New California Laws Target Medical Debt, AI Care Decisions, Detention Centers
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
SACRAMENTO, Calif. — As the nation braces for potential policy shifts under President-elect Donald Trump’s “Make America Healthy Again” mantra, the nation’s most populous state and largest health care market is preparing for a few changes of its own.
With supermajorities in both houses, Democrats in the California Legislature passed — and Democratic Gov. Gavin Newsom signed — laws taking effect this year that will erase medical debt from credit reports, allow public health officials to inspect immigrant detention centers, and require health insurance companies to cover fertility services such as in vitro fertilization.
Still, industry experts say it was a relatively quiet year for health policy in the Golden State, with more attention on a divisive presidential election and with several state legislators seeking to avoid controversial issues as they ran for Congress in competitive swing districts.
Newsom shot down some of legislators’ most ambitious health care policies, including proposals that would have regulated pharmaceutical industry middlemen and given the state more power to stop private equity deals in health care.
Health policy experts say advocates and legislators are now focused on how to defend progressive California policies such as sweeping abortion access in the state and health coverage for immigrants living in the U.S. without authorization.
“I think everyone’s just thinking about how we’re going to enter 2025,” said Rachel Linn Gish, a spokesperson with the consumer health advocacy group Health Access California. “We’re figuring out what is vulnerable, what we are exposed to on the federal side, and what do budget changes mean for our work. That’s kind of putting a cloud over everything.”
Here are some of the biggest new health care laws Californians should know about:
Medical debt
California becomes the eighth state in which medical debt will no longer affect patients’ credit reports or credit scores. SB 1061 bars health care providers and debt collectors from reporting unpaid medical bills to credit bureaus, a practice that supporters of the law say penalizes people for seeking critical care and can make it harder for patients to get a job, buy a car, or secure a mortgage.
Critics including the California Association of Collectors called the measure from Sen. Monique Limón (D-Santa Barbara) a “tremendous overreach” and successfully lobbied for amendments that limited the scope of the bill, including an exemption for any medical debt incurred on credit cards.
The Biden administration has finalized federal rules that would stop unpaid medical bills from affecting patients’ credit scores, but the fate of those changes remains unclear as Trump takes office.
Psychiatric hospital stays for violent offenders
Violent offenders with severe mental illness can now be held longer after a judge orders them released from a state mental hospital.
State officials and local law enforcement will now have 30 days to coordinate housing, medication, and behavioral health treatment for those parolees, giving them far more time than the five-day deadline previously in effect.
The bill drew overwhelming bipartisan support after a high-profile case in San Francisco in which a 61-year-old man was charged in the repeated stabbing of a bakery employee just days after his release from a state mental hospital. The bill’s author, Assembly member Matt Haney (D-San Francisco), called the previous five-day timeline “dangerously short.”
Cosmetics and ‘forever chemicals’
California was the first state to ban PFAS chemicals, also known as “forever chemicals,” in all cosmetics sold and manufactured within its borders. The synthetic compounds, found in everyday products including rain jackets, food packaging, lipstick, and shaving cream, have been linked to cancer, birth defects, and diminished immune function and have been increasingly detected in drinking water.
Industry representatives have argued that use of PFAS — perfluoroalkyl and polyfluoroalkyl substances — is critical in some products and that some can be safely used at certain levels.
Immigration detention facilities
After covid-19 outbreaks, contaminated water, and moldy food became the subjects of detainee complaints and lawsuits, state legislators gave local county health officials the authority to enter and inspect privately run immigrant detention centers. SB 1132, from Sen. María Elena Durazo (D-Los Angeles), gives public health officials the ability to evaluate whether privately run facilities are complying with state and local public health regulations regarding proper ventilation, basic mental and physical health care, and food safety.
Although the federal government regulates immigration, six federal detention centers in California are operated by the GEO Group. One of the country’s largest private prison contractors, GEO has faced a litany of complaints related to health and safety. Unlike public prisons and jails, which are inspected annually, these facilities would be inspected only as deemed necessary.
The contractor filed suit in October to stop implementation of the law, saying it unconstitutionally oversteps the federal government’s authority to regulate immigration detention centers. A hearing in the case is set for March 3, said Bethany Lesser, a spokesperson for California Attorney General Rob Bonta. The law took effect Jan. 1.
Doctors vs. insurance companies using AI
As major insurance companies increasingly use artificial intelligence as a tool to analyze patient claims and authorize some treatment, trade groups representing doctors are concerned that AI algorithms are driving an increase in denials for necessary care. Legislators unanimously agreed.
SB 1120 states that decisions about whether a treatment is medically necessary can be made only by licensed, qualified physicians or other health care providers who review a patient’s medical history and other records.
Sick leave and protected time off
Two new laws expand the circumstances under which California workers may use sick days and other leave. SB 1105 entitles farmworkers who work outdoors to take paid sick leave to avoid heat, smoke, or flooding when local or state officials declare an emergency.
AB 2499 expands the list of reasons employees may take paid sick days or use protected unpaid leave to include assisting a family member who is experiencing domestic violence or other violent crimes.
Prescription labels for the visually impaired
Starting this year, pharmacies will be required to provide drug labels and use instructions in Braille, large print, or audio for blind patients.
Advocates of the move said state law, which already required translated instructions in five languages for non-English speakers, has overlooked blind patients, making it difficult for them to monitor prescriptions and take the correct dosage.
Maternal mental health screenings
Health insurers will be required to bolster maternal mental health programs by mandating additional screenings to better detect perinatal depression, which affects 1 in 5 people who give birth in California, according to state data. Pregnant people will now undergo screenings at least once during pregnancy and then six weeks postpartum, with further screenings as providers deem necessary.
Penalties for threatening health care workers (abortion clinics)
With abortion care at the center of national policy fights, California is cracking down on those who threaten, post personal information about, or otherwise target providers or patients at clinics that perform abortions. Penalties for such behavior will increase under AB 2099, and offenders can face felony charges, up to three years in jail, and $50,000 in fines for repeat or violent offenses. Previously, state law classified many of those offenses as misdemeanors.
Insurance coverage for IVF
Starting in July, state-regulated health plans covering 50 employees or more would be required to cover fertility services under SB 729, passed and signed last year. Advocates have long fought for this benefit, which they say is essential care for many families who have trouble getting pregnant and would ensure LGBTQ+ couples aren’t required to pay more out-of-pocket costs than straight couples when starting a family.
In a signing statement, Newsom asked legislators to delay implementation of the law until 2026 as state officials consider whether to add infertility treatments to the list of benefits that insurance plans are required to cover.
It’s unclear whether legislators intend to address that this session, but a spokesperson for the governor said that Newsom “clearly stated his position on the need for an extension” and that he “will continue to work with the legislature” on the matter.
Plans under CalPERS, the California Public Employees’ Retirement System, would have to comply by July 2027.
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What’s in the supplements that claim to help you cut down on bathroom breaks? And do they work?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
With one in four Australian adults experiencing problems with incontinence, some people look to supplements for relief.
With ingredients such as pumpkin seed oil and soybean extract, a range of products promise relief from frequent bathroom trips.
But do they really work? Let’s sift through the claims and see what the science says about their efficacy.
Christian Moro/Shutterstock What is incontinence?
Incontinence is the involuntary loss of bladder or bowel control, leading to the unintentional leakage of urine or faeces. It can range from occasional minor leaks to a complete inability to control urination and defecation.
This condition can significantly impact daily activities and quality of life, and affects women more often than it affects men.
Some people don’t experience bladder leakage but can sometimes feel an urgent need to go to the bathroom. This is known as overactive bladder syndrome, and occurs when the muscles around the bladder tighten on their own, which greatly reduces its capacity. The result is the person feels the need to go to the bathroom much more frequently.
There are many potential causes of incontinence and overactive bladders, including menopause, pregnancy and child birth, urinary tract infections, pelvic floor disorders, and an enlarged prostate. Conditions such as diabetes, neurological disorders and certain medications (such as diuretics, sleeping pills, antidepressants and blood-pressure drugs) can also contribute.
While pelvic muscle rehabilitation and behavioural techniques for bladder retraining can be helpful, some people are interested in pharmaceutical solutions.
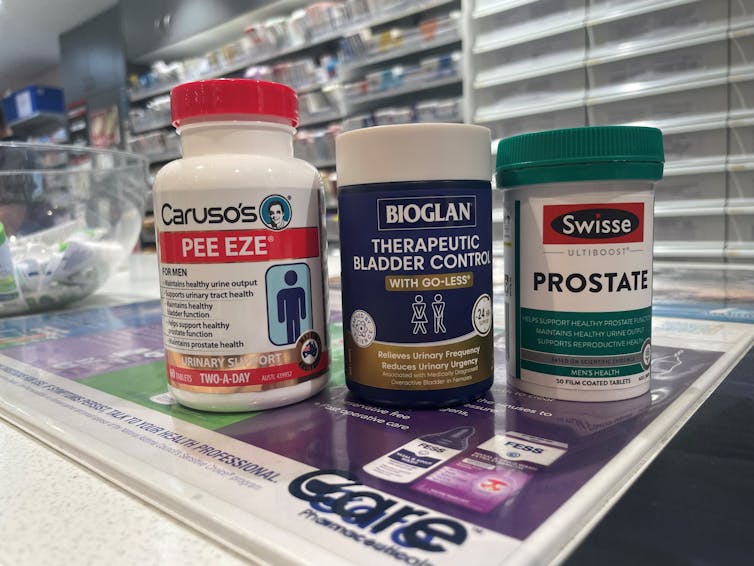
What’s in these products?
A number of supplements are available in Australia that include ingredients used in traditional medicine for urinary incontinence and overactive bladders. The three most common ingredients are:
- Cucurbita pepo (pumpkin seed extract)
- glycine max (soybean extract)
- an extract from the bark of the Crateva magna or nurvala (Varuna) tree.
The supplements have common ingredients. Author How are they supposed to work?
Pumpkin seeds are rich in plant sterols that are thought to reduce the testosterone-related enlargement of the prostate, as well as having broader anti-inflammatory effects. The seed extracts can also contain oleic acid, which may help increase bladder capacity by relaxing the muscles around the organ.
Soybean extracts are rich in isoflavones, especially daidzen and genistein. Like olieic acid, these are thought to act on the muscles around the bladder. Because isoflavones are similar in structure to the female hormone oestrogen, soy extracts may be most beneficial for postmenopausal women who have overactive bladders.
Crateva extract is rich in lupeol- and sterol-based chemicals which have strong anti-inflammatory effects. This has benefits not just for enlarged prostates but possibly also for reducing urinary tract infections.
Do they actually work?
It’s important to note that the government has only approved these types of supplements as “listed medicines”. This means the ingredients have only been assessed for safety. The companies behind the products have not had to provide evidence they actually work.
A 2014 clinical trial examined a combined pumpkin seed and soybean extract called cucurflavone on people with overactive bladders. The 120 participants received either a placebo or a daily 1,000mg dose of the herbal mixture over a period of 12 weeks.
By the end of study, those in the cucurflavone group went to the bathroom around three fewer times per day, compared with people in the control group, who only went to the bathroom on average one fewer time each day.
In a different trial, researchers examined a combination of Crateva bark extract with herbal extracts of horsetail and Japanese evergreen spicebush, called Urox.
For the 150 participants, the Urox formulation helped participants go to the bathroom less frequently when compared with placebo treatment.
After eight weeks of treatment, participants in the placebo group were going to the bathroom to urinate 11 times per day. Those in the Urox group were only going around to 7.5 times per day. And those who took Urox also needed to go to the bathroom one fewer time during the night.
Finally, another study also examined a Creteva, horsetail and Japanese spicebush combination, but this time in children. They were given either a 420mg dose of the supplement or a placebo, and then monitored for how many times they wet the bed.
After two months of taking the supplement, slightly more than 40% of the 24 kids in the supplement group wet the bed less often.
While these results may look promising, there are considerable limitations to the studies which means the data may not be reliable. For example, the trials didn’t include enough participants to have reliable data. To conclusively provide efficacy, final-stage clinical trials require data for between 300 and 3,000 patients.
From the studies, it is also not clear whether some participants were also taking other medicines as well as the supplement. This is important, as medications can interfere with how the supplements work, potentially making them less or more effective.
What if you want to take them?
If you have incontinence or an overactive bladder, you should always discuss this with your doctor, as it may due to a serious or treatable underlying condition.
Otherwise, your GP may give you strategies or exercises to improve your bladder control, prescribe medications or devices, or refer you to a specialist.
If you do decide to take a supplement, discuss this with your doctor and local pharmacist so they can check that any product you choose will not interfere with any other medications you may be taking.
Nial Wheate, Professor of Pharmaceutical Chemistry, Macquarie University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Hungry? How To Beat Cravings
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Science of Hunger, And How To Sate It
This is Dr. David Ludwig. That’s not a typo; he’s a doctor both ways—MD and PhD.
Henceforth we’ll just say “Dr. Ludwig”, though! He’s a professor in the Department of Nutrition at Harvard T.H. Chan School of Public Health, and director of the New Balance Foundation Obesity Prevention Center.
His research focuses on the effects of diet on hormones, metabolism, and body weight, and he’s one of the foremost experts when it comes to carbohydrates, glycemic load, and obesity.
Why are we putting on weight? What are we getting wrong?
Contrary to popular belief, Dr. Ludwig says, weight gain is not caused by a lack of exercise. In fact, people tend to overestimate how many calories are burned by exercise.
A spoonful of sugar may make the medicine go down, but it also contains 60 calories, and that’d take about 1,500 steps for the average person to burn off. Let’s put this another way:
If you walk 10,000 steps per day, that will burn off 400 calories. Still think you can exercise away that ice cream sundae or plate of fries?
Wait, this is interesting and all, but what does this have to do with hunger?
Why we get hungry
Two important things:
- All that exercise makes us hungry, because the more we exercise, the more the body speeds up our metabolism accordingly.
- Empty calories don’t just add weight themselves, they also make us hungrier
What are empty calories, and why do they make us hungrier?
Empty calories are calories that are relatively devoid of other nutrition. This especially means simple sugars (especially refined sugar), white flour and white flour products (quick-release starches), and processed seed oils (e.g. canola, sunflower, and friends).
They zip straight into our bloodstream, and our body sends out an army of insulin to deal with the blood sugar spike. And… that backfires.
Imagine a person whose house is a terrible mess, and they have a date coming over in half an hour.
They’re going to zoom around tidying, but they’re going to stuff things out of sight as quickly and easily as possible, rather than, say, sit down and Marie Kondo the place.
But superficially, they got the job done really quickly!
Insulin does similarly when overwhelmed by a blood sugar spike like that.
So, it stores everything as fat as quickly as possible, and whew, the pancreas needs a break now after all that exertion, and the blood is nice and free from blood sugars.
Wait, the blood is what now?
The body notices the low blood sugar levels, and it also knows you just stored fat so you must be preparing for starvation, and now the low blood sugar levels indicate starvation is upon us. Quick, we must find food if we want to survive! So it sends a hunger signal to make sure you don’t let the body starve.
You make a quick snack, and the cycle repeats.
Dr. Ludwig’s solution:
First, we need to break out of that cycle, and that includes calming down our insulin response (and thus rebuilding our insulin sensitivity, as our bodies will have become desensitized, after the equivalent of an air-raid siren every 40 minutes or so).
How to do that?
First, cut out the really bad things that we mentioned above.
Next: cut healthy carbs too—we’re talking unprocessed grains here, legumes as well, and also starchy vegetables (root vegetables etc). Don’t worry, this will be just for a short while.
The trick here is that we are resensitizing our bodies to insulin.
Keep this up for even just a week, and then gradually reintroduce the healthier carbs. Unprocessed grains are better than root vegetables, as are legumes.
You’re not going to reintroduce the sugars, white flour, canola oil, etc. You don’t have to be a puritan, and if you go to a restaurant you won’t undo all your work if you have a small portion of fries. But it’s not going to be a part of your general diet.
Other tips from Dr. Ludwig:
- Get plenty of high-quality protein—it’s good for you and suppresses your appetite
- Shop for success—make sure you keep your kitchen stocked with healthy easy snack food
- Nuts, cacao nibs, and healthy seeds will be your best friends and allies here
- Make things easy—buy pre-chopped vegetables, for example, so when you’re hungry, you don’t have to wait longer (and work more) to eat something healthy
- Do what you can to reduce stress, and also eat mindfully (that means paying attention to each mouthful, rather than wolfing something down while multitasking)
If you’d like to know more about Dr. Ludwig and his work, you can check out his website for coaching, recipes, meal plans, his blog, and other resources!
Share This Post
-
Leek vs Scallions – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing leek to scallions, we picked the leek.
Why?
In terms of macros, scallions might have a point: scallions have the lower glycemic index, thanks to leek having more carbs for the same amount of fiber. That said, leek already has a low glycemic index, so this is not a big deal.
When it comes to vitamins, leek has more of vitamins B1, B2, B3, B5, B6, B9, E, and choline, while scallions have more of vitamins A, C, and K. Noteworthily, a cup of chopped leek already provides the daily dose of vitamins A and K, and the difference in levels of vitamin C is minimal. All in all, an easy 8:3 win for leeks here, even without taking that into account.
In the category of minerals, leek has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, and selenium, while scallions have a little more zinc.
Both of these allium-family plants (i.e., related to garlic) have an abundance of polyphenols, especially kaempferol.
Of course, enjoy whatever goes best with your meal, but if you’re looking for nutritional density, then leek is where it’s at.
Want to learn more?
You might like to read:
The Many Health Benefits Of Garlic
Take care!
Share This Post
Related Posts
-
How Much Weight Gain Do Antidepressants Cause?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There’s a lot of talk in the news lately about antidepressants and weight gain, so let’s look at some numbers.
Here’s a study from July 2024 that compared the weight gain of eight popular antidepressants, and pop-science outlets have reported it with such snippets as:
❝Bupropion users were approximately 15–20% less likely to gain a clinically significant amount of weight than those taking the most common medication, sertraline.
The researchers considered weight gain of 5% or more as clinically significant.❞
Read in full: Study compares weight gain across eight common antidepressants
At this point, you might (especially if you or a loved one is on sertraline) be grabbing a calculator and seeing what 5% of your weight is, and might be concerned at the implications.
However, this is a little like if, in our This or That section, we were to report that food A has 17x more potassium than food B, without mentioning that food A has 0.01mg/100g and food A has 0.17mg/100g, and thus that, while technically “17x more”, the difference is trivial.
As a quick aside: we do, by the way, try to note when things like that might skew the stats and either wipe them out by not mentioning that they contain potassium at all (as they barely do), or if it’s a bit more, describing them as being “approximately equal in potassium” or else draw attention to the “but the amounts are trivial in both cases”.
Back to the antidepressants: in fact, for those two antidepressants compared in that snippet, the truth is (when we go looking in the actual research paper and the data within):
- sertraline was associated with an average weight change of +1.5kg (just over 3lb) over the course of 24 months
- bupropion was associated with an average weight change of +0.5kg (just under 1lb) over the course of 24 months
Sertraline being the most weight-gain-inducing of the 8 drugs compared, and bupropion being the least, this means (with them both having fairly even curves):
- sertraline being associated with an average weight change of 0.06kg (about 2oz) per month
- bupropion being associated with an average weight change of 0.02kg (less than 1oz) per month
For all eight, see the chart here in the paper itself:
Medication-Induced Weight Change Across Common Antidepressant Treatments ← we’ve made the link go straight to the chart, for your convenience, but you can also read the whole paper there
While you’re there, you might also see that for some antidepressants, such as duloxetine, fluoxetine, and venlafaxine, there’s an initial weight gain, but then it clearly hits a plateau and weight ceases to change after a certain point, which is worth considering too, since “you’ll gain a little bit of weight and then stay at that weight” is a very different prognosis from “you’ll gain a bit of weight and keep gaining it forever until you die”.
But then again, consider this:
Most adults will gain half a kilo this year – and every year. Here’s how to stop “weight creep”
That’s more weight gain than one gets on sertraline, the most weight-gain-inducing antidepressant tested!
What about over longer-term use?
Here’s a more recent study (December 2024) that looked at antidepressant use over 6 years, and found an average 2% weight gain over those 6 years, but it didn’t break it down by antidepressant type, sadly:
…which seems like quite a wasted opportunity, since some of the medications considered are very different, working on completely different systems (for example, SSRIs vs NDRIs, working on serotonin or norepinephrine+dopamine, respectively—see our Neurotransmitter Cheatsheet for more about those) and having often quite different side effects. Nevertheless, the study (despite collecting this information) didn’t then tabulate the data, and instead considered them all to be the same factor, “antidepressants”.
What this study did do that was useful was included a control group not on antidepressants so we know that on average:
- never-users of antidepressants gained an average of 1% of their bodyweight over those 6 years
- users-and-desisters of antidepressants gained an average of 1.8% of their bodyweight over those 6 years*
- continuing users of antidepressants gained an average of 2% of their bodyweight over those 6 years
*for this group, weight gain was a commonly cited reason for stopping taking the antidepressants in question
Writer’s anecdote: I’ve been on mirtazapine (a presynaptic alpha2-adrenoreceptor antagonist which increases central noradrenergic and serotonergic neurotransmission) for some years and can only say that I wish I’d been on it decades previously. I requested mirtazapine specifically, because I’m me and I know my stuff and considered it would most likely be by far the best fit for me out of the options available. Starting at a low dose, the only meaningful side effect was mild sedation (expected, and associated only with low-dose use); increasing after a couple of weeks to a moderate dose, that side effect disappeared and now the only remaining side effect is a slight dryness of the mouth, which is fine, as it ensures I remember to stay hydrated 🙂 anyway, my weight hasn’t changed (beyond very small temporary fluctuations) in the time I’ve been on mirtazapine. Disclaimer: the plural of anecdote is not data, and I can only speak for my own experience, and am not making any particular recommendation here. Your personal physiology will be different from mine, and may respond well or badly to any given treatment according to your own physiology.
Further considerations
This is touched on in the “Discussion” section of the latter paper (so do check that out if you want all the details, more than we can reasonably put here), but there are other factors to consider, for example:
- whether people were underweight/healthy weight/overweight at baseline (sometimes, a weight gain can be a good thing, recovering from an illness, and in the case of the illness that is depression, weight can swing either way)
- antidepressants changing eating and exercise habits (generally speaking: more likely to eat more and exercise more)
- body composition! How did they not cover this (neither paper did)?! Muscle weighs more than fat, and improvements in exercise can result in an increase in muscle and thus an increase in overall weight.
As researchers like to say, “this highlights the need for more high-quality studies to look into…” (and then the various things that went unexamined).
Want to know more?
Check out our previous main feature:
Antidepressants: Personalization Is Key!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Sesame Chocolate Fudge
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you’d like a sweet treat without skyrocketing your blood sugars with, well, rocket fuel… Today’s recipe can help you enjoy a taste of decadence that’s not bad for your blood sugars, and good for your heart and brain.
You will need
- ½ cup sesame seeds
- ¼ cup cocoa powder
- 3 tbsp maple syrup
- 1 tbsp coconut oil (plus a little extra for the pan)
Method
(we suggest you read everything at least once before doing anything)
1) Lightly toast the sesame seeds in a pan until golden brown. Remove from the heat and allow to cool.
2) Put them in a food processor, and blend on full speed until they start to form a dough-like mixture. This may take a few minutes, so be patient. We recommend doing it in 30-second sessions with a 30-second rest between them, to avoiding overheating the motor.
3) Add the rest of the ingredients and blend to combine thoroughly—this should go easily now and only take 10 seconds or so, but judge it by eye.
4) Grease an 8″ square baking tin with a little coconut oil, and add the mixture, patting it down to fill the tin, making sure it is well-compressed.
5) Allow to chill in the fridge for 6 hours, until firm.
6) Turn the fudge out onto a chopping board, and cut into the size squares you want. Serve, or store in the fridge until ready to serve.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Tasty Polyphenols For Your Heart & Brain
- Cacao vs Carob – Which is Healthier?
- Can Saturated Fats Be Healthy?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Night School – by Dr. Richard Wiseman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sleep is a largely neglected part of health for most people. Compared to factors like food and exercise, it’s something that experientially we’re mostly not present for! Little wonder then that we also often feel like it’s outside of our control.
While Dr. Wiseman does cover the usual advices with regard to getting good sleep, this book has a lot more than that.
Assuming that they go beyond the above, resources about sleep can usually be divided into one of two categories:
- Hard science: lots about brainwaves, sleep phases, circadian rhythms, melatonin production, etc… But nothing very inspiring!
- Fantastical whimsy: lots about dreams, spiritualism, and not a scientific source to be found… Nothing very concrete!
This book does better.
We get the science and the wonder. When it comes to lucid dreaming, sleep-learning, sleep hypnosis, or a miraculously reduced need for sleep, everything comes with copious scientific sources or not at all. Dr. Wiseman is well-known in his field for brining scientific skepticism to paranormal claims, by the way—so it’s nice to read how he can do this without losing his sense of wonder. Think of him as the Carl Sagan of sleep, perhaps.
Style-wise, the book is pop-science and easy-reading. Unsurprising, for a professional public educator and science-popularizer.
Structurally, the main part of the book is divided into lessons. Each of these come with background science and principles first, then a problem that we might want to solve, then exercises to do, to get the thing we want. It’s at once a textbook and an instruction manual.
Bottom line: this is a very inspiring book with a lot of science. Whether you’re looking to measurably boost your working memory or heal trauma through dreams, this book has everything.
Click here to check out Night School and learn what your brain can do!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: