Complex PTSD – by Pete Walker
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about Complex PTSD, but there’s a lot more to be said than we can fit into an article or two.
Pete Walker, a licensed marriage and family therapist, does an excellent job and pulls no punches, starting from the book’s dedication and carrying the hard-hitting seriousness all the way through to the Appendices.
To this end, it absolutely may not be an easy book to read at times (emotionally speaking), especially if you have C-PTSD. On the other hand, you may also find it a very validating 300-odd pages of “Yes, he is telling my life story in words, now this makes sense!”
That said, it’s mostly not an anecdotes-based book and nor is it just a feelsy ride; it’s also a textbook and a how-to manual. It’s a textbook of how and why things come about the way they do, and a manual of how to effectively manage C-PTSD, and find peace. There’s no silver bullet here, but there is a very comprehensive guide, and chapters full of tools to use (and no, not the same CBT things you’ve probably read a hundred times, this is C-PTSD-specific stuff).
Bottom line: this is the C-PTSD book; if you buy only one book on the topic, make it this one.
Click here to check out Complex PTSD: From Surviving To Thriving, and indeed thrive!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
When supplies resume, should governments subsidise drugs like Ozempic for weight loss? We asked 5 experts
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Hundreds of thousands of people worldwide are taking drugs like Ozempic to lose weight. But what do we actually know about them? This month, The Conversation’s experts explore their rise, impact and potential consequences.
You’ve no doubt heard of Ozempic but have you heard of Wegovy? They’re both brand names of the drug semaglutide, which is currently in short supply worldwide.
Ozempic is a lower dose of semaglutide, and is approved and used to treat diabetes in Australia. Wegovovy is approved to treat obesity but is not yet available in Australia. Shortages of both drugs are expected to last throughout 2024.
Both drugs are expensive. But Ozempic is listed on Australia’s Pharmaceutical Benefits Schedule (PBS), so people with diabetes can get a three-week supply for A$31.60 ($7.70 for concession card holders) rather than the full price ($133.80).
Wegovy isn’t listed on the PBS to treat obesity, meaning when it becomes available, users will need to pay the full price. But should the government subsidise it?
Wegovy’s manufacturer will need to make the case for it to be added to the PBS to an independent advisory committee. The company will need to show Wegovy is a safe, clinically effective and cost-effective treatment for obesity compared to existing alternatives.
In the meantime, we asked five experts: when supplies resume, should governments subsidise drugs like Ozempic for weight loss?
Four out of five said yes
This is the last article in The Conversation’s Ozempic series. Read the other articles here.
Disclosure statements: Clare Collins is a National Health and Medical Research Council (NHMRC) Leadership Fellow and has received research grants from the National Health and Medical Research Council (NHMRC), the Australian Research Council (ARC), the Medical Research Future Fund (MRFF), the Hunter Medical Research Institute, Diabetes Australia, Heart Foundation, Bill and Melinda Gates Foundation, nib foundation, Rijk Zwaan Australia, the Western Australian Department of Health, Meat and Livestock Australia, and Greater Charitable Foundation. She has consulted to SHINE Australia, Novo Nordisk (for weight management resources and an obesity advisory group), Quality Bakers, the Sax Institute, Dietitians Australia and the ABC. She was a team member conducting systematic reviews to inform the 2013 Australian Dietary Guidelines update, the Heart Foundation evidence reviews on meat and dietary patterns and current co-chair of the Guidelines Development Advisory Committee for Clinical Practice Guidelines for Treatment of Obesity; Emma Beckett has received funding for research or consulting from Mars Foods, Nutrition Research Australia, NHMRC, ARC, AMP Foundation, Kellogg and the University of Newcastle. She works for FOODiQ Global and is a fat woman. She is/has been a member of committees/working groups related to nutrition or food, including for the Australian Academy of Science, the NHMRC and the Nutrition Society of Australia; Jonathan Karnon does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment; Nial Wheate in the past has received funding from the ACT Cancer Council, Tenovus Scotland, Medical Research Scotland, Scottish Crucible, and the Scottish Universities Life Sciences Alliance. He is a fellow of the Royal Australian Chemical Institute, a member of the Australasian Pharmaceutical Science Association and a member of the Australian Institute of Company Directors. Nial is the chief scientific officer of Vaihea Skincare LLC, a director of SetDose Pty Ltd (a medical device company) and a Standards Australia panel member for sunscreen agents. Nial regularly consults to industry on issues to do with medicine risk assessments, manufacturing, design and testing; Priya Sumithran has received grant funding from external organisations, including the NHMRC and MRFF. She is in the leadership group of the Obesity Collective and co-authored manuscripts with a medical writer provided by Novo Nordisk and Eli Lilly.
Fron Jackson-Webb, Deputy Editor and Senior Health Editor, The Conversation
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
The Five Pillars Of Longevity
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Five Pillars Of Longevity
This is Dr. Mark Hyman. He’s a medical doctor, and he’s the board president of clinical affairs of the Institute for Functional Medicine. He’s also the founder and medical director of the UltraWellness Center!
What he’d like you to know about is what he calls the “Five Pillars of Longevity”.
Now, here at 10almonds, we often talk about certain things that science finds to be good for almost any health condition, and have made a habit of referencing what we call “The Usual Five Things™” (not really a trademark, by the way—just a figure of speech), which are:
- Have a good diet
- Get good exercise
- Get good sleep
- Reduce (or eliminate) alcohol consumption
- Don’t smoke
…and when we’re talking about a specific health consideration, we usually provide sources as to why each of them are particularly relevant, and pointers as to the what/how associated with them (ie what diet is good, how to get good sleep, etc).
Dr. Hyman’s “Five Pillars of Longevity” are based on observations from the world’s “Blue Zones”, the popular name for areas with an unusually high concentration of supercentenarians—Sardinia and Okinawa being famous examples, with a particular village in each being especially exemplary.
These Five Pillars of Longevity partially overlap with ours for three out of five, and they are:
- Good nutrition
- Optimized workouts
- Reduce stress
- Get quality sleep
- Find (and live) your purpose
We won’t argue against those! But what does he have to say, for each of them?
Good nutrition
Dr. Hyman advocates for a diet he calls “pegan”, which he considers to combine the paleo and vegan diets. Here at 10almonds, we generally advocate for the Mediterranean Diet because of the mountains of evidence for it, but his approach may be similar in some ways, since it looks to consume a majority plant diet, with some unprocessed meats/fish, limited dairy, and no grains.
By the science, honestly, we stand by the Mediterranean (which includes whole grains), but if for example your body may have issues of some kind with grains, his approach may be a worthy consideration.
Optimized workouts
For Dr. Hyman, this means getting in three kinds of exercise regularly:
- Aerobic/cardio, to look after your heart health
- Resistance training (e.g. weights or bodyweight strength-training) to look after your skeletal and muscular health
- Yoga or similar suppleness training, to look after your joint health
Can’t argue with that, and it can be all too easy to fall into the trap of thinking “I’m healthy because I do x” while forgetting y and/or z! Thus, a three-pronged approach definitely has its merits.
Reduce stress
Acute stress (say, a cold shower) is can confer some health benefits, but chronic stress is ruinous to our health and it ages us. So, reducing this is critical. Dr. Hyman advocates for the practice of mindfulness and meditation, as well as journaling.
Get quality sleep
Quality here, not just quantity. As well as the usual “sleep hygiene” advices, he has some more unorthodox methods, such as the use of binaural beats to increase theta-wave activity in the brain (and thus induce more restful sleep), and the practice of turning off Wi-Fi, on the grounds that Wi-Fi signals interfere with our sleep.
We were curious about these recommendations, so we checked out what the science had to say! Here’s what we found:
- Minimal Effects of Binaural Auditory Beats for Subclinical Insomnia: A Randomized Double-Blind Controlled Study
- Spending the night next to a router – Results from the first human experimental study investigating the impact of Wi-Fi exposure on sleep
In short: probably not too much to worry about in those regards. On the other hand, worrying less, unlike those two things, is a well-established way improve sleep!
(Surprised we disagreed with our featured expert on a piece of advice? Please know: you can always rely on us to stand by what the science says; we pride ourselves on being as reliable as possible!)
Find (and live!) your purpose
This one’s an ikigai thing, to borrow a word from Japanese, or finding one’s raison d’être, as we say in English using French, because English is like that. It’s about having purpose.
Dr. Hyman’s advice here is consistent with what many write on the subject, and it’d be an interesting to have more science on, but meanwhile, it definitely seems consistent with commonalities in the Blue Zone longevity hotspots, where people foster community, have a sense of belonging, know what they are doing for others and keep doing it because they want to, and trying to make the world—or even just their little part of it—better for those who will follow.
Being bitter, resentful, and self-absorbed is not, it seems a path to longevity. But a life of purpose, or even just random acts of kindness, may well be.
Share This Post
-
As Nuns Disappear, Many Catholic Hospitals Look More Like Megacorporations
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ST. LOUIS — Inside the more than 600 Catholic hospitals across the country, not a single nun can be found occupying a chief executive suite, according to the Catholic Health Association.
Nuns founded and led those hospitals in a mission to treat sick and poor people, but some were also shrewd business leaders. Sister Irene Kraus, a former chief executive of Daughters of Charity National Health System, was famous for coining the phrase “no margin, no mission.” It means hospitals must succeed — generating enough revenue to exceed expenses — to fulfill their original mission.
The Catholic Church still governs the care that can be delivered to millions in those hospitals each year, using religious directives to ban abortions and limit contraceptives, in vitro fertilization, and medical aid in dying.
But over time, that focus on margins led the hospitals to transform into behemoths that operate for-profit subsidiaries and pay their executives millions, according to hospital tax filings. These institutions, some of which are for-profit companies, now look more like other megacorporations than like the charities for the destitute of yesteryear.
The absence of nuns in the top roles raises the question, said M. Therese Lysaught, a Catholic moral theologist and professor at Loyola University Chicago: “What does it mean to be a Catholic hospital when the enterprise has been so deeply commodified?”
The St. Louis area serves as the de facto capital of Catholic hospital systems. Three of the largest are headquartered here, along with the Catholic hospital lobbying arm. Catholicism is deeply rooted in the region’s culture. During Pope John Paul II’s only U.S. stop in 1999, he led Mass downtown in a packed stadium of more than 100,000 people.
For a quarter century, Sister Mary Jean Ryan led SSM Health, one of those giant systems centered on St. Louis. Now retired, the 86-year-old said she was one of the last nuns in the nation to lead a Catholic hospital system.
Ryan grew up Catholic in Wisconsin and joined a convent while in nursing school in the 1960s, surprising her family. She admired the nuns she worked alongside and felt they were living out a higher purpose.
“They were very impressive,” she said. “Not that I necessarily liked all of them.”
Indeed, the nuns running hospitals defied the simplistic image often ascribed to them, wrote John Fialka in his book “Sisters: Catholic Nuns and the Making of America.”
“Their contributions to American culture are not small,” he wrote. “Ambitious women who had the skills and the stamina to build and run large institutions found the convent to be the first and, for a long time, the only outlet for their talents.”
This was certainly true for Ryan, who climbed the ranks, working her way from nurse to chief executive of SSM Health, which today has hospitals in Illinois, Missouri, Oklahoma, and Wisconsin.
The system was founded more than a century ago when five German nuns arrived in St. Louis with $5. Smallpox swept through the city and the Sisters of St. Mary walked the streets offering free care to the sick.
Their early foray grew into one of the largest Catholic health systems in the country, with annual revenue exceeding $10 billion, according to its 2023 audited financial report. SSM Health treats patients in 23 hospitals and co-owns a for-profit pharmacy benefit manager, Navitus, that coordinates prescriptions for 14 million people.
But Ryan, like many nuns in leadership roles in recent decades, found herself confronted with an existential crisis. As fewer women became nuns, she had to ensure the system’s future without them.
When Ron Levy, who is Jewish, started at SSM as an administrator, he declined to lead a prayer in a meeting, Ryan recounted in her book, “On Becoming Exceptional.”
“Ron, I’m not asking you to be Catholic,” she recalled telling him. “And I know you’ve only been here two weeks. So, if you’d like to make it three, I suggest you be prepared to pray the next time you’re asked.”
Levy went on to serve SSM for more than 30 years — praying from then on, Ryan wrote.
In Catholic hospitals, meetings are still likely to start with a prayer. Crucifixes often adorn buildings and patient rooms. Mission statements on the walls of SSM facilities remind patients: “We reveal the healing presence of God.”
Above all else, the Catholic faith calls on its hospitals to treat everyone regardless of race, religion, or ability to pay, said Diarmuid Rooney, a vice president of the Catholic Health Association. No nuns run the trade group’s member hospitals, according to the lobbying group. But the mission that compelled the nuns is “what compels us now,” Rooney said. “It’s not just words on a wall.”
The Catholic Health Association urges its hospitals to evaluate themselves every three years on whether they’re living up to Catholic teachings. It created a tool that weighs seven criteria, including how a hospital acts as an extension of the church and cares for poor and marginalized patients.
“We’re not relying on hearsay that the Catholic identity is alive and well in our facilities and hospitals,” Rooney said. “We can actually see on a scale where they are at.”
The association does not share the results with the public.
At SSM Health, “our Catholic identity is deeply and structurally ingrained” even with no nun at the helm, spokesperson Patrick Kampert said. The system reports to two boards. One functions as a typical business board of directors while the other ensures the system abides by the rules of the Catholic Church. The church requires the majority of that nine-member board to be Catholic. Three nuns currently serve on it; one is the chair.
Separately, SSM also is required to file an annual report with the Vatican detailing the ways, Kampert said, “we deepen our Catholic identity and further the healing ministry of Jesus.” SSM declined to provide copies of those reports.
From a business perspective, though, it’s hard to distinguish a Catholic hospital system like SSM from a secular one, said Ruth Hollenbeck, a former Anthem insurance executive who retired in 2018 after negotiating Missouri hospital contracts. In the contracts, she said, the difference amounted to a single paragraph stating that Catholic hospitals wouldn’t do anything contrary to the church’s directives.
To retain tax-exempt status under Internal Revenue Service rules, all nonprofit hospitals must provide a “benefit” to their communities such as free or reduced-price care for patients with low incomes. But the IRS provides a broad definition of what constitutes a community benefit, which gives hospitals wide latitude to justify not needing to pay taxes.
On average, the nation’s nonprofit hospitals reported that 15.5% of their total annual expenses were for community benefits in 2020, the latest figure available from the American Hospital Association.
SSM Health, including all of its subsidiaries, spent proportionately far less than the association’s average for individual hospitals, allocating roughly the same share of its annual expenses to community efforts over three years: 5.1% in 2020, 4.5% in 2021, and 4.9% in 2022, according to a KFF Health News analysis of its most recent publicly available IRS filings and audited financial statements.
A separate analysis from the Lown Institute think tank placed five Catholic systems — including the St. Louis region’s Ascension — on its list of the 10 health systems with the largest “fair share” deficits, which means receiving more in tax breaks than what they spent on the community. And Lown said three St. Louis-area Catholic health systems — Ascension, SSM Health, and Mercy — had fair share deficits of $614 million, $235 million, and $92 million, respectively, in the 2021 fiscal year.
Ascension, Mercy, and SSM disputed Lown’s methodology, arguing it doesn’t take into account the gap between the payments they receive for Medicaid patients and the cost of delivering their care. The IRS filings do.
But, Kampert said, many of the benefits SSM provides aren’t reflected in its IRS filings either. The forms reflect “very simplistic calculations” and do not accurately represent the health system’s true impact on the community, he said.
Today, SSM Health is led by longtime business executive Laura Kaiser. Her compensation in 2022 totaled $8.4 million, including deferred payments, according to its IRS filing. Kampert defended the amount as necessary “to retain and attract the most qualified” candidate.
By contrast, SSM never paid Ryan a salary, giving instead an annual contribution to her convent of less than $2 million a year, according to some tax filings from her long tenure. “I didn’t join the convent to earn money,” Ryan said.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
Who will look after us in our final years? A pay rise alone won’t solve aged-care workforce shortages
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Aged-care workers will receive a significant pay increase after the Fair Work Commission ruled they deserved substantial wage rises of up to 28%. The federal government has committed to the increases, but is yet to announce when they will start.
But while wage rises for aged-care workers are welcome, this measure alone will not fix all workforce problems in the sector. The number of people over 80 is expected to triple over the next 40 years, driving an increase in the number of aged care workers needed.
How did we get here?
The Royal Commission into Aged Care Quality and Safety, which delivered its final report in March 2021, identified a litany of tragic failures in the regulation and delivery of aged care.
The former Liberal government was dragged reluctantly to accept that a total revamp of the aged-care system was needed. But its weak response left the heavy lifting to the incoming Labor government.
The current government’s response started well, with a significant injection of funding and a promising regulatory response. But it too has failed to pursue a visionary response to the problems identified by the Royal Commission.
Action was needed on four fronts:
- ensuring enough staff to provide care
- building a functioning regulatory system to encourage good care and weed out bad providers
- designing and introducing a fair payment system to distribute funds to providers and
- implementing a financing system to pay for it all and achieve intergenerational equity.
A government taskforce which proposed a timid response to the fourth challenge – an equitable financing system – was released at the start of last week.
Consultation closed on a very poorly designed new regulatory regime the week before.
But the big news came at end of the week when the Fair Work Commission handed down a further determination on what aged-care workers should be paid, confirming and going beyond a previous interim determination.
What did the Fair Work Commission find?
Essentially, the commission determined that work in industries with a high proportion of women workers has been traditionally undervalued in wage-setting. This had consequences for both care workers in the aged-care industry (nurses and Certificate III-qualified personal-care workers) and indirect care workers (cleaners, food services assistants).
Aged-care staff will now get significant pay increases – 18–28% increase for personal care workers employed under the Aged Care Award, inclusive of the increase awarded in the interim decision.
The commission determined aged care work was undervalued.
Shutterstock/Toa55Indirect care workers were awarded a general increase of 3%. Laundry hands, cleaners and food services assistants will receive a further 3.96% on the grounds they “interact with residents significantly more regularly than other indirect care employees”.
The final increases for registered and enrolled nurses will be determined in the next few months.
How has the sector responded?
There has been no push-back from employer groups or conservative politicians. This suggests the uplift is accepted as fair by all concerned.
The interim increases of up to 15% probably facilitated this acceptance, with the recognition of the community that care workers should be paid more than fast food workers.
There was no criticism from aged-care providers either. This is probably because they are facing difficulty in recruiting staff at current wage rates. And because government payments to providers reflect the actual cost of aged care, increased payments will automatically flow to providers.
When the increases will flow has yet to be determined. The government is due to give its recommendations for staging implementation by mid-April.
Is the workforce problem fixed?
An increase in wages is necessary, but alone is not sufficient to solve workforce shortages.
The health- and social-care workforce is predicted to grow faster than any other sector over the next decade. The “care economy” will grow from around 8% to around 15% of GDP over the next 40 years.
This means a greater proportion of school-leavers will need to be attracted to the aged-care sector. Aged care will also need to attract and retrain workers displaced from industries in decline and attract suitably skilled migrants and refugees with appropriate language skills.
Aged care will need to attract workers from other sectors.
nastya_ph/ShutterstockThe caps on university and college enrolments imposed by the previous government, coupled with weak student demand for places in key professions (such as nursing), has meant workforce shortages will continue for a few more years, despite the allure of increased wages.
A significant increase in intakes into university and vocational education college courses preparing students for health and social care is still required. Better pay will help to increase student demand, but funding to expand place numbers will ensure there are enough qualified staff for the aged-care system of the future.
Stephen Duckett, Honorary Enterprise Professor, School of Population and Global Health, and Department of General Practice and Primary Care, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
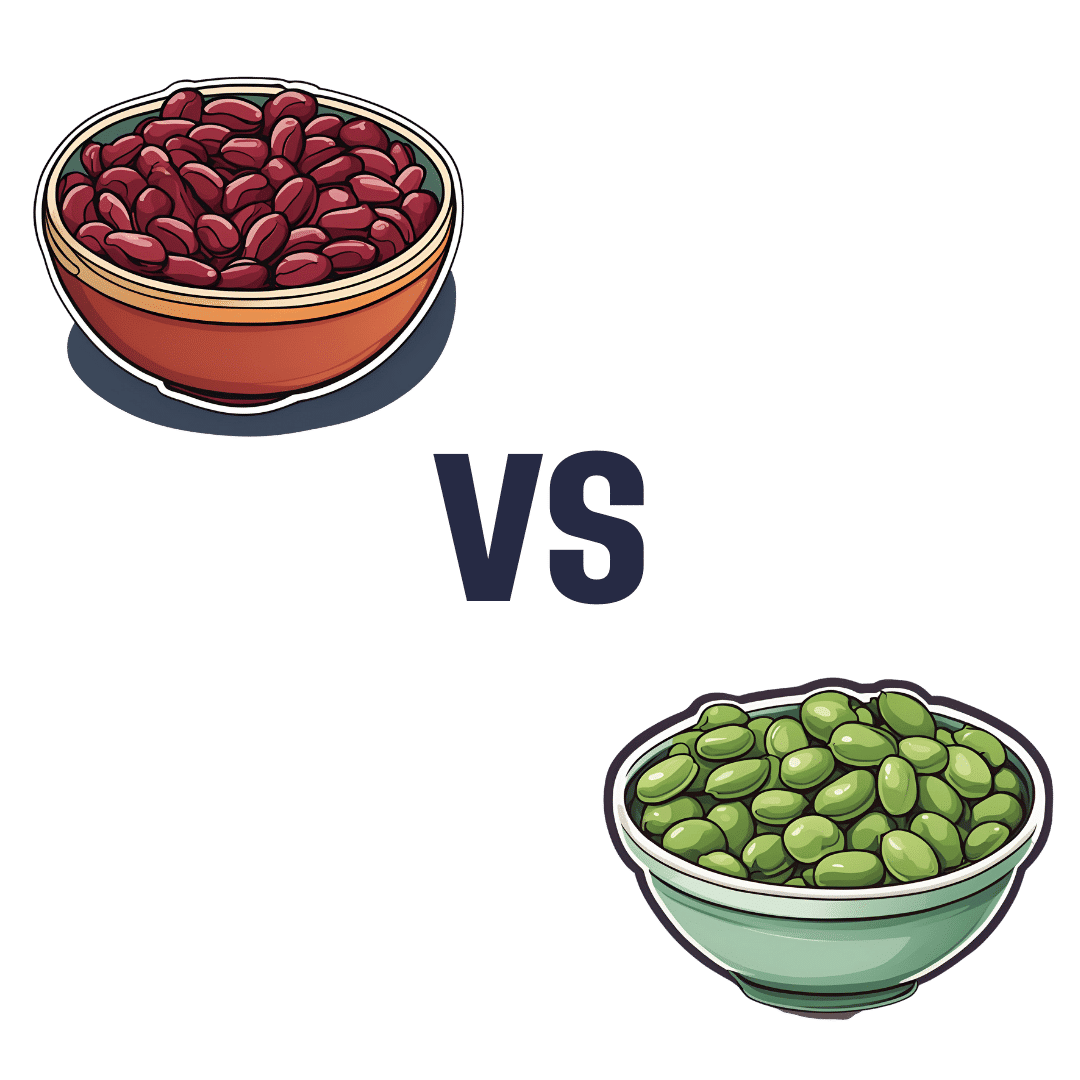
Kidney Beans vs Fava Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing kidney beans to fava beans, we picked the kidney beans.
Why?
It’s a simple and straightforward one today!
The macronutrient profiles are mostly comparable, but kidney beans do have a little more protein and a little more fiber.
In the category of vitamins, kidney beans have more of vitamins B1, B5, B6, B9, C, E, & K, while fava beans boast only more of vitamins B2 and B3. They are both equally good sources of choline, but the general weight of vitamins is very much in kidney beans’ favor, with a 7:2 lead, most of which have generous margins.
When it comes to minerals, kidney beans have more iron, phosphorus, and potassium, while fava beans have more copper and selenium. They’re both equally good sources of other minerals they both contain. Still, a 3:2 victory for kidney beans on the mineral front.
Adding up the moderate victory on macros, the strong victory on vitamins, and the slight victory on minerals, all in all makes for a clear win for kidney beans.
Still, enjoy both! Diversity is healthy.
Want to learn more?
You might like to read:
Chickpeas vs Black Beans – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cold Medicines & Heart Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cold Medicines & Heart Health
In the wake of many decongestants disappearing from a lot of shelves after a common active ingredient being declared useless*, you may find yourself considering alternative decongestants at this time of year.
*In case you missed it:
It doesn’t seem to be dangerous, by the way, just also not effective:
FDA Panel Says Common OTC Decongestant, Phenylephrine, Is Useless
Good for your nose, bad for your heart?
With products based on phenylephrine out of the running, products based on pseudoephedrine, a competing drug, are enjoying a surge in popularity.
Good news: pseudoephedrine works!
Bad news: pseudoephedrine works because it is a vasoconstrictor, and that vasoconstriction reduces nasal swelling. That same vasoconstriction also raises overall blood pressure, potentially dangerously, depending on an assortment of other conditions you might have.
Further reading: Can decongestants spike your blood pressure? What to know about hypertension and cold medicine
Who’s at risk?
The warning label, unread by many, reads:
❝Do not use this product if you have heart disease, high blood pressure, thyroid disease, diabetes, or difficulty in urination due to enlargement of the prostate gland, unless directed by a doctor❞
Source: Harvard Health | Don’t let decongestants squeeze your heart
What are the other options?
The same source as above recommends antihistamines as an option to be considered, citing:
❝Antihistamines such as […] cetirizine (Zyrtec) and loratadine (Claritin) can help with a stuffy nose and are safe for the heart.❞
But we’d be remiss not to mention drug-free options too, for example:
- Saline rinse with a neti pot or similar
- Use of a humidifier in your house/room
- Steam inhalation, with or without eucalyptus etc
See also: Inhaled Eucalyptus’s Immunomodulatory and Antimicrobial Effects
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: