same as healing other injuries in all ways, so the same results might not be replicated in, say, organ or tissue injuries.
Against cancer
This time, there’s lots of evidence! Its mechanism of action appears to be severalfold:
- Anti-inflammatory
- Antioxidant
- Antitumor
- Chemopreventive
Because of the abundance of evidence (including specifically against skin cancer, lung cancer, breast cancer, and more), we could list studies all day here, but instead we’ll just link this one really good research review that has a handy navigation menu on the right, where you can see how it works in each of the stated ways.
Here’s the paper:
An Update on the Therapeutic Anticancer Potential of Ocimum sanctum L.: “Elixir of Life”
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Enjoy!
Share This Post
-
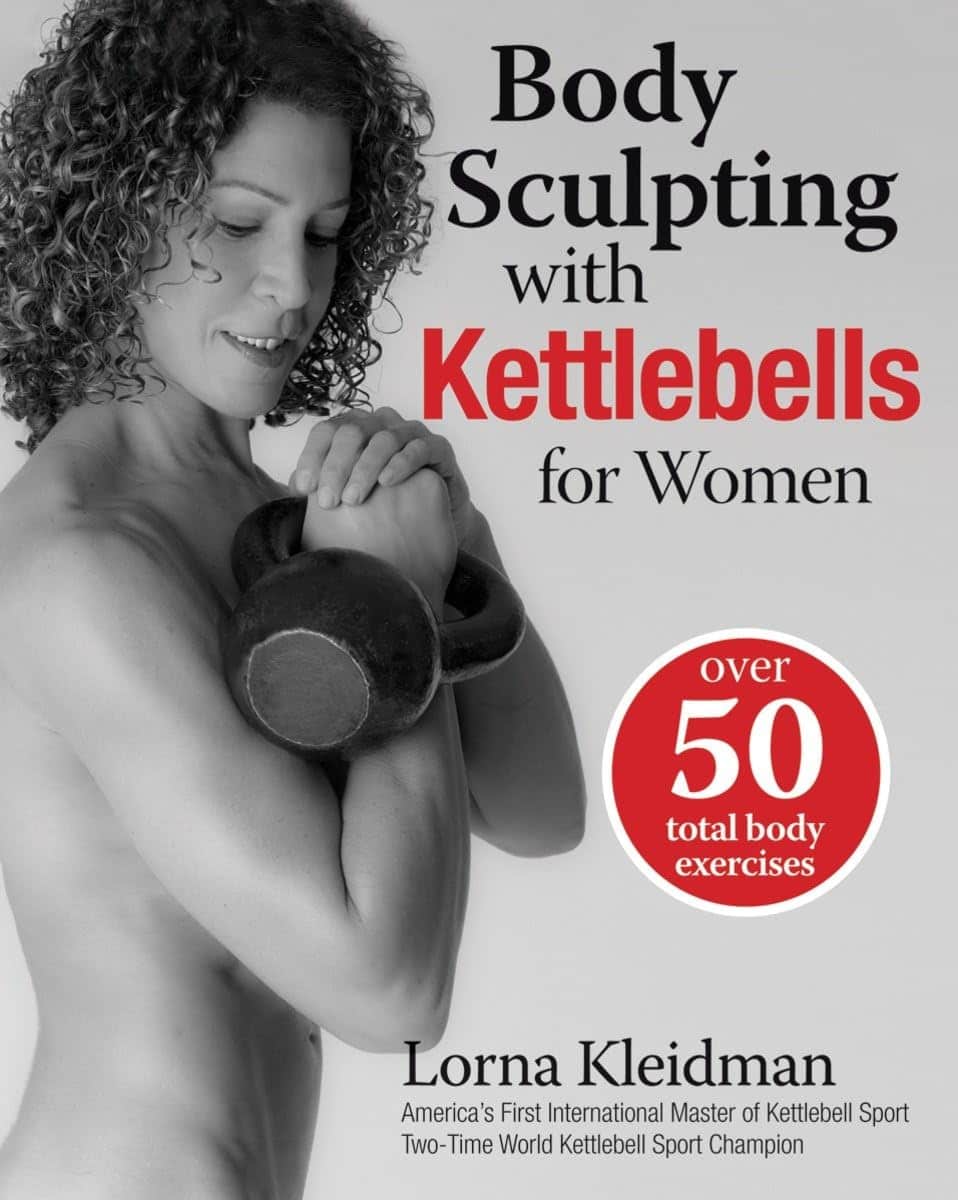
Body Sculpting with Kettlebells for Women – by Lorna Kleidman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For those of us who are more often lifting groceries or pots and pans than bodybuilding trophies, kettlebells provide a way of training functional strength. This book does (as per the title) offer both sides of things—the body sculpting, and thebody maintenance free from pain and injury.
Kleidman first explains the basics of kettlebell training, and how to get the most from one’s workouts, before discussing what kinds of exercises are best for which benefits, and finally moving on to provide full exercise programs.
The exercise programs themselves are fairly comprehensive without being unduly detailed, and give a week-by-week plan for getting your body to where you want it to be.
The style is fairly personal and relaxed, while keeping things quite clear—the photographs are also clear, though if there’s a weakness here, it’s that we don’t get to see which muscles are being worked in the same as we do when there’s an illustration with a different-colored part to show that.
Bottom line: if you’re looking for an introductory course for kettlebell training that’ll take you from beginner through to the “I now know what I’m doing and can take it from here, thanks” stage.
Click here to check out Body Sculpting With Kettlebells For Women, and get sculpting!
Share This Post
-
Eggplant vs Zucchini – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing eggplant to zucchini, we picked the zucchini.
Why?
In terms of macros, eggplant has more carbs and fiber while zucchini has more protein; we’ll generally prioritize fiber, so call this a subjective win for eggplant in this category, though an argument could be made for a tie.
In the category of vitamins, eggplant has more of vitamins B3, B5, and E, while zucchini has more of vitamins A, B1, B2, B6, B9, C, K, and choline, scoring a win for zucchini here.
Looking at minerals, eggplant has more copper, manganese, and selenium, while zucchini has more calcium, iron, magnesium, phosphorus, potassium and zinc, meaning another win for zucchini in this round.
In terms of polyphenols, eggplant has a greater variety of polyphenols, while zucchini has greater total mass of polyphenols, so we’re calling this one a tie.
Adding up the sections makes for an overall win for zucchini, but by all means enjoy either or both (perhaps together!); diversity is good!
Want to learn more?
You might like:
What’s Your Plant Diversity Score?
Enjoy!
Share This Post
Related Posts
-
Singledom & Healthy Longevity
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Statistically, those who live longest, do so in happy, fulfilling, committed relationships.
Note: happy, fulfilling, committed relationships. Less than that won’t do. Your insurance company might care about your marital status for its own sake, but your actual health doesn’t—it’s about the emotional safety and security that a good, healthy, happy, fulfilling relationship offers.
We wrote about this here:
Only One Kind Of Relationship Promotes Longevity This Much!
But that’s not the full story
For a start, while being in a happy fulfilling committed relationship statistically adds healthy life years, being in a relationship that falls short of those adjectives certainly does not. See also:
Relationships: When To Stick It Out & When To Call It Quits
But also, life satisfaction steadily improves with age, for single people (the results are more complicated for partnered people—probably because of the range of difference in quality of relationships). At least, this held true in this large (n=6,188) study of people aged 40–85 years:
❝With advancing age, partnership status became less predictive of loneliness and the satisfaction with being single increased. Among later-born cohorts, the association between partnership status and loneliness was less strong than among earlier-born cohorts. Later-born single people were more satisfied with being single than their earlier-born counterparts.❞
Note that this does mean that while life satisfaction indeed improves with age for single people, that’s a generalized trend, and the greatest life satisfaction within this set of singles comes hand-in-hand with being single by choice rather than by perceived obligation, i.e., those who are “single and not looking” will generally be the most content, and this contentedness will improve with age, but for those who are “single and looking”, in that case it’s the younger people who have it better, likely due to a greater sense of having plenty of time.
For that matter, gender plays a role; this large survey of singles found that (despite the popular old pop-up ads advising that “older women in your area are looking to date”), in reality older single women were the least likely to actively look for a partner:
See: A Profile Of Single Americans
…which also shows that about half of single Americans are “not looking”, and of those who are, about half are open to a serious relationship, though this is more common under the age of 40, while being over the age of 40 sees more people looking only for something casual.
Take-away from this section: being single only decreases life satisfaction if one doesn’t enjoy being single, and even then, and increases it if one does enjoy being single.
But that’s about life satisfaction, not longevity
We found no studies specifically into longevity of singledom, only the implications that may be drawn from the longevity of partnered people.
However, there is a lot of research that shows it’s not being single that kills, it’s being socially isolated. It’s a function of neurodegeneration from a lack of conversation, and it’s a function of what happens when someone slips in the shower and is found a week later. Things like that.
For example: Is Living Alone “Aging Alone”? Solitary Living, Network Types, and Well-Being
What if you are alone and don’t want to be?
We’ve not, at time of writing, written dating advice in our Psychology Sunday section, but this writer’s advice is: don’t even try.
That’s not nihilism or even cynicism, by the way; it’s actually a kind of optimism. The trick is just to let them come to you.
(sample size of one here, but this writer has never looked for a relationship in her life, they’ve always just found me, and now that I’m widowed and intend to remain single, I still get offers—and no, I’m not a supermodel, nor rich, nor anything like that)
Simply: instead of trying to find a partner, just work on expanding your social relationships in general (which is much easier, because the process is something you can control, whereas the outcome of trying to find a suitable partner is not), and if someone who’s right for you comes along, great! If not, then well, at least you have a flock of friends now, and who knows what new unexpected romance may lie around the corner.
As for how to do that,
How To Beat Loneliness & Isolation
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
You Are Not a Before Picture – by Alex Light
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s that time of year, and many of us are looking at what we’ll do in the coming days, weeks, and months to level-up our health. So… Is this a demotivational book?
Quite the opposite! It’s rather a case of an often much-needed reminder to ensure that our plans are really our own, and really are what’s best for us. Why wouldn’t they be, you ask?
Much of diet culture (ubiquitous! From magazine covers to movie stars to the models advertising anything from health insurance to water filters) has us reaching for “body goals” that are not possible without a different skeleton and genes and compromises and post-production edits.
Alex Light—herself having moved from the fashion and beauty industry into health education—sets out in a clear, easy-reading manner, how we can look after ourselves, not be neglectful of our bodies, and/but also not get distracted into unhelpful, impossible, castles-in-the-air.
Bottom line: you cannot self-hate your way into good health, and good health will always be much more attainable than a body that’s just not yours. This book can help you sort out which is which.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
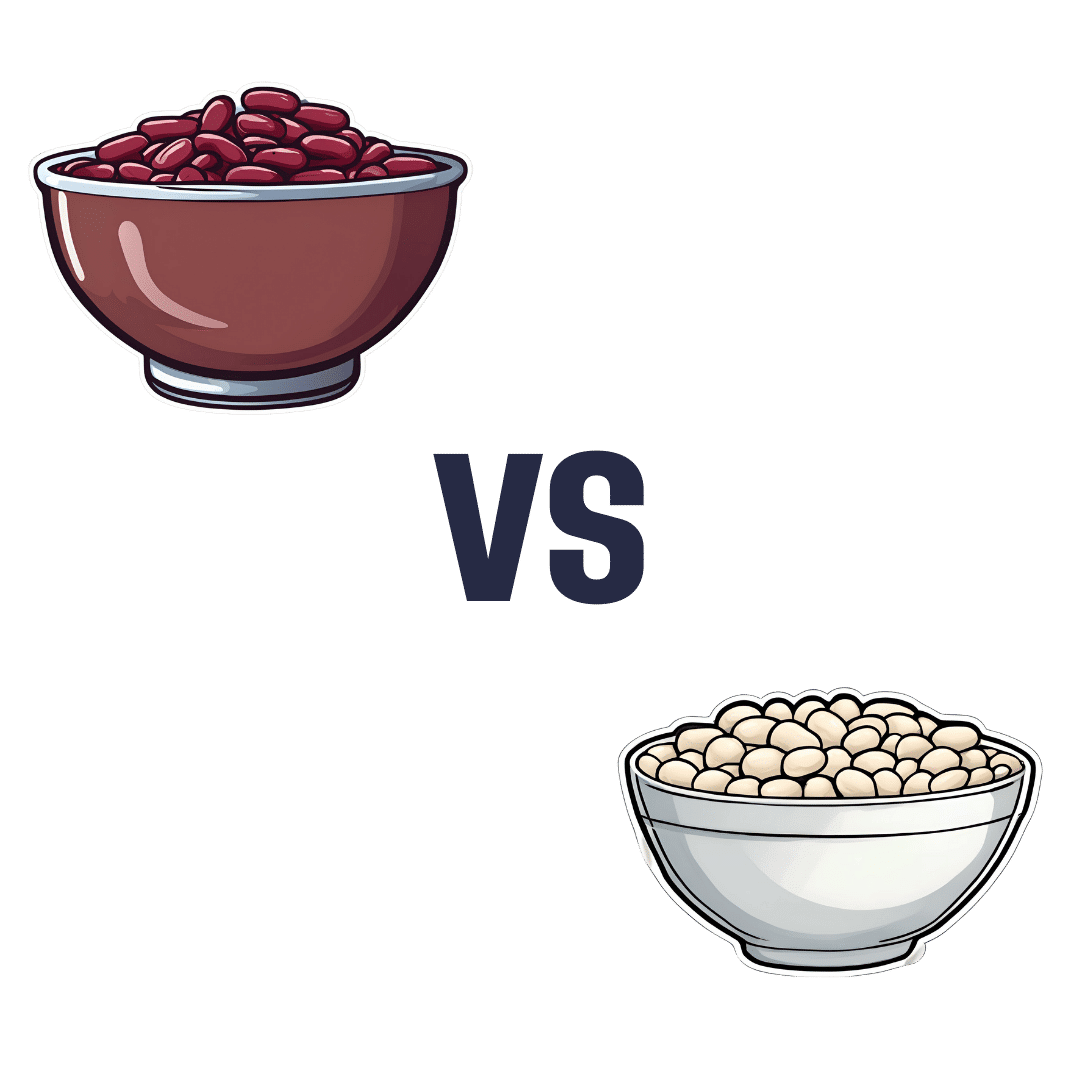
Kidney Beans vs White Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing kidney beans to white beans, we picked the white.
Why?
It was close, and each has its strengths! Bear in mind, these are very closely-related beans. But as we say, there are distinguishing factors…
In terms of macros, kidney beans have very slightly more fiber and white beans have very slightly more protein. But both are close enough in both of those things to call this a tie in this category.
When it comes to vitamins, there are two ways of looking at this:
- kidney beans have more of vitamins B1, B2, B3, B6, B9, C, and K, while white beans have more vitamin B5, E, and choline
- kidney beans have slightly more of some vitamins that don’t usually see a deficiency, while white beans have 31x more vitamin E
Nevertheless, we’re sticking by our usual method of noting that this is a 7:3 win for kidney beans in this category; we just wanted to note that in practical health terms, an argument can be made for white beans on the vitamin front too.
In the category of minerals, kidney beans have slightly more phosphorus, while white beans have more calcium, copper, iron, magnesium, manganese, potassium, selenium, and zinc. An easy win for white beans this time.
(In case you’re wondering about the margin on phosphorus, it was 0.2x more, so we’re not seeing a situation like white beans’ 31x more vitamin E)
In short: both are great and both have their strengths. Enjoy both, together if you like! But if we have to pick one, we’re going with white beans.
Want to learn more?
You might like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: