Cantaloupe vs Cucumber – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cantaloupe to cucumber, we picked the cucumber.
Why?
In terms of macros, both are of course 90–95% water, with just enough fiber to hold them together. However, it’s cantaloupe that’s 90% water and cucumber that’s 95% water, because cantaloupe has more than 2x the carbs and 144x the sugar (whence the sweetness). Now, it’s a fruit and so this sugar isn’t really anything to worry about if you’re eating it in solid form (as opposed to as juice), but by the numbers, it does mean that cucumber has the much lower glycemic index (cucumber has a GI of 21, while cantaloupe has a GI of 65), so we’ll give cucumber the win in this category.
In the category of vitamins, cantaloupe has more of vitamins A, B3, B6, B9, C, and E, while cucumber has more of vitamins B2, B5, and K, so cantaloupe scores a 6:3 win in this round.
When it comes to minerals, cantaloupe has more potassium and selenium, while cucumber has more calcium, iron, magnesium, manganese, phosphorus, and zinc, so another win for cucumber here.
Looking at polyphenols, cantaloupe has almost nothing (trace amounts of some lignans), while cucumber has more of the same lignans that cantaloupe has, plus highly beneficial flavones apigenin and luteolin, and famously good flavonols like kaempferol and quercetin. So, one more win for cucumber here.
Plus, and it’s not yet known the mechanism of action for this one, but cucumber extract beats glucosamine and chondroitin for reducing joint inflammation, at 1/135th of the dose.
Adding up the sections makes for a very clear overall win for cucumber, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
What’s Your Plant Diversity Score?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Pain Doesn’t Belong on a Scale of Zero to 10
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Over the past two years, a simple but baffling request has preceded most of my encounters with medical professionals: “Rate your pain on a scale of zero to 10.”
I trained as a physician and have asked patients the very same question thousands of times, so I think hard about how to quantify the sum of the sore hips, the prickly thighs, and the numbing, itchy pain near my left shoulder blade. I pause and then, mostly arbitrarily, choose a number. “Three or four?” I venture, knowing the real answer is long, complicated, and not measurable in this one-dimensional way.
Pain is a squirrely thing. It’s sometimes burning, sometimes drilling, sometimes a deep-in-the-muscles clenching ache. Mine can depend on my mood or how much attention I afford it and can recede nearly entirely if I’m engrossed in a film or a task. Pain can also be disabling enough to cancel vacations, or so overwhelming that it leads people to opioid addiction. Even 10+ pain can be bearable when it’s endured for good reason, like giving birth to a child. But what’s the purpose of the pains I have now, the lingering effects of a head injury?
The concept of reducing these shades of pain to a single number dates to the 1970s. But the zero-to-10 scale is ubiquitous today because of what was called a “pain revolution” in the ’90s, when intense new attention to addressing pain — primarily with opioids — was framed as progress. Doctors today have a fuller understanding of treating pain, as well as the terrible consequences of prescribing opioids so readily. What they are learning only now is how to better measure pain and treat its many forms.
About 30 years ago, physicians who championed the use of opioids gave robust new life to what had been a niche specialty: pain management. They started pushing the idea that pain should be measured at every appointment as a “fifth vital sign.” The American Pain Society went as far as copyrighting the phrase. But unlike the other vital signs — blood pressure, temperature, heart rate, and breathing rate — pain had no objective scale. How to measure the unmeasurable? The society encouraged doctors and nurses to use the zero-to-10 rating system. Around that time, the FDA approved OxyContin, a slow-release opioid painkiller made by Purdue Pharma. The drugmaker itself encouraged doctors to routinely record and treat pain, and aggressively marketed opioids as an obvious solution.
To be fair, in an era when pain was too often ignored or undertreated, the zero-to-10 rating system could be regarded as an advance. Morphine pumps were not available for those cancer patients I saw in the ’80s, even those in agonizing pain from cancer in their bones; doctors regarded pain as an inevitable part of disease. In the emergency room where I practiced in the early ’90s, prescribing even a few opioid pills was a hassle: It required asking the head nurse to unlock a special prescription pad and making a copy for the state agency that tracked prescribing patterns. Regulators (rightly) worried that handing out narcotics would lead to addiction. As a result, some patients in need of relief likely went without.
After pain doctors and opioid manufacturers campaigned for broader use of opioids — claiming that newer forms were not addictive, or much less so than previous incarnations — prescribing the drugs became far easier and were promoted for all kinds of pain, whether from knee arthritis or back problems. As a young doctor joining the “pain revolution,” I probably asked patients thousands of times to rate their pain on a scale of zero to 10 and wrote many scripts each week for pain medication, as monitoring “the fifth vital sign” quickly became routine in the medical system. In time, a zero-to-10 pain measurement became a necessary box to fill in electronic medical records. The Joint Commission on the Accreditation of Healthcare Organizations made regularly assessing pain a prerequisite for medical centers receiving federal health care dollars. Medical groups added treatment of pain to their list of patient rights, and satisfaction with pain treatment became a component of post-visit patient surveys. (A poor showing could mean lower reimbursement from some insurers.)
But this approach to pain management had clear drawbacks. Studies accumulated showing that measuring patients’ pain didn’t result in better pain control. Doctors showed little interest in or didn’t know how to respond to the recorded answer. And patients’ satisfaction with their doctors’ discussion of pain didn’t necessarily mean they got adequate treatment. At the same time, the drugs were fueling the growing opioid epidemic. Research showed that an estimated 3% to 19% of people who received a prescription for pain medication from a doctor developed an addiction.
Doctors who wanted to treat pain had few other options, though. “We had a good sense that these drugs weren’t the only way to manage pain,” Linda Porter, director of the National Institutes of Health’s Office of Pain Policy and Planning, told me. “But we didn’t have a good understanding of the complexity or alternatives.” The enthusiasm for narcotics left many varietals of pain underexplored and undertreated for years. Only in 2018, a year when nearly 50,000 Americans died of an overdose, did Congress start funding a program — the Early Phase Pain Investigation Clinical Network, or EPPIC-Net — designed to explore types of pain and find better solutions. The network connects specialists at 12 academic specialized clinical centers and is meant to jump-start new research in the field and find bespoke solutions for different kinds of pain.
A zero-to-10 scale may make sense in certain situations, such as when a nurse uses it to adjust a medication dose for a patient hospitalized after surgery or an accident. And researchers and pain specialists have tried to create better rating tools — dozens, in fact, none of which was adequate to capture pain’s complexity, a European panel of experts concluded. The Veterans Health Administration, for instance, created one that had supplemental questions and visual prompts: A rating of 5 correlated with a frown and a pain level that “interrupts some activities.” The survey took much longer to administer and produced results that were no better than the zero-to-10 system. By the 2010s, many medical organizations, including the American Medical Association and the American Academy of Family Physicians, were rejecting not just the zero-to-10 scale but the entire notion that pain could be meaningfully self-reported numerically by a patient.
In the years that opioids had dominated pain remedies, a few drugs — such as gabapentin and pregabalin for neuropathy, and lidocaine patches and creams for musculoskeletal aches — had become available. “There was a growing awareness of the incredible complexity of pain — that you would have to find the right drugs for the right patients,” Rebecca Hommer, EPPIC-Net’s interim director, told me. Researchers are now looking for biomarkers associated with different kinds of pain so that drug studies can use more objective measures to assess the medications’ effect. A better understanding of the neural pathways and neurotransmitters that create different types of pain could also help researchers design drugs to interrupt and tame them.
Any treatments that come out of this research are unlikely to be blockbusters like opioids; by design, they will be useful to fewer people. That also makes them less appealing prospects to drug companies. So EPPIC-Net is helping small drug companies, academics, and even individual doctors design and conduct early-stage trials to test the safety and efficacy of promising pain-taming molecules. That information will be handed over to drug manufacturers for late-stage trials, all with the aim of getting new drugs approved by the FDA more quickly.
The first EPPIC-Net trials are just getting underway. Finding better treatments will be no easy task, because the nervous system is a largely unexplored universe of molecules, cells, and electronic connections that interact in countless ways. The 2021 Nobel Prize in Physiology or Medicine went to scientists who discovered the mechanisms that allow us to feel the most basic sensations: cold and hot. In comparison, pain is a hydra. A simple number might feel definitive. But it’s not helping anyone make the pain go away.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
It’s OK That You’re Not OK – by Megan Devine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Firstly, be aware: this is not a cheerful book. If you’re looking for something to life your mood after a loss, it will not be this.
What, then, will you find? A reminder that grief is also the final translation of love, and not necessarily something to be put aside as quickly as possible—or even ever, if we don’t want to.
Too often, society (and even therapists) will correctly note that no two instances of grief are the same (after all, no two people are, so definitely no two relationships are, so how could two instances of grief be?), but will still expect that if most people can move on quickly from most losses, that you should too, and that if you don’t then there is something pathological at hand that needs fixing.
Part one of the book covers this (and more) in a lot of detail; critics have called it a diatribe against the current status quo in the field of grief.
Part two of the book is about “what to do with your grief”, and addresses the reality of grief, how (and why) to stay alive when not doing so feels like a compelling option, dealing with grief’s physical side effects, and calming your mind in ways that actually work (without trying to sweep your grief under a rug).
Parts three and four are more about community—how to navigate the likely unhelpful efforts a lot of people may make in the early days, and when it comes to those people who can and will actually be a support, how to help them to help you.
In the category of criticism, she also plugs her own (paid, subscription-based) online community, which feels a little mercenary, especially as while community definitely can indeed help, the prospect of being promptly exiled from it if you stop paying, doesn’t.
Bottom line: if you have experienced grief and felt like moving on was the right thing to do, then this book isn’t the one for you. If, on the other hand, your grief feels more like something you will carry just as you carry the love you feel for them, then you’ll find a lot about that here.
Share This Post
-
What are ‘collarium’ sunbeds? Here’s why you should stay away
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Reports have recently emerged that solariums, or sunbeds – largely banned in Australia because they increase the risk of skin cancer – are being rebranded as “collarium” sunbeds (“coll” being short for collagen).
Commercial tanning and beauty salons in Queensland, New South Wales and Victoria are marketing collariums, with manufacturers and operators claiming they provide a longer lasting tan and stimulate collagen production, among other purported benefits.
A collarium sunbed emits both UV radiation and a mix of visible wavelength colours to produce a pink or red light. Like an old-school sunbed, the user lies in it for ten to 20 minute sessions to quickly develop a tan.
But as several experts have argued, the providers’ claims about safety and effectiveness don’t stack up.
Why were sunbeds banned?
Commercial sunbeds have been illegal across Australia since 2016 (except for in the Northern Territory) under state-based radiation safety laws. It’s still legal to sell and own a sunbed for private use.
Their dangers were highlighted by young Australians including Clare Oliver who developed melanoma after using sunbeds. Oliver featured in the No Tan Is Worth Dying For campaign and died from her melanoma at age 26 in 2007.
Sunbeds lead to tanning by emitting UV radiation – as much as six times the amount of UV we’re exposed to from the summer sun. When the skin detects enough DNA damage, it boosts the production of melanin, the brown pigment that gives you the tanned look, to try to filter some UV out before it hits the DNA. This is only partially successful, providing the equivalent of two to four SPF.
Essentially, if your body is producing a tan, it has detected a significant amount of DNA damage in your skin.
Research shows people who have used sunbeds at least once have a 41% increased risk of developing melanoma, while ten or more sunbed sessions led to a 100% increased risk.
In 2008, Australian researchers estimated that each year, sunbeds caused 281 cases of melanoma, 2,572 cases of squamous cell carcinoma (another common type of skin cancer), and $3 million in heath-care costs, mostly to Medicare.
How are collarium sunbeds supposed to be different?
Australian sellers of collarium sunbeds imply they are safe, but their machine descriptions note the use of UV radiation, particularly UVA.
UVA is one part of the spectrum of UV radiation. It penetrates deeper into the skin than UVB. While UVB promotes cancer-causing mutations by discharging energy straight into the DNA strand, UVA sets off damage by creating reactive oxygen species, which are unstable compounds that react easily with many types of cell structures and molecules. These damage cell membranes, protein structures and DNA.
Evidence shows all types of sunbeds increase the risk of melanoma, including those that use only UVA.
Some manufacturers and clinics suggest the machine’s light spectrum increases UV compatibility, but it’s not clear what this means. Adding red or pink light to the mix won’t negate the harm from the UV. If you’re getting a tan, you have a significant amount of DNA damage.
Collagen claims
One particularly odd claim about collarium sunbeds is that they stimulate collagen.
Collagen is the main supportive tissue in our skin. It provides elasticity and strength, and a youthful appearance. Collagen is constantly synthesised and broken down, and when the balance between production and recycling is lost, the skin loses strength and develops wrinkles. The collagen bundles become thin and fragmented. This is a natural part of ageing, but is accelerated by UV exposure.
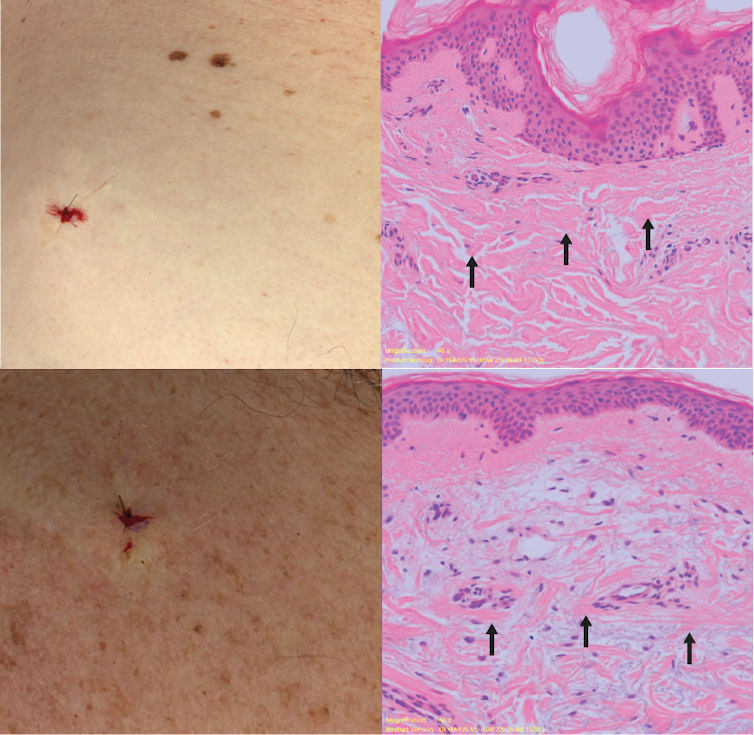
Sun-protected skin (top) has thick bands of pink collagen (arrows) in the dermis, as seen on microscopic examination. Chronically sun-damaged skin (bottom) has much thinner collagen bands.
Katie Lee/UQThe reactive oxygen species generated by UVA light damage existing collagen structures and kick off a molecular chain of events that downgrades collagen-producing enzymes and increases collagen-destroying enzymes. Over time, a build-up of degraded collagen fragments in the skin promotes even more destruction.
While there is growing evidence red light therapy alone could be useful in wound healing and skin rejuvenation, the UV radiation in collarium sunbeds is likely to undo any benefit from the red light.
What about phototherapy?
There are medical treatments that use controlled UV radiation doses to treat chronic inflammatory skin diseases like psoriasis.
The anti-collagen effects of UVA can also be used to treat thickened scars and keloids. Side-effects of UV phototherapy include tanning, itchiness, dryness, cold sore virus reactivation and, notably, premature skin ageing.
These treatments use the minimum exposure necessary to treat the condition, and are usually restricted to the affected body part to minimise risks of future cancer. They are administered under medical supervision and are not recommended for people already at high risk of skin cancer, such as people with atypical moles.
So what happens now?
It looks like many collariums are just sunbeds rebranded with red light. Queensland Health is currently investigating whether these salons are breaching the state’s Radiation Safety Act, and operators could face large fines.
As the 2024 Australians of the Year – melanoma treatment pioneers Georgina Long and Richard Scolyer – highlighted in their acceptance speech, “there is nothing healthy about a tan”, and we need to stop glamorising tanning.
However, if you’re desperate for the tanned look, there is a safer and easy way to get one – out of a bottle or by visiting a salon for a spray tan.
Katie Lee, PhD Candidate, Dermatology Research Centre, The University of Queensland and Anne Cust, Professor of Cancer Epidemiology, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
What Your Doctor Wants You to Know to Crush Medical Debt – by Dr. Virgie Ellington
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First things first: this one’s really only of relevance to people living in the US. That’s most of our readership, but if it’s not you, then apologies, this one won’t be of interest.
For the US Americans, though, Dr. Ellington starts strong with “you got a bill—now get the right bill”, and then gives a step-by-step process for finding the mistakes in your medical bills, fixing them, dealing with insurers who do not want to live up to their part of the bargain, and how to minimize what you need to pay, when you actually arrive at your final bill.
The biggest strength of this book is the wealth of insider knowledge (the author has worked as a primary care physician as well as as a health insurance executive), and while this information won’t stay current forever, its relatively recent publication date (2022) means that little has changed since then, and once you’re up to speed with how things are now, it’ll be easy to roll with whatever changes may come in the future.
Bottom line: if you’re living in the US and would like to not be ripped off as badly as possible when it comes to healthcare costs, this book is a very small, very powerful, investment.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How light can shift your mood and mental health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is the next article in our ‘Light and health’ series, where we look at how light affects our physical and mental health in sometimes surprising ways. Read other articles in the series.
It’s spring and you’ve probably noticed a change in when the Sun rises and sets. But have you also noticed a change in your mood?
We’ve known for a while that light plays a role in our wellbeing. Many of us tend to feel more positive when spring returns.
But for others, big changes in light, such as at the start of spring, can be tough. And for many, bright light at night can be a problem. Here’s what’s going on.
llaszlo/Shutterstock An ancient rhythm of light and mood
In an earlier article in our series, we learned that light shining on the back of the eye sends “timing signals” to the brain and the master clock of the circadian system. This clock coordinates our daily (circadian) rhythms.
“Clock genes” also regulate circadian rhythms. These genes control the timing of when many other genes turn on and off during the 24-hour, light-dark cycle.
But how is this all linked with our mood and mental health?
Circadian rhythms can be disrupted. This can happen if there are problems with how the body clock develops or functions, or if someone is routinely exposed to bright light at night.
When circadian disruption happens, it increases the risk of certain mental disorders. These include bipolar disorder and atypical depression (a type of depression when someone is extra sleepy and has problems with their energy and metabolism).
Light on the brain
Light may also affect circuits in the brain that control mood, as animal studies show.
There’s evidence this happens in humans. A brain-imaging study showed exposure to bright light in the daytime while inside the scanner changed the activity of a brain region involved in mood and alertness.
Another brain-imaging study found a link between daily exposure to sunlight and how the neurotransmitter (or chemical messenger) serotonin binds to receptors in the brain. We see alterations in serotonin binding in several mental disorders, including depression.
Our mood can lift in sunlight for a number of reasons, related to our genes, brain and hormones. New Africa/Shutterstock What happens when the seasons change?
Light can also affect mood and mental health as the seasons change. During autumn and winter, symptoms such as low mood and fatigue can develop. But often, once spring and summer come round, these symptoms go away. This is called “seasonality” or, when severe, “seasonal affective disorder”.
What is less well known is that for other people, the change to spring and summer (when there is more light) can also come with a change in mood and mental health. Some people experience increases in energy and the drive to be active. This is positive for some but can be seriously destabilising for others. This too is an example of seasonality.
Most people aren’t very seasonal. But for those who are, seasonality has a genetic component. Relatives of people with seasonal affective disorder are more likely to also experience seasonality.
Seasonality is also more common in conditions such as bipolar disorder. For many people with such conditions, the shift into shorter day-lengths during winter can trigger a depressive episode.
Counterintuitively, the longer day-lengths in spring and summer can also destabilise people with bipolar disorder into an “activated” state where energy and activity are in overdrive, and symptoms are harder to manage. So, seasonality can be serious.
Alexis Hutcheon, who experiences seasonality and helped write this article, told us:
[…] the season change is like preparing for battle – I never know what’s coming, and I rarely come out unscathed. I’ve experienced both hypomanic and depressive episodes triggered by the season change, but regardless of whether I’m on the ‘up’ or the ‘down’, the one constant is that I can’t sleep. To manage, I try to stick to a strict routine, tweak medication, maximise my exposure to light, and always stay tuned in to those subtle shifts in mood. It’s a time of heightened awareness and trying to stay one step ahead.
So what’s going on in the brain?
One explanation for what’s going on in the brain when mental health fluctuates with the change in seasons relates to the neurotransmitters serotonin and dopamine.
Serotonin helps regulate mood and is the target of many antidepressants. There is some evidence of seasonal changes in serotonin levels, potentially being lower in winter.
Dopamine is a neurotransmitter involved in reward, motivation and movement, and is also a target of some antidepressants. Levels of dopamine may also change with the seasons.
But the neuroscience of seasonality is a developing area and more research is needed to know what’s going on in the brain.
How about bright light at night?
We know exposure to bright light at night (for instance, if someone is up all night) can disturb someone’s circadian rhythms.
This type of circadian rhythm disturbance is associated with higher rates of symptoms including self-harm, depressive and anxiety symptoms, and lower wellbeing. It is also associated with higher rates of mental disorders, such as major depression, bipolar disorder, psychotic disorders and post-traumatic stress disorder (or PTSD).
Why is this? Bright light at night confuses and destabilises the body clock. It disrupts the rhythmic regulation of mood, cognition, appetite, metabolism and many other mental processes.
But people differ hugely in their sensitivity to light. While still a hypothesis, people who are most sensitive to light may be the most vulnerable to body clock disturbances caused by bright light at night, which then leads to a higher risk of mental health problems.
Bright light at night disrupts your body clock, putting you at greater risk of mental health issues. Ollyy/Shutterstock Where to from here?
Learning about light will help people better manage their mental health conditions.
By encouraging people to better align their lives to the light-dark cycle (to stabilise their body clock) we may also help prevent conditions such as depression and bipolar disorder emerging in the first place.
Healthy light behaviours – avoiding light at night and seeking light during the day – are good for everyone. But they might be especially helpful for people at risk of mental health problems. These include people with a family history of mental health problems or people who are night owls (late sleepers and late risers), who are more at risk of body clock disturbances.
Alexis Hutcheon has lived experience of a mental health condition and helped write this article.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14.
Jacob Crouse, Research Fellow in Youth Mental Health, Brain and Mind Centre, University of Sydney; Emiliana Tonini, Postdoctoral Research Fellow, Brain and Mind Centre, University of Sydney, and Ian Hickie, Co-Director, Health and Policy, Brain and Mind Centre, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Apple vs Pineapple – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing apple to pineapple, we picked the pineapple.
Why?
An apple a day may keep the doctor away, but pineapples are heavier and armored and spiky and generally much more intimidating.
More seriously, apples are great but we say pineapples have the better nutritional and phytochemical properties overall:
In terms of macros, actually apples win this first round, albeit marginally; the two fruits are equal on carbs, while apple has a little more fiber and pineapple has a (very) little more protein. This makes the fiber content the deciding factor, so apples do win this one, even if by just 1g/100g difference.
When it comes to vitamins, however, apples have more of vitamins E and K, while pineapple has more of vitamins A, B1, B2, B3, B5, B6, B7, B9, C, and choline. The margins of difference are equally generous on both sides, so this is a clear and overwhelming win for pineapple (including 10x more vitamin C than apples, which are themselves considered a good source of vitamin C)
In the category of minerals, apples have slightly more phosphorus, and pineapple has a lot more calcium, copper, iron, magnesium, manganese, potassium, selenium, and zinc. Another easy win for pineapple.
Pineapples are not only also higher in polyphenols, but also contain bromelain, a powerful anti-inflammatory group of enzymes that are unique to pineapple—you can read about it in the link below!
Meanwhile, pineapple wins the day in our head-to-head here, but as ever when it comes to a plurality of healthy things, do enjoy either or both! Diversity is good.
Want to learn more?
You might like to read:
Bromelain vs Inflammation & Much More
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: