Can a drug like Ozempic help treat addictions to alcohol, opioids or other substances?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Semaglutide (sold as Ozempic, Wegovy and Rybelsus) was initially developed to treat diabetes. It works by stimulating the production of insulin to keep blood sugar levels in check.
This type of drug is increasingly being prescribed for weight loss, despite the fact it was initially approved for another purpose. Recently, there has been growing interest in another possible use: to treat addiction.
Anecdotal reports from patients taking semaglutide for weight loss suggest it reduces their appetite and craving for food, but surprisingly, it also may reduce their desire to drink alcohol, smoke cigarettes or take other drugs.
But does the research evidence back this up?
Animal studies show positive results
Semaglutide works on glucagon-like peptide-1 receptors and is known as a “GLP-1 agonist”.
Animal studies in rodents and monkeys have been overwhelmingly positive. Studies suggest GLP-1 agonists can reduce drug consumption and the rewarding value of drugs, including alcohol, nicotine, cocaine and opioids.
Out team has reviewed the evidence and found more than 30 different pre-clinical studies have been conducted. The majority show positive results in reducing drug and alcohol consumption or cravings. More than half of these studies focus specifically on alcohol use.
However, translating research evidence from animal models to people living with addiction is challenging. Although these results are promising, it’s still too early to tell if it will be safe and effective in humans with alcohol use disorder, nicotine addiction or another drug dependence.
What about research in humans?
Research findings are mixed in human studies.
Only one large randomised controlled trial has been conducted so far on alcohol. This study of 127 people found no difference between exenatide (a GLP-1 agonist) and placebo (a sham treatment) in reducing alcohol use or heavy drinking over 26 weeks.
In fact, everyone in the study reduced their drinking, both people on active medication and in the placebo group.
However, the authors conducted further analyses to examine changes in drinking in relation to weight. They found there was a reduction in drinking for people who had both alcohol use problems and obesity.
For people who started at a normal weight (BMI less than 30), despite initial reductions in drinking, they observed a rebound increase in levels of heavy drinking after four weeks of medication, with an overall increase in heavy drinking days relative to those who took the placebo.
There were no differences between groups for other measures of drinking, such as cravings.

In another 12-week trial, researchers found the GLP-1 agonist dulaglutide did not help to reduce smoking.
However, people receiving GLP-1 agonist dulaglutide drank 29% less alcohol than those on the placebo. Over 90% of people in this study also had obesity.
Smaller studies have looked at GLP-1 agonists short-term for cocaine and opioids, with mixed results.
There are currently many other clinical studies of GLP-1 agonists and alcohol and other addictive disorders underway.
While we await findings from bigger studies, it’s difficult to interpret the conflicting results. These differences in treatment response may come from individual differences that affect addiction, including physical and mental health problems.
Larger studies in broader populations of people will tell us more about whether GLP-1 agonists will work for addiction, and if so, for whom.
How might these drugs work for addiction?
The exact way GLP-1 agonists act are not yet well understood, however in addition to reducing consumption (of food or drugs), they also may reduce cravings.
Animal studies show GLP-1 agonists reduce craving for cocaine and opioids.
This may involve a key are of the brain reward circuit, the ventral striatum, with experimenters showing if they directly administer GLP-1 agonists into this region, rats show reduced “craving” for oxycodone or cocaine, possibly through reducing drug-induced dopamine release.
Using human brain imaging, experimenters can elicit craving by showing images (cues) associated with alcohol. The GLP-1 agonist exenatide reduced brain activity in response to an alcohol cue. Researchers saw reduced brain activity in the ventral striatum and septal areas of the brain, which connect to regions that regulate emotion, like the amygdala.
In studies in humans, it remains unclear whether GLP-1 agonists act directly to reduce cravings for alcohol or other drugs. This needs to be directly assessed in future research, alongside any reductions in use.
Are these drugs safe to use for addiction?
Overall, GLP-1 agonists have been shown to be relatively safe in healthy adults, and in people with diabetes or obesity. However side effects do include nausea, digestive troubles and headaches.
And while some people are OK with losing weight as a side effect, others aren’t. If someone is already underweight, for example, this drug might not be suitable for them.
In addition, very few studies have been conducted in people with addictive disorders. Yet some side effects may be more of an issue in people with addiction. Recent research, for instance, points to a rare risk of pancreatitis associated with GLP-1 agonists, and people with alcohol use problems already have a higher risk of this disorder.
Other drugs treatments are currently available
Although emerging research on GLP-1 agonists for addiction is an exciting development, much more research needs to be done to know the risks and benefits of these GLP-1 agonists for people living with addiction.
In the meantime, existing effective medications for addiction remain under-prescribed. Only about 3% of Australians with alcohol dependence, for example, are prescribed medication treatments such as like naltrexone, acamprosate or disulfiram. We need to ensure current medication treatments are accessible and health providers know how to prescribe them.
Continued innovation in addiction treatment is also essential. Our team is leading research towards other individualised and effective medications for alcohol dependence, while others are investigating treatments for nicotine addiction and other drug dependence.
Read the other articles in The Conversation’s Ozempic series here.
Shalini Arunogiri, Addiction Psychiatrist, Associate Professor, Monash University; Leigh Walker, , Florey Institute of Neuroscience and Mental Health, and Roberta Anversa, , The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Honey vs Maple Syrup – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing honey to maple syrup, we picked the honey.
Why?
It was very close, as both have small advantages:
• Honey has some medicinal properties (and depending on type, may contain an antihistamine)
• Maple syrup is a good source of manganese, as well as low-but-present amounts of other mineralsHowever, you wouldn’t want to eat enough maple syrup to rely on it as a source of those minerals, and honey has the lower GI (average 46 vs 54; for comparison, refined sugar is 65), which works well as a tie-breaker.
(If GI’s very important to you, though, the easy winner here would be agave syrup if we let it compete, with its GI of 15)
Read more:
• Can Honey Relieve Allergies?
• From Apples to Bees, and High-Fructose C’sShare This Post
-
A Cold Shower A Day Keeps The Doctor Away?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A Cold Shower A Day Keeps The Doctor Away?
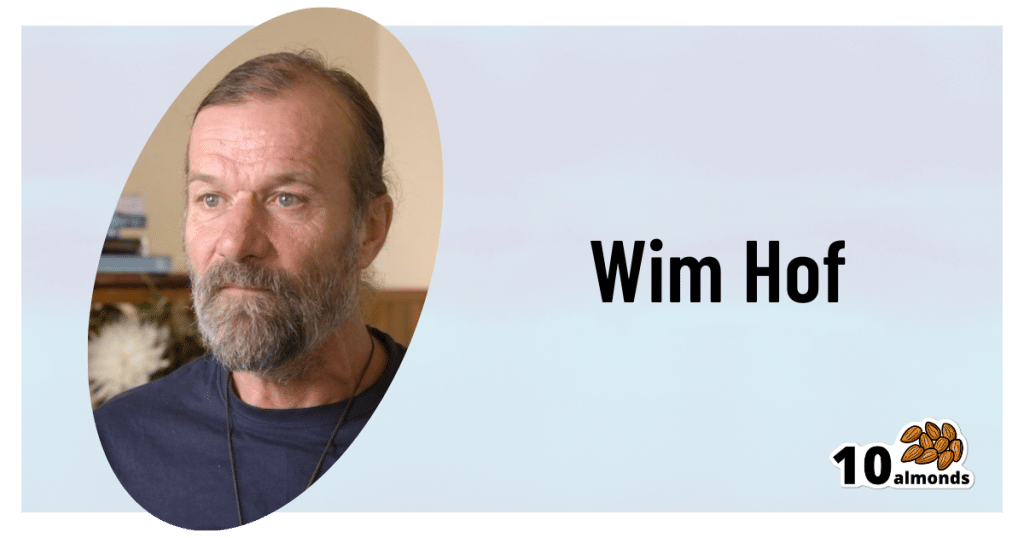
This is Dutch extreme athlete Wim Hof, also known as “The Iceman”! He’s broken many world records mostly relating to the enduring the cold, for example:
- climbing Mount Kilimanjaro in shorts
- running a half-marathon above the Arctic Circle barefoot
- standing in a container completely covered with ice cubes for more than 112 minutes
You might not want to do yoga in your pyjamas on an iceberg, but you might like…
- better circulatory health
- reduced risk of stroke
- a boosted immune system
- healthier skin
- more energy and alertness
…and things like that. Wim Hof’s method is not just about extreme athletic achievements; most of what he does, the stuff that can benefit the rest of us, is much more prosaic.
The Wim Hof Method
For Wim Hof, three things are key:
- Breathing (See: Wim Hof Method Breathing Exercises)
- Commitment (See: How to Increase Willpower)
- Cold therapy (See: Benefits of Cold Therapy)
Today, we’re going to be focusing on the last one there.
What are the benefits of Cold Therapy?
Once upon a time, we didn’t have central heating, electric blankets, thermal underwear, and hot showers. In fact, once upon a time, we didn’t have houses or clothes. We used to be a lot more used to the elements! And while it’s all well and good to enjoy modern comforts, it has left our bodies lacking practice.
Practice at what? Most notably: vasodilation and vasoconstriction, in response to temperature changes. Either:
- vasodilation, because part of our body needs more blood to keep it warm and nourished, or
- vasoconstriction, because part of our body needs less blood running through it to get cooled down.
Switching between the two gives the blood vessels practice at doing it, and improves vascular muscle tone. If your body doesn’t get that practice, your blood vessels will be sluggish at making the change. This can cause circulation problems, which in turn have a big impact in many other areas of health, including:
- cardiovascular disease
- stroke risk
- mood instability
- nerve damage in extremities
On the flipside, if the blood vessels do get regular practice at dilating and constricting, you might enjoy lower risk of those things, and instead:
- improved immune response
- healthier skin
- better quality sleep
- more energy and alertness
- improved sexual performance/responsiveness
So, how to get that, without getting extreme?
As today’s title suggests, “a cold shower a day” is a great practice.
You don’t have to jump straight in, especially if you think your circulation and vascular responses might be a bit sluggish in the first instance. In fact, Wim Hof recommends:
- Week 1: Thirty seconds of cold water at the end of a warm shower each morning
- Week 2: One minute of cold water at the end of a warm shower each morning
- Week 3: A minute and a half of cold water at the end of a warm shower each morning
- Week 4: Two minutes of cold water at the end of a warm shower each morning
How cold is cold?
The benefits of cold exposure begin at around 16ºC / 60ºF, so in most places, water from the cold water mains is sufficiently cold.
As your body becomes more used to making the quick-change on a vascular level, the cold water will seem less shocking to your system. In other words, on day 30 it won’t hit you like it did on day one.
At that point, you can either continue with your two-minutes daily cold shower, and reap the benefits, or if you’re curious to push it further, that’s where ice baths come in!
Can anyone do it, or are any conditions contraindicated?
As ever, we’re a health and productivity newsletter, not doctors, let alone your doctors. Nothing here is medical advice. However, Wim Hof himself says:
❝Listen to your body, and never force the practices. We advise against doing Wim Hof Method if you are dealing with any of the following:
- Epilepsy
- High blood pressure
- Coronary heart disease
- A history of serious healthy issues like heart failure or stroke
- Pregnancy*
- Childhood*❞
*There is simply not enough science regarding the effects of cold exposure on people who are pregnant, or children. Obviously, we don’t expect this to be remedied anytime soon, because the study insitutions’ ethics boards would (rightly!) hold up the study.
As for the other conditions, and just generally if unsure, consult a doctor.
As you can see, this does mean that a limitation of Cold Therapy is that it appears to be far better as a preventative, since it helps guard against the very conditions that could otherwise become contraindications.
We haven’t peppered today’s main feature with study papers, partly because Wim Hof’s own website has kindly collated a collection of them (with links and summaries!) onto one page:
Further reading: The Science Behind The Wim Hof Method
Share This Post
-
Goji Berries: Which Benefits Do They Really Have?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Are Goji Berries Really A Superfood?
Goji berries are popularly considered a superfood, and sold for everything from anti-aging effects, to exciting benefits* that would get this email directed to your spam folder if we described them.
*We searched so you don’t have to: there doesn’t seem to be much research to back [that claim that we can’t mention], but we did find one paper on its “invigorating” benefits for elderly male rats. We prefer to stick to human studies where we can!
So how does the science stack up for the more mainstream claims?
Antioxidant effects
First and most obvious for this fruit that’s full of helpful polysaccharides, carotenoids, phenolic acids, and flavonoids, yes, they really do have strong antioxidant properties:
Immune benefits
Things that are antioxidant are generally also anti-inflammatory, and often have knock-on benefits for the immune system. That appears to be the case here.
For example, in this small-but-statistically-significant study (n=60) in healthy adults (aged 55–72 years)
❝The GoChi group showed a statistically significant increase in the number of lymphocytes and levels of interleukin-2 and immunoglobulin G compared to pre-intervention and the placebo group, whereas the number of CD4, CD8, and natural killer cells or levels of interleukin-4 and immunoglobulin A were not significantly altered. The placebo group showed no significant changes in any immune measures.
Whereas the GoChi group showed a significant increase in general feelings of well-being, such as fatigue and sleep, and showed a tendency for increased short-term memory and focus between pre- and post-intervention, the placebo group showed no significant positive changes in these measures.❞
“GoChi” here is a brand name for goji berries, and it’s not clear from the abstract whether the company funded the study:
Here’s another study, this time n=150, and ages 65–70 years old. This time it’s with a different brand (“Lacto-Wolfberry”, a milk-with-goji supplement drink) and it’s also unclear whether the company funded the study. However, taking the data at face value:
❝In conclusion, long-term dietary supplementation with Lacto-Wolfberry in elderly subjects enhances their capacity to respond to antigenic challenge without overaffecting their immune system, supporting a contribution to reinforcing immune defense in this population. ❞
In other words: it allowed those who took it to get measurably more benefit from the flu vaccinations that they received, without any ill effects.
Anticancer potential
This one’s less contentious (the immune benefits seemed very credible; we’d just like to see more transparent research to say for sure), so in the more clearly-evidenced case against cancer we’ll just drop a few quick studies, clipped for brevity:
- Goji berry (Lycium barbarum) inhibits the proliferation, adhesion, and migration of oral cancer cells
- A closer look at immunomodulatory properties of goji berries extract in human colon cancer cells
- Lycium barbarum polysaccharides induce apoptosis in human prostate cancer cells and inhibits prostate cancer growth
- Identification of goji berry cyclic peptides and anticervical carcinoma activity
- Antiproliferative effects of Lycium barbarum’s (goji berry) fractions on breast cancer Cell Lines
You get the idea: it helps!
Bonus benefit for the eyes
Goji berries also help against age-related macular degeneration. The research for this is in large part secondary, i.e. goji berries contain things x, y, and z, and then separate studies say that those things help against age-related macular degeneration.
We did find some goji-specific studies though! One of them was for our old friends the “Lacto-Wolfberry” people and again, wasn’t very transparent, so we’ll not take up extra time/space with that one here.
Instead, here’s a much clearer, transparent, and well-referenced study with no conflicts of interest, that found:
❝Overall, daily supplementation with Goji berry for 90d improves MPOD by increasing serum Z levels rather than serum L levels in early AMD patients. Goji berry may be an effective therapeutic intervention for preventing the progression of early AMD.❞
- MPOD = Macular Pigment Optical Density, a standard diagnostic tool for age-related macular degeneration
- AMD = Age-related Macular Degeneration
(that whole paper is very compelling reading, if you have time)
If you want a quicker read, we offer:
How To Avoid Age-Related Macular Degeneration
and also…
Where to get goji berries?
You can probably find them at your local health food store, if not the supermarket. However, if you’d like to buy them online, here’s an example product on Amazon for your convenience
Enjoy!
Share This Post
Related Posts
-
The China Study – by Dr. T Colin Campbell and Dr. Thomas M. Campbell
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is not the newest book we’ve reviewed (originally published 2005; this revised and expanded edition 2016), but it is a seminal one.
You’ve probably heard it referenced, and maybe you’ve wondered what the fuss is about. Now you can know!
The titular study itself was huge. We tend to think “oh there was one study” and look to discount it, but it literally looked at the population of China. That’s a large study.
And because China is relatively ethnically homogenous, especially per region, it was easier to isolate what dietary factors made what differences to health. Of course, that did also create a limitation: follow-up studies would be needed to see if the results were the same for non-Chinese people. But even for the rest of us (this reviewer is not Chinese), it already pointed science in the right direction. And sure enough, smaller follow-up studies elsewhere found the same.
But enough about the research; what about the book? This is a book review, not a research review, after all.
The book itself is easy for a lay reader to understand. It explains how the study was conducted (no small feat), and how the data was examined. It also discusses the results, and the conclusions drawn from those results.
In light of all this, it also offers simple actionable advices, on how to eat to avoid disease in general, and cancer in particular. In especially that latter case, one take-home conclusion was: get more of your protein from plants for a big reduction in cancer risk, for example.
Bottom line: this book is an incredible blend of “comprehensive” and “readable” that we don’t often find in the same book! It contains not just a lot of science, but also an insight into how the science works, on a research level. And, of course, its results and conclusions have strong implications for all our lives.
Click here to check out The China Study, to know more about it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Common Hospital Blood Pressure Mistake (Don’t Let This Happen To You Or A Loved One)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There’s a major issue in healthcare, Dr. Suneel Dhand tells us, pertaining to the overtreatment of hypertension in hospitals. Here’s how to watch out for it and know when to question it:
Under pressure
When patients, particularly from older generations, are admitted to the hospital, their blood pressure often fluctuates due to illness, dehydration, and other factors. Despite this, they are often continued on their usual blood pressure medications, which can lead to dangerously low blood pressure.
Why does this happen? The problem arises from rigid protocols that dictate stopping blood pressure medication only if systolic pressure is below a certain threshold, often 100. However, Dr. Dhand argues that 100 is already low*, and administering medication when blood pressure is close to this can cause it to drop dangerously lower
*10almonds note: low for an adult, anyway, and especially for an older adult. To be clear: it’s not a bad thing! That is the average systolic blood pressure of a healthy teenager and it’s usually the opposite of a problem if we have that when older (indeed, this very healthy writer’s blood pressure averages 100/70, and suffice it to say, it’s been a long time since I was a teenager). But it does mean that we definitely don’t want to take medications to artificially lower it from there.
Low blood pressure from overtreatment can lead to severe consequences, requiring emergency interventions to stabilize the patient.
Dr. Dhand’s advice for patients and families is:
- Ensure medication accuracy: make sure the medical team knows the correct blood pressure medications and dosages for you or your loved one.
- Monitor vital signs: actively check blood pressure readings, especially if they are in the low 100s or even 110s, and discuss any medication concerns with the medical team.
- Watch for symptoms of low blood pressure: be alert for symptoms like dizziness or weakness, which could indicate dangerously low blood pressure.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
The Insider’s Guide To Making Hospital As Comfortable As Possible
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Calm Your Mind with Food – by Dr. Uma Naidoo
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
From the author of This Is Your Brain On Food, the psychiatrist-chef (literally, she is a Harvard-trained psychiatrist and an award-winning chef) is back with a more specific work, this time aimed squarely at what it says in the title; how to calm your mind with food.
You may be wondering: does this mean comfort-eating? And, well, not in the sense that term’s usually used. There will be eating and comfort will occur, but the process involves an abundance of nutrients, a minimization of health-deleterious ingredients, and a “for every chemical its task” approach. In other words, very much “nutraceuticals”, as our diet.
On which note: as we’ve come to expect from Dr. Naidoo, we see a lot of hard science presented simply and clearly, with neither undue sensationalization nor unnecessary jargon. We learn about the brain, the gut, relevant biology and chemistry, and build up from understanding ingredients to dietary patterns to having a whole meal plan, complete with recipes.
You may further be wondering: how much does it add that we couldn’t get from the previous book? And the answer is, not necessarily a huge amount, especially if you’re fairly comfortable taking ideas and creating your own path forwards using them. If, on the other hand, you’re a little anxious about doing that (as someone perusing this book may well be), then Dr. Naidoo will cheerfully lead you by the hand through what you need to know and do.
Bottom line: if not being compared to her previous book, this is a great standalone book with a lot of very valuable content. However, the previous book is a tough act to follow! So… All in all we’d recommend this more to people who want to indeed “calm your mind with food”, who haven’t read the other book, as this one will be more specialized for you.
Click here to check out Calm Your Mind With Food, and do just that!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: