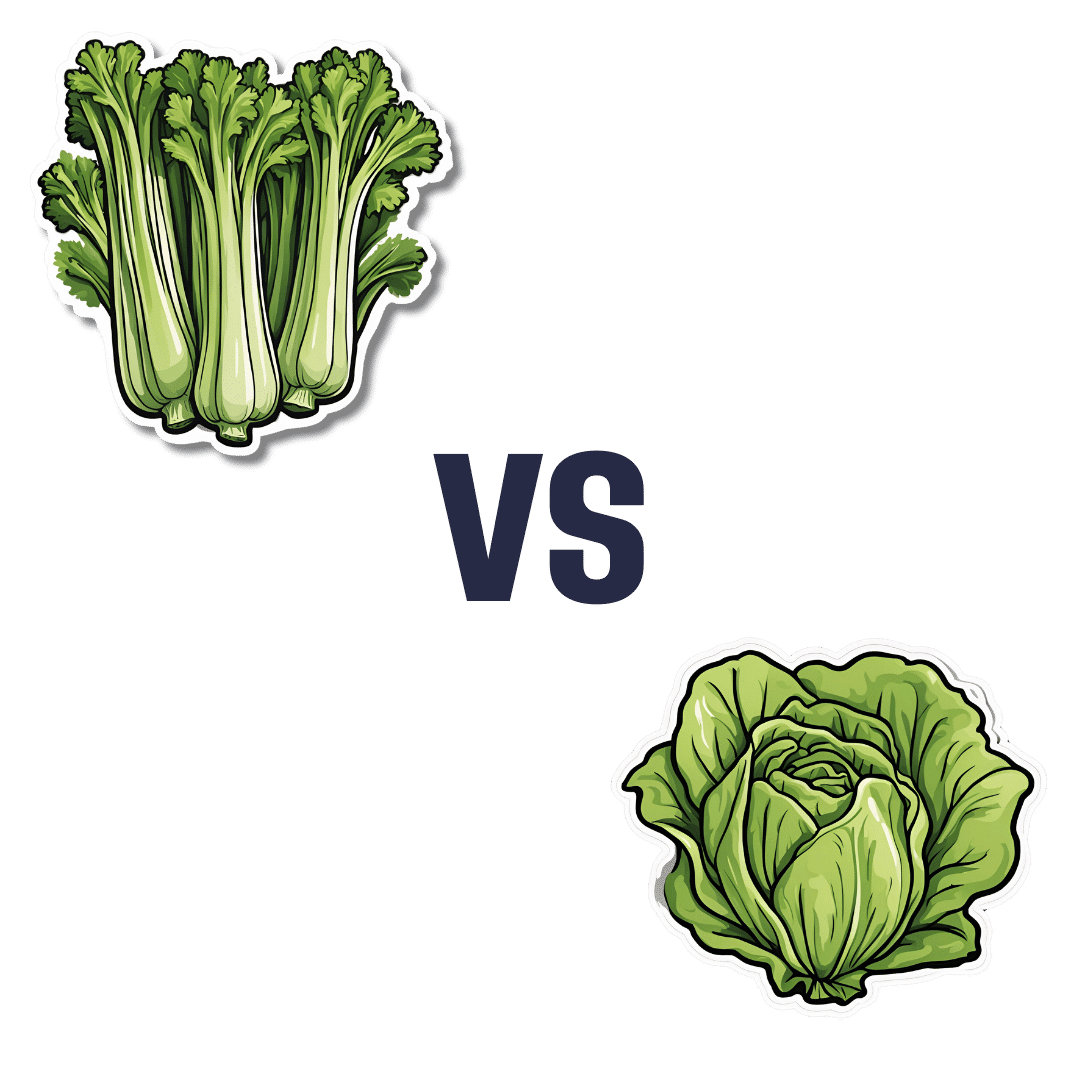
Celery vs Lettuce – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing celery to lettuce, we picked the lettuce.
Why?
Let us consider the macros first: lettuce has 2x the protein, but of course the numbers are tiny and probably nobody is eating this for the protein. Both of these salad items are roughly comparable in terms of carbs and fiber, being both mostly water with just enough other stuff to hold their shape. Nominally this section is a slight win for lettuce on account of the protein, but in realistic practical terms, it’s a tie.
In terms of vitamins, celery has more of vitamins B5 and E, while lettuce has more of vitamins A, B1, B2, B3, B6, B7, B9, C, K, and choline. An easy win for lettuce here.
In the category of minerals, celery has more calcium, copper, and potassium, while lettuce has more iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. So, a fair win for lettuce.
Adding up the sections makes for an overall win for lettuce; of course, enjoy both, though!
Want to learn more?
You might like to read:
Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Pear vs Peach – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pears to peaches, we picked the peaches.
Why?
Both are great! But peaches are exceptional in some ways that pears just can’t match up to:
In terms of macros, pears have more carbs and fiber, the ratio of which results in an approximately equal glycemic index. Thus, we’ll say that pears win this round by virtue of being the nutritionally denser option.
Looking at the vitamins, pears have (slightly) more of vitamins B6, B9, and K, while peaches have (much) more of vitamins A, B1, B2, B3, B5, B7, C, E, and choline—thus sweeping this category easily for peaches.
In the category of minerals, pears have more calcium and copper, while peaches have more iron, magnesium, manganese, phosphorus, potassium, and zinc. This time, the margins of difference for each mineral are comparably low (i.e. pears are close behind peaches on all those minerals), but still, by strength of numbers, it’s a clear win for peaches.
When it comes to polyphenols, not only do peaches have more, but also, they have anticancer properties that pears don’t—see our link below for more about that!
Meanwhile, adding up the sections makes for an overall win for peaches, but as ever when it comes to fruits, by all means enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer ← peaches in the #2 spot! They induce cell death in cancer cells while sparing healthy ones
Enjoy!
Share This Post
-
The Real Benefit Of Genetic Testing
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Genetic Testing: Health Benefits & Methods
Genetic testing is an oft-derided American pastime, but there’s a lot more to it than finding out about your ancestry!
Note: because there are relatively few companies offering health-related genetic testing services, and we are talking about the benefits of those services, some of this main feature may seem like an advert.
It’s not; none of those companies are sponsoring us, and if any of them become a sponsor at some point, we’ll make it clear and put it in the clearly-marked sponsor segment.
As ever, our only goal here is to provide science-backed information, to enable you to make your own, well-informed, decisions.
Health genomics & genetic testing
The basic goal of health genomics and genetic testing is to learn:
- What genetic conditions you have
- Clearcut genetic conditions, such as Fragile X syndrome, or Huntington’s disease
- What genetic predispositions you have
- Such as an increased/decreased risk for various kinds of cancer, diabetes, heart conditions, and so forth
- What genetic traits you have
- These may range from “blue eyes” to “superathlete muscle type”
- More specifically, pharmacogenomic information
- For example, “fast caffeine metabolizer” or “clopidogrel (Plavix) non-responder” (i.e., that drug simply will not work for you)
Wait, what’s the difference between health genomics and genetic testing?
- Health genomics is the science of how our genes affect our health.
- Genetic testing can be broadly defined as the means of finding out which genes we have.
A quick snippet…
More specifically, a lot of these services look at which single nucleotide polymorphisms (SNPs, pronounced “snips”) we have. While we share almost all of our DNA with each other (and indeed, with most vertebrates), our polymorphisms are the bits that differ, and are the bits that, genetically speaking, make us different.
So, by looking just at the SNPs, it means we “only” need to look at about 3,000,000 DNA positions, and not our entire genome. For perspective, those 3,000,000 DNA positions make up about 0.1% of our whole genome, so without focusing on SNPs, the task would be 1000x harder.
For example, the kind of information that this sort of testing may give you, includes (to look at some “popular” SNPs):
- rs53576 in the oxytocin receptor influences social behavior and personality
- rs7412 and rs429358 can raise the risk of Alzheimer’s disease by more than 10x
- rs6152 can influence baldness
- rs333 resistance to HIV
- rs1800497 in a dopamine receptor may influence the sense of pleasure
- rs1805007 determines red hair and sensitivity to anesthetics
- rs9939609 triggers obesity and type-2 diabetes
- rs662799 prevents weight gain from high fat diets
- rs12255372 linked to type-2 diabetes and breast cancer
- rs1799971 makes alcohol cravings stronger
- rs17822931 determines earwax, sweating and body odor
- rs1333049 coronary heart disease
- rs1051730 and rs3750344 nicotine dependence
- rs4988235 lactose intolerance
(You can learn about these and more than 100,000 other SNPs at SNPedia.com)
I don’t know what SNPs I have, and am disinclined to look them up one by one!
The first step to knowing, is to get your DNA out of your body and into a genetic testing service. This is usually done by saliva or blood sample. This writer got hers done many years ago by 23andMe and was very happy with that service, but there are plenty of other options.
Healthline did an independent review of the most popular companies, so you might like to check out:
Healthline: Best DNA Testing Kits of 2023
Those companies will give you some basic information, such as “6x higher breast cancer risk” or “3x lower age-related macular degeneration risk” etc.
However, to really get bang-for-buck, what you want to do next is:
- Get your raw genetic data (the companies above should provide it); this will probably look like a big text file full of As, Cs, Gs, and Ts, but it make take another form.
- Upload it to Promethease. When this writer got hers done , the cost was $2; that price has now gone up to a whopping $12.
- You will then get a report that will cross-reference your data with everything known about SNPs, and give a supremely comprehensive, readable-to-the-human-eye, explanation of what it all means for you—from much more specific health risk prognostics, to more trivial things like whether you can roll your tongue or smell decomposed asparagus metabolites in urine.
A note on privacy: anything you upload to Promethease will be anonymized, and/but in doing so, you consent to it going into the grand scientific open-source bank of “things we know about the human genome”, and thus contribute to the overall sample size of genetic data.
In our opinion, it means you’re doing your bit for science, without personal risk. But your opinion may differ, and that’s your decision to make.
Lastly, on the pros and cons of pharmacogenetic testing specifically:
Share This Post
- What genetic conditions you have
-
Continuous Glucose Monitors Without Diabetes: Pros & Cons
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The “Glucose Goddess”, biochemist Jessie Inchauspé, gives us the low-down:
Knowledge is power (but watch out)
A continuous glucose monitor (CGM) is a device that continually monitors glucose levels, without the need to stab one’s finger every few hours to test blood.
It was designed for diabetics, especially for those with Type 1 Diabetes, where around-the-clock monitoring is necessary for appropriate insulin dosing.
For non-diabetics, they can be a good way of learning what our body’s response to various foods and activities is like, the better to be able to tweak our habits to avoid undue glucose spikes (which are harmful for our pancreas, liver, heart, brain, kidneys, and more).
How it works: there’s a sensor that sits on the arm (or elsewhere, but the arm is a popular placement) with a little probe that goes under the skin. It’s applied using a device that inserts it automatically using a needle (you only need to press a button, you don’t need to guide the needle yourself); the needle then retracts, leaving the soft, flexible probe in place. Having been attached, that sensor can now stay in place for 2 weeks (usually; depends on brand, but for example FreeStyle Libre, the most popular brand, the sensors last 2 weeks), and yes, it’s fine to bathe/shower/etc with it. When you want an update from your CGM, you scan it with your phone (or you can buy a dedicated reader, but that is more expensive and unnecessary), and it uploads the data since your last scan.
Pros: it’s convenient and gives a lot of data, so even if you only use it for a short period of time (for example, a month) you can get a very good idea of what affects your blood sugar levels and how. Also, because of the constant nature of the monitoring, it helps avoid accidental sample bias of the kind that can occur with manual testing, by testing a little too soon or too late, and missing a spike/dip.
Cons: it can be expensive, depending on where you live and what options are available for you locally, so you might not want to do it long-term (since that would require buying two sensors per month). It’s also, for all its wealth of data, slightly less accurate than fingerprick testing—that’s because it takes an interstitial reading instead of directly from the blood. For this reason, if you test both ways, you may find a discrepancy of about 3mg/dL. Given that the healthy range is about 70–140mg/dL, a discrepancy of 3mg/dL is probably not going to be important, but it is a thing to mention can (and probably will) happen.
Patterns to bear in mind (with any kind of blood sugar monitoring):
- Dawn phenomenon: a natural glucose rise upon waking.
- Exercise-induced spikes (normal due to energy demands).
- Fat in meals slowing glucose absorption.
- Different foods can sometimes cause a double-wave after dinner (because glucose from different foods is absorbed differently, and/or different foods affect insulin response independent of glucose)
- Steep, rapid spikes that are more harmful than gradual, sustained increases.
- Vitamin C spikes: temporary chemical interference with the sensor, not actual glucose rises.
- Nighttime glucose dips (often false readings caused by sleeping position).
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
10 Ways To Balance Blood Sugars
Take care!
Share This Post
Related Posts
-
Solitary Fitness – by Charles Bronson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sometimes it can seem that every new diet and/or exercise regime you want to try will change your life, if just you first max out your credit card on restocking your kitchen and refurbishing your home gym, not to mention buying all the best supplements, enjoying the latest medical gadgets, and so on and so forth.
And often… Most of those things genuinely are good! And it’s great that such things are becoming more accessible and available.
But… Wouldn’t it be nice to know how to have excellent strength and fitness without any of that, even if just as a “bare bones” protocol to fall back on? That’s what Manson provides in this book.
The writing style is casual and friendly; Manson is not exactly an academic, but he knows his stuff when it comes to what works. And a good general rule of thumb is: if it’s something that he can do in his jail cell, we can surely do it in the comfort of our homes.
Bottom line: if you want functional strength and fitness with zero gimmicks, this is the book for you (as an aside, it’s also simply an interesting and recommendable read, sociologically speaking, but that’s another matter entirely).
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tourette’s Syndrome Treatment Options
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Is there anything special that might help someone with Tourette’s syndrome?❞
There are of course a lot of different manifestations of Tourette’s syndrome, and some people’s tics may be far more problematic to themselves and/or others, while some may be quite mild and just something to work around.
It’s an interesting topic for sure, so we’ll perhaps do a main feature (probably also covering the related-and-sometimes-overlapping OCD umbrella rather than making it hyperspecific to Tourette’s), but meanwhile, you might consider some of these options:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Paracetamol pack sizes and availability are changing. Here’s what you need to know
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Changes are coming into effect from February 1 about how paracetamol is sold in Australia.
This mainly affects pack sizes of paracetamol sold outside pharmacies and how paracetamol is accessed in pharmacies.
The changes, announced by Australia’s drug regulator, are in line with moves internationally to reduce the harms of liver toxicity and the risk of overdose.
However, there are no new safety concerns when paracetamol is used as directed. And children’s products are not affected.
Bowonpat Sakaew/Shutterstock What is paracetamol?
Paracetamol is commonly sold under brand names such as Panadol, Dymadon and Panamax. It’s used to treat mild pain and fever for short periods or can be prescribed for chronic (long-term) pain.
Millions of packs of this cheap and accessible medicine are sold in Australia every year.
Small packs (up to 20 tablets) have been available from supermarkets and other retailers such as petrol stations. Larger packs (up to 100 tablets) are only available from pharmacies.
Paracetamol is relatively safe when used as directed. However, at higher-than-recommended doses, it can cause liver toxicity. In severe cases and when left untreated, this can be lethal.
Why are the rules changing?
In 2022, we wrote about how the Therapeutic Goods Administration (TGA) was considering changes to paracetamol access because of an increase in people going to hospital with paracetamol poisoning.
An expert review it commissioned found there were about 40–50 deaths every year from paracetamol poisoning between 2007 and 2020. Between 2009–10 and 2016–17, hospital admissions for this increased (from 8,617 to 11,697), before reducing in 2019–20 (8,723). Most admissions were due to intentional self-poisonings, and about half of these were among people aged ten to 24.
After the report, the TGA consulted with the public to work out how to prevent paracetamol poisonings.
Options included reducing pack sizes, limiting how many packs could be bought at once, moving larger packs behind the pharmacy counter and restricting access by age.
Responses were mixed. Although responses supported the need to prevent poisonings, there were concerns about how changes might affect:
- people with chronic pain, especially those in regional areas, where it may be harder to access pharmacies and, therefore, larger packs
- people on limited incomes, if certain products were made prescription-only.
Although deaths from paracetamol poisoning are tragic and preventable, they are rare considering how much paracetamol Australians use. There is less than one death due to poisoning for every million packs sold.
Because of this, it was important the TGA addressed concerns about poisonings while making sure Australians still had easy access to this essential medicine.
If you buy large packs of paracetamol for chronic pain, you’ll need to go to the pharmacy counter. StratfordProductions/Shutterstock So what’s changing?
The key changes being introduced relate to new rules about the pack sizes that can be sold outside pharmacies, and the location of products sold in pharmacies.
From February 1, packs sold in supermarkets and places other than pharmacies will reduce from a maximum 20 tablets to 16 tablets per pack. These changes bring Australia in line with other countries. These include the United Kingdom, which restricted supermarket packs to 16 tablets in 1998, and saw reductions in poisonings.
In all jurisdictions except Queensland and Western Australia, packs sold in pharmacies larger than 50 tablets will move behind the pharmacy counter and can only be sold under pharmacist supervision. In Queensland and WA, products containing more than 16 tablets will only be available from behind the pharmacy counter and sold under pharmacist supervision.
In all jurisdictions, any packs containing more than 50 tablets will need to be sold in blister packs, rather than bottles.
Several paracetamol products are not affected by these changes. These include children’s products, slow-release formulations (for example, “osteo” products), and products already behind the pharmacy counter or only available via prescription.
What else do I need to know?
These changes have been introduced to reduce the risk of poisonings from people exceeding recommended doses. The overall safety profile of paracetamol has not changed.
Paracetamol is still available from all current locations and there are no plans to make it prescription-only or remove it from supermarkets altogether. Many companies have already been updating their packaging to ensure there are no gaps in supply.
The reduction in pack sizes of paracetamol available in supermarkets means a pack of 16 tablets will now last two days instead of two-and-a-half days if taken at the maximum dose (two tablets, four times a day). Anyone in pain that does not improve after short-term use should speak to their pharmacist or GP.
For people who use paracetamol regularly for chronic pain, it is more cost-effective to continue buying larger packs from pharmacies. As larger packs (50+ tablets) need to be kept out of sight, you will need to ask at the pharmacy counter. Pharmacists know that for many people it’s appropriate to use paracetamol daily for chronic pain.
Natasa Gisev, Clinical pharmacist and Scientia Associate Professor at the National Drug and Alcohol Research Centre, UNSW Sydney and Ria Hopkins, Postdoctoral Research Fellow, National Drug and Alcohol Research Centre, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: