Daily Activity Levels & The Measurable Difference They Make To Brain Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most studies into the difference that exercise makes to cognitive decline are retrospective, i.e. they look backwards in time, asking participants what their exercise habits were like in the past [so many] years, and tallying that against their cognitive health in the present.
Some studies are interventional, and those are most often 3, 6, or 12 months, depending on funding. In those cases, they make a hypothesis (e.g. this intervention will boost this measure of brain health) and then test it.
However, humans aren’t generally great at making short term decisions for long term gains. In other words: if it’s rainy out, or you’re a little pushed for time, you’re likely to take the car over walking regardless of what data point this adjusts in an overarching pattern that will affect your brain’s amyloid-β clean-up rates in 5–20 years time.
Nine days
The study we’re going to look at today was a 9-day observational study, using smartphone-based tracking with check-ins every 3½ hours, with participants reporting their physical activity as light, moderate, or intense (these terms were defined and exemplified, so that everyone involved was singing from the same songsheet in terms of what activities constitute what intensity).
The sample size was reasonable (n=204) and was generally heterogenous sample (i.e. varied in terms of sex, racial background, and fitness level) of New Yorkers aged 40–65.
So, the input variable was activity level, and the output variable was cognitive fitness.
As to how they measured the output, two brain games assessed:
- cognitive processing speed, and
- working memory (a proxy for executive function).
What they found:
- participants active within the last 3½ hours had faster processing speed, equivalent to being four years younger
- response times in the working memory (for: executive function) task reflected similar processing speed improvements, for participants active in the last 3½ hours
And, which is important to note,
❝This benefit was observed regardless of whether the activities they reported were higher intensity (e.g., running/jogging) or lower intensity (e.g., walking, chores).❞
Source: Cognitive Health Benefits of Everyday Physical Activity in a Diverse Sample of Middle-Aged Adults
Practical take-away:
Move more often! At least every couple of hours (when not sleeping)!
The benefits will benefit you in the now, as well as down the line.
See also:
The Doctor Who Wants Us To Exercise Less, & Move More
and, for that matter:
Do You Love To Go To The Gym? No? Enjoy These “No-Exercise Exercises”!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Infections Here, Infections There…
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This week in health news, let’s take a look at infections outside and in, and how to walk away from it all (in a good way):
The bird that flu away
This one cannot be described as good news. Basically, bird flu is now already epidemic amongst cows in the US, with 845 herds (not 845 cows; 845 herds) testing positive across 16 states. The US Department of Agriculture earlier this month announced a federal order to test milk nationwide. Researchers welcomed the news, but said it should have happened months ago—before the virus was so entrenched. It currently has a fatality rate of 2–5% in cows; we don’t have enough data to reasonably talk about its fatality rate in humans—yet.
❝It’s disheartening to see so many of the same failures that emerged during the COVID-19 crisis re-emerge❞
~ Tom Bollyky, director of the Global Health Program at the Council on Foreign Relations
Read in full: How America lost control of the bird flu, setting the stage for another pandemic
Related: Cows’ Milk, Bird Flu, & You
Alzheimer’s from the gut upwards
Alzheimer’s is generally thought of as being a purely brain thing, but there’s a link between a [specific] chronic gut infection, and the development of Alzheimer’s disease. This infection is called human cytomegalovirus, or HCMV for short, and usually we’ve all been exposed to it by young adulthood. However, for some people, it lingers in an active state in the gut, wherefrom it may travel to the brain via the vagus nerve “gut-brain highway”. And once there, well, you can guess the rest:
Read in full: The surprising role of gut infection in Alzheimer’s disease
Related: How To Reduce Your Alzheimer’s Risk
Walking back to happiness
Analyzing data from 96,138 adults around the world, showed that more steps meant less depression for participants.
You may be thinking “well yes, depressed people walk less”, but more specifically, increases in activity showed increases in anti-depressive benefits, with even small incremental increases showing correspondingly incremental benefits. Specifically, each additional 1,000 steps per day corresponded to a 9% reduction in depression:
Read in full: Higher daily step counts associated with fewer depressive symptoms
Related: Walking… Better.
Take care!
Share This Post
-
How To Reduce The Harm Of Festive Drinking (Without Abstaining)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Reduce The Harm Of Festive Drinking
Not drinking alcohol is—of course—the best way to avoid the harmful effects of alcohol. However, not everyone wants to abstain, especially at this time of year, so today we’re going to be focusing on harm reduction without abstinence.
If you do want to quit (or even reduce) drinking, you might like our previous article about that:
For everyone else, let’s press on with harm reduction:
Before You Drink
A common (reasonable, but often unhelpful) advice is “set yourself a limit”. The problem with this is that when we’re sober, “I will drink no more than n drinks” is easy. After the first drink, we start to feel differently about it.
So: delay your first drink of the day for as long as possible
That’s it, that’s the tip. The later you start drinking, not only will you likely drink less, but also, your liver will have had longer to finish processing whatever you drank last night, so it’s coming at the new drink(s) fresh.
On that note…
Watch your meds! Often, especially if we are taking medications that also tax our liver (acetaminophen / paracetamol / Tylenol is a fine example of this), we are at risk of having a bit of a build-up, like an office printer that still chewing on the last job while you’re trying to print the next.
Additionally: do indeed eat before you drink.
While You Drink
Do your best to drink slowly. While this can hit the same kind of problem as the “set yourself a limit” idea, in that once you start drinking you forget to drink slowly, it’s something to try for.
If your main reason for drinking is the social aspect, then merely having a drink in your hand is generally sufficient. You don’t need to be keeping pace with anyone.
It is further good to alternate your drinks with water. As in, between each alcoholic drink, have a glass of water. This helps in several ways:
- Hydrates you, which is good for your body’s recovery abilities
- Halves the amount of time you spend drinking
- Makes you less thirsty; it’s easy to think “I’m thirsty” and reach for an alcoholic drink that won’t actually help. So, it may slow down your drinking for that reason, too.
At the dinner table especially, it’s very reasonable to have two glasses, one filled with water. Nobody will be paying attention to which glass you drink from more often.
After You Drink
Even if you are not drunk, assume that you are.
Anything you wouldn’t let a drunk person in your care do, don’t do. Now is not the time to drive, have a shower, or do anything you wouldn’t let a child do in the kitchen.
Hospital Emergency Rooms, every year around this time, get filled up with people who thought they were fine and then had some accident.
The biggest risks from alcohol are:
- Accidents
- Heart attacks
- Things actually popularly associated with alcohol, e.g. alcohol poisoning etc
So, avoiding accidents is as important as, if not more important than, avoiding damage to your liver.
Drink some water, and eat something.
Fruit is great, as it restocks you on vitamins, minerals, and water, while being very easy to digest.
Go to bed.
There is a limit to how much trouble you can get into there. Sleep it off.
In the morning, do not do “hair of the dog”; drinking alcohol will temporarily alleviate a hangover, but only because it kicks your liver back into an earlier stage of processing the alcohol—it just prolongs the inevitable.
Have a good breakfast, instead. Remember, fruit is your friend (as explained above).
Want to know more?
Here’s a great service with a lot of further links to a lot more resources:
With You | How to safely detox from alcohol at home
Take care!
Share This Post
-
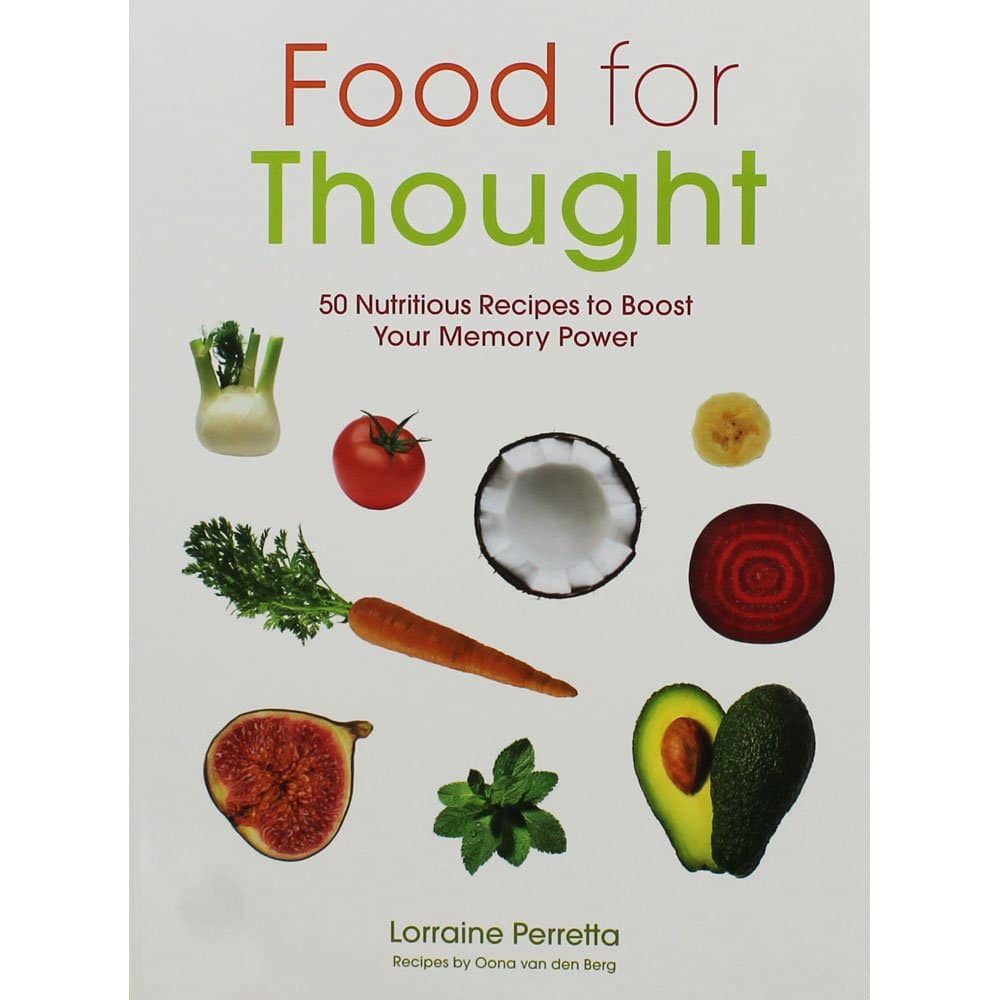
Food for Thought – by Lorraine Perretta
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What are “brain foods”? If you think for a moment, you can probably list a few. What this book does is better.
As well as providing the promised 50 recipes (which themselves are varied, good, and easy), Perretta explains the science of very many brain-healthy ingredients. Not just that, but also the science of a lot of brain-unhealthy ingredients. In the latter case, probably things you already knew to stay away from, but still, it’s a good reminder of one more reason why.
Nor does she merely sort things into brain-healthy (or brain-unhealthy, or brain-neutral), but rather she gives lists of “this for memory” and “this against depression” and “this for cognition” and “this against stress” and so forth.
Perhaps the greatest value of this book is in that; her clear explanations with science that’s simplified but not dumbed down. The recipes are definitely great too, though!
Bottom line: if you’d like to eat more for brain health, this book will give you many ways of doing so
Click here to check out Food for Thought, and upgrade your recipes!
Share This Post
Related Posts
-
Men have a biological clock too. Here’s what’s more likely when dads are over 50
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We hear a lot about women’s biological clock and how age affects the chance of pregnancy.
New research shows men’s fertility is also affected by age. When dads are over 50, the risk of pregnancy complications increases.
Data from more than 46 million births in the United States between 2011 and 2022 compared fathers in their 30s with fathers in their 50s.
While taking into account the age of the mother and other factors known to affect pregnancy outcomes, the researchers found every ten-year increase in paternal age was linked to more complications.
The researchers found that compared to couples where the father was aged 30–39, for couples where the dad was in his 50s, there was a:
- 16% increased risk of preterm birth
- 14% increased risk of low birth weight
- 13% increase in gestational diabetes.
The older fathers were also twice as likely to have used assisted reproductive technology, including IVF, to conceive than their younger counterparts.
Steven van Loy/Unsplash Dads are getting older
In this US study, the mean age of all fathers increased from 30.8 years in 2011 to 32.1 years in 2022.
In that same period, the proportion of men aged 50 years or older fathering a child increased from 1.1% to 1.3%.
We don’t know the proportion of men over 50 years who father children in Australia, but data shows the average age of fathers has increased.
In 1975 the median age of Australian dads was 28.6 years. This jumped to 33.7 years in 2022.
How male age affects getting pregnant
As we know from media reports of celebrity dads, men produce sperm from puberty throughout life and can father children well into old age.
However, there is a noticeable decline in sperm quality from about age 40.
Female partners of older men take longer to achieve pregnancy than those with younger partners.
A study of the effect of male age on time to pregnancy showed women with male partners aged 45 or older were almost five times more likely to take more than a year to conceive compared to those with partners aged 25 or under. More than three quarters (76.8%) of men under the age of 25 years impregnated their female partners within six months, compared with just over half (52.9%) of men over the age of 45.
Pooled data from ten studies showed that partners of older men are also more likely to experience miscarriage. Compared to couples where the male was aged 25 to 29 years, paternal age over 45 years increased the risk of miscarriage by 43%.
Older men are more likely to need IVF
Outcomes of assisted reproductive technology, such as IVF, are also influenced by the age of the male partner.
A review of studies in couples using assisted reproductive technologies found paternal age under 40 years reduced the risk of miscarriage by about 25% compared to couples with men aged over 40.
Having a male under 40 years also almost doubled the chance of a live birth per treatment cycle. With a man over 40, 17.6% of treatment rounds resulted in a live birth, compared to 28.4% when the male was under 40.
How does male age affect the health outcomes of children?
As a result of age-related changes in sperm DNA, the children of older fathers have increased risk of a number of conditions. Autism, schizophrenia, bipolar disorders and leukaemia have been linked to the father’s advanced years.
A review of studies assessing the impact of advanced paternal age reported that children of older fathers have increased rates of psychiatric disease and behavioural impairments.
But while the increased risk of adverse health outcomes linked to older paternal age is real, the magnitude of the effect is modest. It’s important to remember that an increase in a very small risk is still a small risk and most children of older fathers are born healthy and develop well.
Improving your health can improve your fertility
In addition to the effects of older age, some chronic conditions that affect fertility and reproductive outcomes become more common as men get older. They include obesity and diabetes which affect sperm quality by lowering testosterone levels.
While we can’t change our age, some lifestyle factors that increase the risk of pregnancy complications and reduce fertility, can be tackled. They include:
- smoking
- recreational drug taking
- anabolic steroid use
- heavy alcohol consumption.
Get the facts about the male biological clock
Research shows men want children as much as women do. And most men want at least two children.
Yet most men lack knowledge about the limitations of female and male fertility and overestimate the chance of getting pregnant, with and without assisted reproductive technologies.
We need better public education, starting at school, to improve awareness of the impact of male and female age on reproductive outcomes and help people have healthy babies.
For men wanting to improve their chance of conceiving, the government-funded sites Healthy Male and Your Fertility are a good place to start. These offer evidence-based and accessible information about reproductive health, and tips to improve your reproductive health and give your children the best start in life.
Karin Hammarberg, Senior Research Fellow, Global and Women’s Health, School of Public Health & Preventive Medicine, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Many Faces Of Cosmetic Surgery
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cosmetic Surgery: What’s The Truth?
In Tuesday’s newsletter, we asked you your opinion on elective cosmetic surgeries, and got the above-depicted, below-described, set of responses:
- About 48% said “Everyone should be able to get what they want, assuming informed consent”
- About 28% said “It can ease discomfort to bring features more in line with normalcy”
- 15% said “They should be available in the case of extreme disfigurement only”
- 10% said “No elective cosmetic surgery should ever be performed; needless danger”
Well, there was a clear gradient of responses there! Not so polarizing as we might have expected, but still enough dissent for discussion
So what does the science say?
The risks of cosmetic surgery outweigh the benefits: True or False?
False, subjectively (but this is important).
You may be wondering: how is science subjective?
And the answer is: the science is not subjective, but people’s cost:worth calculations are. What’s worth it to one person absolutely may not be worth it to another. Which means: for those for whom it wouldn’t be worth it, they are usually the people who will not choose the elective surgery.
Let’s look at some numbers (specifically, regret rates for various surgeries, elective/cosmetic or otherwise):
- Regret rate for elective cosmetic surgery in general: 20%
- Regret rate for knee replacement (i.e., not cosmetic): 17.1%
- Regret rate for hip replacement (i.e., not cosmetic): 4.8%
- Regret rate for gender-affirming surgeries (for transgender patients): 1%
So we can see, elective surgeries have an 80–99% satisfaction rate, depending on what they are. In comparison, the two joint replacements we mentioned have a 82.9–95.2% satisfaction rate. Not too dissimilar, taken in aggregate!
In other words: if a person has studied the risks and benefits of a surgery and decides to go ahead, they’re probably going to be happy with the results, and for them, the benefits will have outweighed the risks.
Sources for the above numbers, by the way:
- What is the regret rate for plastic surgery?
- Decision regret after primary hip and knee replacement surgery
- A systematic review of patient regret after surgery—a common phenomenon in many specialties but rare within gender-affirmation surgery
But it’s just a vanity; therapy is what’s needed instead: True or False?
False, generally. True, sometimes. Whatever the reasons for why someone feels the way they do about their appearance—whether their face got burned in a fire or they just have triple-J cups that they’d like reduced, it’s generally something they’ve already done a lot of thinking about. Nevertheless, it does also sometimes happen that it’s a case of someone hoping it’ll be the magical solution, when in reality something else is also needed.
How to know the difference? One factor is whether the surgery is “type change” or “restorative”, and both have their pros and cons.
- In “type change” (e.g. rhinoplasty), more psychological adjustment is needed, but when it’s all over, the person has a new nose and, statistically speaking, is usually happy with it.
- In “restorative” (e.g. facelift), less psychological adjustment is needed (as it’s just a return to a previous state), so a person will usually be happy quickly, but ultimately it is merely “kicking the can down the road” if the underlying problem is “fear of aging”, for example. In such a case, likely talking therapy would be beneficial—whether in place of, or alongside, cosmetic surgery.
Here’s an interesting paper on that; the sample sizes are small, but the discussion about the ideas at hand is a worthwhile read:
Does cosmetic surgery improve psychosocial wellbeing?
Some people will never be happy no matter how many surgeries they get: True or False?
True! We’re going to refer to the above paper again for this one. In particular, here’s what it said about one group for whom surgeries will not usually be helpful:
❝There is a particular subgroup of people who appear to respond poorly to cosmetic procedures. These are people with the psychiatric disorder known as “body dysmorphic disorder” (BDD). BDD is characterised by a preoccupation with an objectively absent or minimal deformity that causes clinically significant distress or impairment in social, occupational, or other areas of functioning.
For several reasons, it is important to recognise BDD in cosmetic surgery settings:
Firstly, it appears that cosmetic procedures are rarely beneficial for these people. Most patients with BDD who have had a cosmetic procedure report that it was unsatisfactory and did not diminish concerns about their appearance.
Secondly, BDD is a treatable disorder. Serotonin-reuptake inhibitors and cognitive behaviour therapy have been shown to be effective in about two-thirds of patients with BDD❞
~ Dr. David Castle et al. (lightly edited for brevity)
Which is a big difference compared to, for example, someone having triple-J breasts that need reducing, or the wrong genitals for their gender, or a face whose features are distinct outliers.
Whether that’s a reason people with BDD shouldn’t be able to get it is an ethical question rather than a scientific one, so we’ll not try to address that with science.
After all, many people (in general) will try to fix their woes with a haircut, a tattoo, or even a new sportscar, and those might sometimes be bad decisions, but they are still the person’s decision to make.
And even so, there can be protectionist laws/regulations that may provide a speed-bump, for example:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Your Exercise Today Gives A Brain Boost Tomorrow
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Regular 10almonds readers may remember we not long back wrote about a study that showed how daily activity levels, in aggregate, make a difference to brain health over the course of 1–2 weeks (in fact, it was a 9-day study):
Daily Activity Levels & The Measurable Difference They Make To Brain Health
Today, we’re going to talk about a new (published today, at time of writing) study that shows the associations between daily exercise levels (amongst other things) and how well people performed in cognitive tests the next day.
By this we mean: they recorded exercise vs sedentary behavior vs sleep on a daily basis (using wearable tech to track it), and tested them daily with cognitive tests, and looked at how the previous day’s activities (or lack thereof) impacted the next day’s test results.
Notably, the sample was of older adults (aged 50–83). The sample size wasn’t huge but was statistically significant (n=76) and the researchers are of course calling for more studies to be done with more people.
What they found
To put their findings into few words:
- Consistent light exercise boosts general cognitive performance not just for hours (which was already known) but through the next day.
- More moderate or vigorous activity than usual in particular led to better working memory and episodic memory the next day.
- More sleep (especially slow-wave deep sleep) improved episodic memory and psychomotor speed.
- Sedentary behavior was associated with poorer working memory.
Let’s define some terms:
- general cognitive performance = average of scores across the different tests
- working memory = very short term memory, such as remembering what you came into this room for, or (as an example of a test format) being able to take down a multi-digit number in one go without it being broken down (and then, testing with longer lengths of number until failure)
- episodic memory = memory of events in a narrative context, where and when they happened, etc
- psychomotor speed = the speed of connection between perception and reaction in quick-response tests
These are, of course, all useful things to have, which means the general advice here is to:
- move more, generally
- exercise more, specifically
- sit less, whenever reasonably possible
- sleep well
You can read the study itself here:
Want to know the best kind of exercise for brain health?
Check out our article about neuroscientist Dr. Suzuki, and what she has to say about it:
The Exercise That Protects Your Brain
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: