With Only Gloves To Protect Them, Farmworkers Say They Tend Sick Cows Amid Bird Flu
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
GREELEY, Colo. — In early August, farmworkers gathered under a pavilion at a park here for a picnic to celebrate Farmworker Appreciation Day. One sign that this year was different from the others was the menu: Beef fajitas, tortillas, pico de gallo, chips, beans — but no chicken.
Farms in Colorado had culled millions of chickens in recent months to stem the transmission of bird flu. Organizers filled out the spread with hot dogs.
No matter the menu, some dairy workers at the event said they don’t exactly feel appreciated. They said they haven’t received any personal protective equipment beyond gloves to guard against the virus, even as they or colleagues have come down with conjunctivitis and flu-like symptoms that they fear to be bird flu.
“They should give us something more,” one dairy worker from Larimer County said in Spanish. He spoke on the condition of anonymity out of fear he’d lose his job for speaking out. “What if something happens to us? They act as if nothing is wrong.”
Agricultural health and safety experts have been trying to get the word out about how to protect against bird flu, including through bilingual videos on TikTok showing the proper way to gear up with respirators, eye protection, gloves, and coveralls. And Colorado’s health and agriculture departments have offered a free month’s supply of protective equipment to any producer who requests it.
But so far, many farms aren’t taking them up on it: According to numbers provided by the state health department in late August, fewer than 13% of the state’s dairies had requested and received such PPE.
The virus is known to infect mammals — from skunks, bears, and cows to people and house pets. It began showing up in dairy cattle in recent months, and Colorado has been in the thick of it. Ten of the 13 confirmed human cases in the U.S. this year have occurred in Colorado, where it continues to circulate among dairy cows. It isn’t a risk in cooked meat or pasteurized milk but is risky for those who come into contact with infected animals or raw milk.
Weld County, where the farmworker event was held, is one of the nation’s top milk producers, supplying enough milk each month this year to fill about 45 Olympic-size swimming pools, according to U.S. Department of Agriculture data. Neighboring counties are notable producers, too.
Concerns are growing about undiagnosed illness among farmworkers because of a lack of testing and safety precautions. One reason for concern: Bird flu and seasonal flu are capable of gene trading, so if they ended up in the same body at the same time, bird flu might end up with genes that boost its contagiousness. The virus doesn’t appear to be spreading easily between people yet. That could change, and if people aren’t being tested then health officials may be slow to notice.
Strains of seasonal flu already kill some 47,000 people in the U.S. a year. Public health officials fear the havoc a new form of the flu could wreak if it spreads among people.
The Centers for Disease Control and Prevention recommends that dairy workers don a respirator and goggles or a face shield, among other protections, whether they are working with sick animals or not.
A recent study found that not all infected cows show symptoms, so workers could be interacting with contagious animals without realizing it. Even when it is known that animals are infected, farmworkers often still have to get in close contact with them, sometimes under grueling conditions, such as during a recent heat wave when Colorado poultry workers collected hundreds of chickens by hand for culling because of the outbreak. At least six of the workers became infected with bird flu.
One dairy worker in Weld County, who spoke on the condition of anonymity for fear of losing his job, said his employer has not offered any protective equipment beyond gloves, even though he works with sick cows and raw milk.
His bosses asked the workers to separate sick cows from the others after some cows produced less milk, lost weight, and showed signs of weakness, he said. But the employer didn’t say anything about the bird flu, he said, or suggest they take any precautions for their own safety.
He said he bought protective goggles for himself at Walmart when his eyes became itchy and red earlier this summer. He recalled experiencing dizziness, headaches, and low appetite around the same time. But he self-medicated and pushed through, without missing work or going to a doctor.
“We need to protect ourselves because you never know,” he said in Spanish. “I tell my wife and son that the cows are sick, and she tells me to leave, but it will be the same wherever I go.”
He said he’d heard that his employers were unsympathetic when a colleague approached them about feeling ill. He’d even seen someone affiliated with management remove a flyer about how people can protect themselves from the bird flu and throw it in a bin.
The dairy worker in neighboring Larimer County said he, too, has had just gloves as protection, even when he has worked with sick animals — close enough for saliva to wipe off on him. He started working with them when a colleague missed work because of his flu-like symptoms: fever, headache, and red eyes.
“I only wear latex gloves,” he said. “And I see that those who work with the cows that are sick also only wear gloves.”
He said he doesn’t have time to wash his hands at work but puts on hand sanitizer before going home and takes a shower once he arrives. He has not had symptoms of infection.
Such accounts from dairy workers echo those from farmworkers in Texas, as reported by KFF Health News in July.
“Employers who are being proactive and providing PPE seem to be in the minority in most states,” said Bethany Boggess Alcauter with the National Center for Farmworker Health, a not-for-profit organization based in Texas that advocates for improving the health of farmworkers and their families. “Farmworkers are getting very little information.”
But Zach Riley, CEO of the Colorado Livestock Association, said he thinks such scenarios are the exception, not the rule.
“You would be hard-pressed to find a dairy operation that isn’t providing that PPE,” he said. Riley said dairies typically have a stockpile of PPE ready to go for situations like this and that, if they don’t, it’s easily accessed through the state. “All you have to do is ask.”
Producers are highly motivated to keep infections down, he said, because “milk is their life source.” He said he has heard from some producers that “their family members who work on the farm are doing 18-to 20-hour days just to try to stay ahead of it, so that they’re the first line between everything, to protect their employees.”
Colorado’s health department is advertising a hotline that ill dairy workers can call for help getting a flu test and medicine.
Project Protect Food Systems Workers, an organization that emerged early in the covid-19 pandemic to promote farmworker health across Colorado, is distributing PPE it received from the state so promotoras — health workers who are part of the community they serve — can distribute masks and other protections directly to workers if employers aren’t giving them out.
Promotora Tomasa Rodriguez said workers “see it as another virus, another covid, but it is because they don’t have enough information.”
She has been passing out flyers about symptoms and protective measures, but she can’t access many dairies. “And in some instances,” she said, “a lot of these workers don’t know how to read, so the flyers are not reaching them, and then the employers are not doing any kind of talks or trainings.”
The CDC’s Nirav Shah said during an Aug. 13 call with journalists that awareness about bird flu among dairy workers isn’t as high as officials would like it to be, despite months of campaigns on social media and the radio.
“There’s a road ahead of us that we still need to go down to get awareness on par with, say, what it might be in the poultry world,” he said. “We’re using every single messenger that we can.”
KFF Health News correspondents Vanessa G. Sánchez and Amy Maxmen contributed to this report.
Healthbeat is a nonprofit newsroom covering public health published by Civic News Company and KFF Health News. Sign up for its newsletters here.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Is TikTok right? Can adding a teaspoon of cinnamon to your coffee help you burn fat?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cinnamon has been long used around the world in both sweet and savoury dishes and drinks.
But a new TikTok trend claims adding a teaspoon of cinnamon to your daily coffee (and some cocoa to make it more palatable) for one week can help you burn fat. Is there any truth to this?
Evannovostro/Shutterstock Not all cinnamon is the same
There are two types of cinnamon, both of which come from grinding the bark of the cinnamomum tree and may include several naturally occurring active ingredients.
Cassia cinnamon is the most common type available in grocery stores. It has a bitter taste and contains higher levels of one of the active ingredient cinnamaldehyde, a compound that gives cinnamon its flavour and odour. About 95% of cassia cinnamon is cinnamaldehyde.
The other is Ceylon cinnamon, which tastes sweeter. It contains about 50-60% cinnamaldehyde.
Does cinnamon burn fat? What does the research say?
A review of 35 studies examined whether consuming cinnamon could affect waist circumference, which is linked to increased body fat levels. It found cinnamon doses below 1.5 grams per day (around half a teaspoon) decreased waist circumference by 1.68cm. However, consuming more than 1.5g/day did not have a significant effect.
A meta-analysis of 21 clinical trials with 1,480 total participants found cinnamon also reduced body mass index (BMI) by 0.40kg/m² and body weight by 0.92kg. But it did not change the participants’ composition of fat or lean mass.
Another umbrella review, which included all the meta-analyses, found a small effect of cinnamon on weight loss. Participants lost an average of 0.67kg and reduced their BMI by 0.45kg/m².
The effect appears small. Radu Sebastian/Shutterstock So overall, the weight loss we see from these high-quality studies is very small, ranging anywhere from two to six months and mostly with no change in body composition.
The studies included people with different diseases, and most were from the Middle East and/or the Indian subcontinent. So we can’t be certain we would see this effect in people with other health profiles and in other countries. They were also conducted over different lengths of time from two to six months.
The supplements were different, depending on the study. Some had the active ingredient extracted from cinnamon, others used cinnamon powder. Doses varied from 0.36g to 10g per day.
They also used the two different types of cinnamon – but none of the studies used cinnamon from the grocery store.
How could cinnamon result in small amounts of weight loss?
There are several possible mechanisms.
It appears to allow blood glucose (sugar) to enter the body’s cells more quickly. This lowers blood glucose levels and can make insulin work more effectively.
It also seems to improve the way we break down fat when we need it for energy.
Finally, it may make us feel fuller for longer by slowing down how quickly the food is released from our stomach into the small intestine.
What are the risks?
Cinnamon is generally regarded as safe when used as a spice in cooking and food.
However, in recent months the United States and Australia have issued health alerts about the level of lead and other heavy metals in some cinnamon preparations.
Lead enters as a contaminant during growth (from the environment) and in harvesting. In some cases, it has been suggested there may have been intentional contamination.
Some people can have side effects from cinnamon, including gastrointestinal pain and allergic reactions.
One of the active ingredients, coumarin, can be toxic for some people’s livers. This has prompted the European Food Authority to set a limit of 0.1mg/kg of body weight.
Cassia cinnamon contains up to 1% of coumarin, and the Ceylon variety contains much less, 0.004%. So for people weighing above 60kg, 2 teaspoons (6g) of cassia cinnamon would bring them over the safe limit.
What about the coffee and cocoa?
Many people may think coffee can also help us lose weight. However there isn’t good evidence to support this yet.
An observational study found drinking one cup of regular coffee was linked to a reduction in weight that is gained over four years, but by a very small amount: an average of 0.12kg.
Good-quality cocoa and dark chocolate have also been shown to reduce weight. But again, the weight loss was small (between 0.2 and 0.4kg) and only after consuming it for four to eight weeks.
So what does this all mean?
Using cinnamon may have a very small effect on weight, but it’s unlikely to deliver meaningful weight loss without other lifestyle adjustments.
We also need to remember these trials used products that differ from the cinnamon we buy in the shops. How we store and how long we keep cinnamon might also impact or degrade the active ingredients.
And consuming more isn’t going to provide additional benefit. In fact, it could increase your risk of side effects.
So if you enjoy the taste of cinnamon in your coffee, continue to add it, but given its strong taste, you’re likely to only want to add a little.
And no matter how much we’d like this to be true, we certainly won’t gain any fat-loss benefits by consuming cinnamon on doughnuts or in buns, due to their high kilojoule count.
If you want to lose weight, there are evidence-backed approaches that won’t spoil your morning coffee.
Evangeline Mantzioris, Program Director of Nutrition and Food Sciences, Accredited Practising Dietitian, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
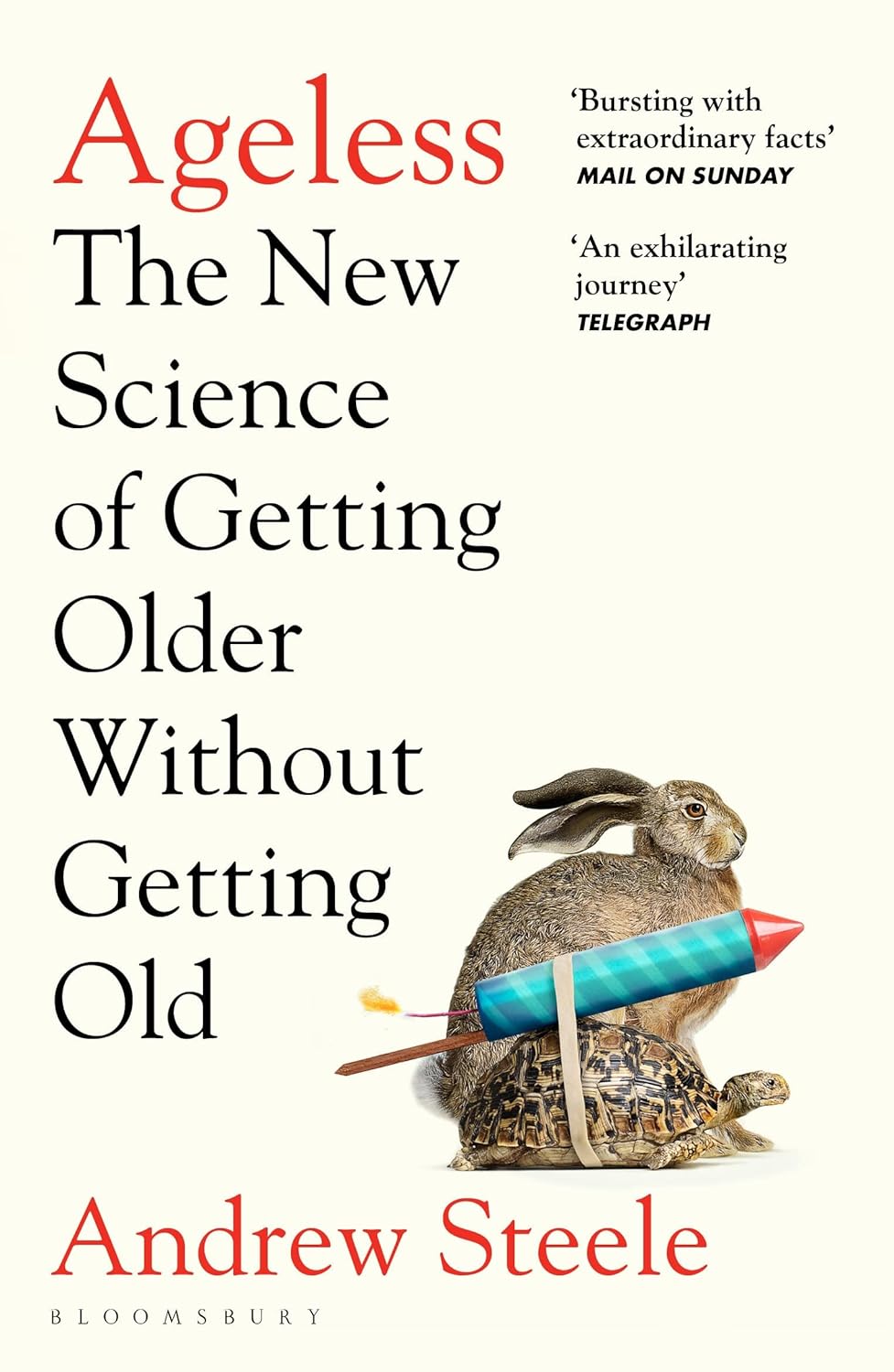
Ageless – by Dr. Andrew Steele
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
So, yet another book with “The new science of…” in the title; does this one deliver new science?
Actually, yes, this time! The author was originally a physicist before deciding that aging was the number one problem that needed solving, and switched tracks to computational biology, and pioneered a lot of research, some of the fruits of which can be found in this book, in amongst a more general history of the (very young!) field of biogerontology.
Downside: most of this is not very practical for the lay reader; most of it is explanations of how things happen on a cellular and/or genetic level, and how we learned that. A lot also pertains to what we can learn from animals that either age very slowly, or are biologically immortal (in other words, they can still be killed, but they don’t age and won’t die of anything age-related), or are immune to cancer—and how we might borrow those genes for gene therapy.
However, there are also chapters on such things as “running repairs”, “reprogramming aging”, and “how to live long enough to live even longer”.
The style is conversational pop science; in the prose, he simply states things without reference, but at the back, there are 40 pages of bibliography, indexed in the order in which they occurred and prefaced with the statement that he’s referencing in each case. It’s an odd way to do citations, but it works comfortably enough.
Bottom line: if you’d like to understand aging on the cellular level, and how we know what we know and what the likely future possibilities are, then this is a great book; it’s also simply very enjoyable to read, assuming you have an interest in the topic (as this reviewer does).
Click here to check out Ageless, and understand the science of getting older without getting old!
Share This Post
-
Anti-Inflammatory Khichri & Tadka
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is halfway between a daal and a risotto; it’s delicious and it’s full of protein, fiber, heathy fats, and flavors. And those flavors? Mostly from health-giving phytochemicals of one kind of another.
You will need
For the khichri:
- 1 oz chana dal
- 1 oz red lentils
- 1 oz brown lentils
- 1 oz quinoa
- 4 oz wholegrain basmati rice
- 1 tbsp chia seeds
- 1 tsp ground turmeric
- ½ tsp MSG or 1 tsp low-sodium salt
For the tadka:
- 2 tbsp avocado oil (or other oil suitable for high temperatures—so, not olive oil on this occasion!)
- ¼ bulb garlic, thinly sliced
- 1 fresh red chili (adjust per heat preferences)
- 1 fresh green chili (adjust per heat preferences)
- 1 tsp cumin seeds
- 6 curry leaves
- 12 twists of freshly ground black pepper
To serve:
- Optional: flatbreads or poppadoms
- Optional: lemon wedges or lime wedges
- Optional: chopped cilantro or parsley
Method
(we suggest you read everything at least once before doing anything)
1) Simmer the khichri ingredients in 5 cups of water, stirring occasionally if necessary, until it has a risotto-like consistency; this will probably take about 30–40 minutes. This time can be greatly reduced by using a pressure cooker, but obviously you won’t be able to check or stir, so do that only if you know what you’re doing cooking those grains and pseudograins in there, and what settings/timings to use for your specific device.
2) Make the tadka when the khichri is nearly ready, by heating the 2 tbsp of avocado oil in a skillet until very hot but not smoking, Add the rest of the ingredients from the tadka section, and cook until the garlic is nice and golden.
3) Pour the tadka over the khichri to serve, with any of the optional accompaniments we mentioned.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Capsaicin For Weight Loss And Against Inflammation
- The Many Health Benefits Of Garlic
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- Why Curcumin (Turmeric) Is Worth Its Weight In Gold
- If You’re Not Taking Chia, You’re Missing Out
Take care!
Share This Post
Related Posts
-
A Supplement To Rival St. John’s Wort Against Depression
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Do You Feel The SAMe?
S-Adeonsyl-L-Methionone (SAMe) is a chemical found naturally in the body, and/but enjoyed widely as a supplement. The main reasons people take it are:
- Improve mood (antidepressant effect)
- Improve joints (reduce osteoarthritis symptoms)
- Improve liver (detoxifying effect)
Let’s see what the science says for each of those claims…
Does it improve mood?
It seems to perform comparably to St. John’s Wort (which is good; it performs comparably to Prozac).
Best of all, it does this with fewer contraindications (St. John’s Wort has so many contraindications).
Here’s how they stack up:
This looks very promising, though it’d be nice to see a larger body of research, to be sure.
Does it reduce osteoarthritis symptoms?
The good news: it performs comparably to ibuprofen, with fewer side effects!
The bad news: it also performs comparably to placebo!
Read into that what you will about ibuprofen’s usefulness vs OA symptoms.
Read all about it:
S-Adenosylmethionine for osteoarthritis of the knee or hip
If you were hoping for something for OA or similar symptoms, you might like our previous main features:
- Avoiding/Managing Osteoarthritis
- Managing Chronic Pain (Realistically!)
- The 7 Approaches To Pain Management
- (Science-Based) Alternative Pain Relief
Does it help against liver disease?
According to adverts for SAMe: absolutely!
According to science: we don’t know
The science for this is so weak that it’d be unworthy of mention if it weren’t for the fact that SAMe is so widely sold as good against hepatotoxicity.
To be clear: maybe it really is great! Science hasn’t yet disproved its usefulness either.
It is popularly assumed to be beneficial due to there being an association between lower levels of SAMe in the body (remember, it is also produced inside our bodies) and development of liver disease, especially cholestasis.
Here’s an example of what pretty much every study we found was like (inconclusive research based mostly on mice):
S-adenosylmethionine in liver health, injury, and cancer
For other options for liver health, consider:
Is it safe?
Safety trials have been done ranging from 3 months to 2 years, with no serious side effects coming to light. So, it appears quite safe.
That said, as with anything, there are contraindications, such as:
- if you have bipolar disorder, skip this unless directed by your health care provider, because it may worsen the symptoms of mania
- if you are on SSRIs or other serotonergic drugs, it may interact with those
- if you are immunocompromised, you might want to skip it can increase the risk of P. carinii growth in such cases
As always, do speak with your doctor/pharmacist for personalized advice.
Summary
SAMe’s evidence-based qualities seem to stack up as follows:
- Against depression: good
- Against osteoarthritis: weak
- Against liver disease: unknown
As for safety, it has been found quite safe for most people.
Where can I get it?
We don’t sell it, but here is an example product on Amazon, for your convenience
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Hazelnuts vs Pistachios – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing hazelnuts to pistachios, we picked the hazelnuts.
Why?
An argument could be made for either, depending on what we prioritize! So there was really no wrong answer here today, but it is good to know what each nut’s strengths are:
In terms of macros, pistachios have more fiber, carbs, protein, and (mostly healthy) fat. That does make them the “more food per food” option, but it’s worth noting that while hazelnuts have more fiber, they also have a higher margin of difference when it comes to their greater carb count, and resultantly, hazelnuts do have the lower glycemic index. That said, they’re still both low-GI foods, so we’ll call this section a win for pistachios overall.
When it comes to vitamins, hazelnuts have more of vitamins B3, B5, B9, C, E, K, and choline, while pistachios have more of vitamins A, B1, B2, and B6. So, a fair 7:4 win for hazelnuts here.
In the category of minerals, hazelnuts have more calcium, copper, iron, magnesium, manganese, and zinc, while pistachios have more phosphorus, potassium, and selenium. A clear 6:3 win for hazelnuts.
In short, both are good sources of many nutrients, so choose according to what you want to prioritize, or better yet, enjoy both.
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Being Mortal – by Dr. Atul Gawande
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Maybe you want to “live forever or die trying”, and that’s an understandable goal… But are you prepared for “or die trying” being the outcome?
This is not a cheerful book, if you’re anything like this reviewer, you will need a little towel or something to mop up the tears while you read. But it’s worth it.
Dying is one thing; fighting for life is even generally considered a noble endeavor. Suffering alone isn’t fun, losing independence can feel humiliating, and seeing someone who was always a tower of strength, now a frail shadow of their former self, reduced to begging for something that they’re “not allowed”, can be worse.
Do we want that for ourselves? For our loved ones? Can there be a happy medium between that, and the alternative to indeed “go gentle into that good night”?
Dr. Gawande, a surgeon well-acquainted with death and dying, thinks so. But it involves work on our part, and being prepared for hard decisions.
- What is most important to us, and what tradeoffs are we willing to make for it?
- What, even, is actually an option to us with the resources available?
- Can we make peace with a potentially bad lot? And… Should we?
- When is fighting important, and when is it self-destructive?
These (and others) are all difficult questions posed by Dr. Gawande, but critical ones.
We don’t usually quote other people’s reviews when reviewing books here, but let’s consider the following words from the end of a long review on Amazon:
❝If “dying as we lived” is some kind of standard for how we should go, then maybe alone and medicalized makes some sense right now after all.❞
Bottom line: we all deserve better than that. And if we don’t take the time to think about what’s most important, then time will take it from us. This very insightful book may not have all the answers, but it has the questions, and it can help a lot in exploring them and deciding what matters most to us in the end, really.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: