California Becomes Latest State To Try Capping Health Care Spending
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
California’s Office of Health Care Affordability faces a herculean task in its plan to slow runaway health care spending.
The goal of the agency, established in 2022, is to make care more affordable and accessible while improving health outcomes, especially for the most disadvantaged state residents. That will require a sustained wrestling match with a sprawling, often dysfunctional health system and powerful industry players who have lots of experience fighting one another and the state.
Can the new agency get insurers, hospitals, and medical groups to collaborate on containing costs even as they jockey for position in the state’s $405 billion health care economy? Can the system be transformed so that financial rewards are tied more to providing quality care than to charging, often exorbitantly, for a seemingly limitless number of services and procedures?
The jury is out, and it could be for many years.
California is the ninth state — after Connecticut, Delaware, Massachusetts, Nevada, New Jersey, Oregon, Rhode Island, and Washington — to set annual health spending targets.
Massachusetts, which started annual spending targets in 2013, was the first state to do so. It’s the only one old enough to have a substantial pre-pandemic track record, and its results are mixed: The annual health spending increases were below the target in three of the first five years and dropped beneath the national average. But more recently, health spending has greatly increased.
In 2022, growth in health care expenditures exceeded Massachusetts’ target by a wide margin. The Health Policy Commission, the state agency established to oversee the spending control efforts, warned that “there are many alarming trends which, if unaddressed, will result in a health care system that is unaffordable.”
Neighboring Rhode Island, despite a preexisting policy of limiting hospital price increases, exceeded its overall health care spending growth target in 2019, the year it took effect. In 2020 and 2021, spending was largely skewed by the pandemic. In 2022, the spending increase came in at half the state’s target rate. Connecticut and Delaware, by contrast, both overshot their 2022 targets.
It’s all a work in progress, and California’s agency will, to some extent, be playing it by ear in the face of state policies and demographic realities that require more spending on health care.
And it will inevitably face pushback from the industry as it confronts unreasonably high prices, unnecessary medical treatments, overuse of high-cost care, administrative waste, and the inflationary concentration of a growing number of hospitals in a small number of hands.
“If you’re telling an industry we need to slow down spending growth, you’re telling them we need to slow down your revenue growth,” says Michael Bailit, president of Bailit Health, a Massachusetts-based consulting group, who has consulted for various states, including California. “And maybe that’s going to be heard as ‘we have to restrain your margins.’ These are very difficult conversations.”
Some of California’s most significant health care sectors have voiced disagreement with the fledgling affordability agency, even as they avoid overtly opposing its goals.
In April, when the affordability office was considering an annual per capita spending growth target of 3%, the California Hospital Association sent it a letter saying hospitals “stand ready to work with” the agency. But the proposed number was far too low, the association argued, because it failed to account for California’s aging population, new investments in Medi-Cal, and other cost pressures.
The hospital group suggested a spending increase target averaging 5.3% over five years, 2025-29. That’s slightly higher than the 5.2% average annual increase in per capita health spending over the five years from 2015 to 2020.
Five days after the hospital association sent its letter, the affordability board approved a slightly less aggressive target that starts at 3.5% in 2025 and drops to 3% by 2029. Carmela Coyle, the association’s chief executive, said in a statement that the board’s decision still failed to account for an aging population, the growing need for mental health and addiction treatment, and a labor shortage.
The California Medical Association, which represents the state’s doctors, expressed similar concerns. The new phased-in target, it said, was “less unreasonable” than the original plan, but the group would “continue to advocate against an artificially low spending target that will have real-life negative impacts on patient access and quality of care.”
But let’s give the state some credit here. The mission on which it is embarking is very ambitious, and it’s hard to argue with the motivation behind it: to interject some financial reason and provide relief for millions of Californians who forgo needed medical care or nix other important household expenses to afford it.
Sushmita Morris, a 38-year-old Pasadena resident, was shocked by a bill she received for an outpatient procedure last July at the University of Southern California’s Keck Hospital, following a miscarriage. The procedure lasted all of 30 minutes, Morris says, and when she received a bill from the doctor for slightly over $700, she paid it. But then a bill from the hospital arrived, totaling nearly $9,000, and her share was over $4,600.
Morris called the Keck billing office multiple times asking for an itemization of the charges but got nowhere. “I got a robotic answer, ‘You have a high-deductible plan,’” she says. “But I should still receive a bill within reason for what was done.” She has refused to pay that bill and expects to hear soon from a collection agency.
The road to more affordable health care will be long and chock-full of big challenges and unforeseen events that could alter the landscape and require considerable flexibility.
Some flexibility is built in. For one thing, the state cap on spending increases may not apply to health care institutions, industry segments, or geographic regions that can show their circumstances justify higher spending — for example, older, sicker patients or sharp increases in the cost of labor.
For those that exceed the limit without such justification, the first step will be a performance improvement plan. If that doesn’t work, at some point — yet to be determined — the affordability office can levy financial penalties up to the full amount by which an organization exceeds the target. But that is unlikely to happen until at least 2030, given the time lag of data collection, followed by conversations with those who exceed the target, and potential improvement plans.
In California, officials, consumer advocates, and health care experts say engagement among all the players, informed by robust and institution-specific data on cost trends, will yield greater transparency and, ultimately, accountability.
Richard Kronick, a public health professor at the University of California-San Diego and a member of the affordability board, notes there is scant public data about cost trends at specific health care institutions. However, “we will know that in the future,” he says, “and I think that knowing it and having that information in the public will put some pressure on those organizations.”
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
When Carbs, Proteins, & Fats Switch Metabolic Roles
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Strange Things Happening In The Islets Of Langerhans
It is generally known and widely accepted that carbs have the biggest effect on blood sugar levels (and thus insulin response), fats less so, and protein least of all.
And yet, there was a groundbreaking study published yesterday which found:
❝Glucose is the well-known driver of insulin, but we were surprised to see such high variability, with some individuals showing a strong response to proteins, and others to fats, which had never been characterized before.
Insulin plays a major role in human health, in everything from diabetes, where it is too low*, to obesity, weight gain and even some forms of cancer, where it is too high.
These findings lay the groundwork for personalized nutrition that could transform how we treat and manage a range of conditions.❞
*saying ”too low” here is potentially misleading without clarification; yes, Type 1 Diabetics will have too little [endogenous] insulin (because the pancreas is at war with itself and thus isn’t producing useful quantities of insulin, if any). Type 2, however, is more a case of acquired insulin insensitivity, because of having too much at once too often, thus the body stops listening to it, “boy who cried wolf”-style, and the pancreas also starts to get fatigued from producing so much insulin that’s often getting ignored, and does eventually produce less and less while needing more and more insulin to get the same response, so it can be legitimately said “there’s not enough”, but that’s more of a subjective outcome than an objective cause.
Back to the study itself, though…
What they found, and how they found it
Researchers took pancreatic islets from 140 heterogenous donors (varied in age and sex; ostensibly mostly non-diabetic donors, but they acknowledge type 2 diabetes could potentially have gone undiagnosed in some donors*) and tested cell cultures from each with various carbs, proteins, and fats.
They found the expected results in most of the cases, but around 9% responded more strongly to the fats than the carbs (even more strongly than to glucose specifically), and even more surprisingly 8% responded more strongly to the proteins.
*there were also some known type 2 diabetics amongst the donors; as expected, those had a poor insulin response to glucose, but their insulin response to proteins and fats were largely unaffected.
What this means
While this is, in essence, a pilot study (the researchers called for larger and more varied studies, as well as in vivo human studies), the implications so far are important:
It appears that, for a minority of people, a lot of (generally considered very good) antidiabetic advice may not be working in the way previously understood. They’re going to (for example) put fat on their carbs to reduce the blood sugar spike, which will technically still work, but the insulin response is going to be briefly spiked anyway, because of the fats, which very insulin response is what will lower the blood sugars.
In practical terms, there’s not a lot we can do about this at home just yet—even continuous glucose monitors won’t tell us precisely, because they’re monitoring glucose, not the insulin response. We could probably measure everything and do some math and work out what our insulin response has been like based on the pace of change in blood sugar levels (which won’t decrease without insulin to allow such), but even that is at best grounds for a hypothesis for now.
Hopefully, more publicly-available tests will be developed soon, enabling us all to know our “insulin response type” per the proteome predictors discovered in this study, rather than having to just blindly bet on it being “normal”.
Ironically, this very response may have hidden itself for a while—if taking fats raised insulin response without raising blood sugar levels, then if blood sugar levels are the only thing being measured, all we’ll see is “took fats at dinner; blood sugars returned to normal more quickly than when taking carbs without fats”.
You can read the study in full here:
Proteomic predictors of individualized nutrient-specific insulin secretion in health and disease
Want to know more about blood sugar management?
You might like to catch up on:
- 10 Ways To Balance Your Blood Sugars
- Track Your Blood Sugars For Better Personalized Health
- How To Turn Back The Clock On Insulin Resistance
Take care!
Share This Post
-
Only walking for exercise? Here’s how to get the most out of it
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’re living longer than in previous generations, with one in eight elderly Australians now aged over 85. But the current gap between life expectancy (“lifespan”) and health-adjusted life expectancy (“healthspan”) is about ten years. This means many of us live with significant health problems in our later years.
To increase our healthspan, we need planned, structured and regular physical activity (or exercise). The World Health Organization recommends 150–300 minutes of moderate-intensity exercise – such as brisk walking, cycling and swimming – per week and muscle strengthening twice a week.
Yet few of us meet these recommendations. Only 10% meet the strength-training recommendations. Lack of time is one of the most common reasons.
Walking is cost-effective, doesn’t require any special equipment or training, and can be done with small pockets of time. Our preliminary research, published this week, shows there are ways to incorporate strength-training components into walking to improve your muscle strength and balance.
Why walking isn’t usually enough
Regular walking does not appear to work as muscle-strengthening exercise.
In contrast, exercises consisting of “eccentric” or muscle-lengthening contractions improve muscle strength, prevent muscle wasting and improve other functions such as balance and flexibility.
Typical eccentric contractions are seen, for example, when we sit on a chair slowly. The front thigh muscles lengthen with force generation.
When you sit down slowly on a chair, the front thigh muscles lengthen.
buritora/ShutterstockOur research
Our previous research found body-weight-based eccentric exercise training, such as sitting down on a chair slowly, improved lower limb muscle strength and balance in healthy older adults.
We also showed walking down stairs, with the front thigh muscles undergoing eccentric contractions, increased leg muscle strength and balance in older women more than walking up stairs. When climbing stairs, the front thigh muscles undergo “concentric” contractions, with the muscles shortening.
It can be difficult to find stairs or slopes suitable for eccentric exercises. But if they could be incorporated into daily walking, lower limb muscle strength and balance function could be improved.
This is where the idea of “eccentric walking” comes into play. This means inserting lunges in conventional walking, in addition to downstairs and downhill walking.
In our new research, published in the European Journal of Applied Physiology, we investigated the effects of eccentric walking on lower limb muscle strength and balance in 11 regular walkers aged 54 to 88 years.
The intervention period was 12 weeks. It consisted of four weeks of normal walking followed by eight weeks of eccentric walking.
The number of eccentric steps in the eccentric walking period gradually increased over eight weeks from 100 to 1,000 steps (including lunges, downhill and downstairs steps). Participants took a total of 3,900 eccentric steps over the eight-week eccentric walking period while the total number of steps was the same as the previous four weeks.
We measured the thickness of the participants’ front thigh muscles, muscle strength in their knee, their balance and endurance, including how many times they could go from a sitting position to standing in 30 seconds without using their arms. We took these measurements before the study started, at four weeks, after the conventional walking period, and at four and eight weeks into the eccentric walking period.
We also tested their cognitive function using a digit symbol-substitution test at the same time points of other tests. And we asked participants to complete a questionnaire relating to their activities of daily living, such as dressing and moving around at home.
Finally, we tested participants’ blood sugar, cholesterol levels and complement component 1q (C1q) concentrations, a potential marker of sarcopenia (muscle wasting with ageing).
Regular walking won’t contract your muscles in the same way as eccentric walking.
alexei_tm/ShutterstockWhat did we find?
We found no significant changes in any of the outcomes in the first four weeks when participants walked conventionally.
From week four to 12, we found significant improvements in muscle strength (19%), chair-stand ability (24%), balance (45%) and a cognitive function test (21%).
Serum C1q concentration decreased by 10% after the eccentric walking intervention, indicating participants’ muscles were effectively stimulated.
The sample size of the study was small, so we need larger and more comprehensive studies to verify our findings and investigate whether eccentric walking is effective for sedentary people, older people, how the different types of eccentric exercise compare and the potential cognitive and mental health benefits.
But, in the meantime, “eccentric walking” appears to be a beneficial exercise that will extend your healthspan. It may look a bit eccentric if we insert lunges while walking on the street, but the more people do it and benefit from it, the less eccentric it will become.
Ken Nosaka, Professor of Exercise and Sports Science, Edith Cowan University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
What’s behind rising heart attack rates in younger adults
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Deaths from heart attacks have been in decline for decades, thanks to improved diagnosis and treatments. But, among younger adults under 50 and those from communities that have been marginalized, the trend has reversed.
More young people have suffered heart attacks each year since the 2000s—and the reasons why aren’t always clear.
Here’s what you need to know about heart attack trends in younger adults.
Heart attack deaths began declining in the 1980s
Heart disease has been a leading cause of death in the United States for more than a century, but rates have declined for decades as diagnosis and treatments improved. In the 1950s, half of all Americans who had heart attacks died, compared to one in eight today.
A 2023 study found that heart attack deaths declined 4 percent a year between 1999 and 2020.
The downward trend plateaued in the 2000s as heart attacks in young adults rose
In 2012, the decline in heart disease deaths in the U.S. began to slow. A 2018 study revealed that a growing number of younger adults were suffering heart attacks, with women more affected than men. Additionally, younger adults made up one-third of heart attack hospitalizations, with one in five heart attack patients being under 40.
The following year, data showed that heart attack rates among adults under 40 had increased steadily since 2006. Even more troubling, young patients were just as likely to die from heart attacks as patients more than a decade older.
Why are more younger adults having heart attacks?
Heart attacks have historically been viewed as a condition that primarily affects older adults. So, what has changed in recent decades that puts younger adults at higher risk?
Higher rates of obesity, diabetes, and high blood pressure
Several leading risk factors for heart attacks are rising among younger adults.
Between 2009 and 2020, diabetes and obesity rates increased in Americans ages 20 to 44.During the same period, hypertension, or high blood pressure, rates did not improve in younger adults overall and worsened in young Hispanic people. Notably, young Black adults had hypertension rates nearly twice as high as the general population.
Hypertension significantly increases the risk of heart attack and cardiovascular death in young adults.
Increased substance use
Substance use of all kinds increases the risk of cardiovascular issues, including heart attacks. A recent study found that cardiovascular deaths associated with substance use increased by 4 percent annually between 1999 and 2019.
The rise in substance use-related deaths has accelerated since 2012 and was particularly pronounced among women, younger adults (25-39), American Indians and Alaska Natives, and those in rural areas.
Alcohol was linked to 65 percent of the deaths, but stimulants (like methamphetamine) and cannabis were the substances associated with the greatest increase in cardiovascular deaths during the study period.
Poor mental health
Depression and poor mental health have been linked to cardiovascular issues in young adults. A 2023 study of nearly 600,000 adults under 50 found that depression and self-reported poor mental health are a risk factor for heart disease, regardless of socioeconomic or other cardiovascular risk factors.
Adults under 50 years consistently report mental health conditions at around twice the rate of older adults. Additionally, U.S. depression rates have trended up and reached an all-time high in 2023, when 17.8 percent of adults reported having depression.
Depression rates are rising fastest among women, adults under 44, and Black and Hispanic populations.
COVID-19
COVID-19 can cause real, lasting damage to the heart, increasing the risk of certain cardiovascular diseases for up to a year after infection. Vaccination reduces the risk of heart attack and other cardiovascular events caused by COVID-19 infection.
The first year of the pandemic marked the largest single-year spike in heart-related deaths in five years, including a 14 percent increase in heart attacks. In the second year of the pandemic, heart attacks in young adults increased by 30 percent.
Heart attack prevention
Not every heart attack is preventable, but everyone can take steps to reduce their risks. The American Heart Association recommends managing health conditions that increase heart disease risk, including diabetes, obesity, and high blood pressure.
Lifestyle changes like improving diet, reducing substance use, and increasing physical activity can also help reduce heart attack risk.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
Apples vs Figs – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing apples to figs, we picked the figs.
Why?
These two fruits are both known for being quite rich in sugar (but also rich in fiber, which offsets it metabolically), and indeed their macros are quite similar. That said, figs have slightly more protein, fiber, and carbs. Both are considered low glycemic index foods. We can consider this category a tie, or perhaps a nominal win for apples, whose glycemic index is the lower of the two. But since figs’ GI is also low, it’s really not a deciding factor.
In terms of vitamins, apples have more of vitamins C and E, while figs have more of vitamins A, B1, B2, B3, B5, B6, B9, and choline, with noteworthy margins of difference. A clear for figs here.
When it comes to minerals, apples are not higher in any minerals, while figs are several times higher in calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. An overwhelming win for figs.
Of course, enjoy either or both, but if you want nutritional density, apples simply cannot compete with figs.
Want to learn more?
You might like to read:
Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Thinking of trying a new diet? 4 questions to ask yourself before you do
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We live in a society that glorifies dieting, with around 42% of adults globally having tried to lose weight. Messages about dieting and weight loss are amplified on social media, with a never-ending cycle of weight loss fads and diet trends.
Amid often conflicting messages and misinformation, if you’re looking for diet advice online, it’s easy to become confused and overwhelmed.
So before diving into the latest weight loss trend or extreme diet, consider these four questions to help you make a more informed decision.
PeopleImages.com – Yuri A/Shutterstock 1. Is the diet realistic?
Have you considered the financial cost of maintaining the diet or lifestyle, and the time and resources that would be required? For example, do you need to purchase specific products, supplements, or follow a rigid meal plan?
If the diet is coming from someone who is trying to sell you something – such as a particular weight-loss product you need in order to follow the diet – this could be a particular red flag.
Many extreme diet recommendations come from a place of privilege and overlook food access, affordability, cooking skills, where you live, or even your culture and ethics.
If the diet has these sorts of issues it can lead to frustration, stress, stigmatisation and feelings of failure for the person trying to adhere to the diet. But the problem may be with the diet itself – not with you.
Many diets promoted online will be expensive, or require a lot of time and resources. artem evdokimov/Shutterstock 2. Is there evidence to support this diet?
Self-proclaimed “experts” online will often make claims focused on specific groups, known as target populations. This might be 30- to 50-year-old men with diabetes, for example.
In some cases, evidence for claims made may come from animal studies, which might not be applicable to humans at all.
So be aware that if research findings are for a group that doesn’t match your profile, then the results might not be relevant to you.
It takes time and a lot of high-quality studies to tell us a “diet” is safe and effective, not just one study. Ask yourself, is it supported by multiple studies in humans? Be critical and question the claims before you accept them.
For accurate information look for government websites, or ask your GP or dietitian.
3. How will this diet affect my life?
Food is much more than calories and nutrients. It plays many roles in our lives, and likewise diets can influence our lives in ways we often overlook.
Socially and culturally, food can be a point of connection and celebration. It can be a source of enjoyment, a source of comfort, or even a way to explore new parts of the world.
So when you’re considering a new diet, think about how it might affect meaningful moments for you. For example, if you’re going travelling, will your diet influence the food choices you make? Will you feel that you can’t sample the local cuisine? Or would you be deterred from going out for dinner with friends because of their choice of restaurant?
4. Will this diet make me feel guilty or affect my mental health?
What is your favourite meal? Does this diet “allow” you to eat it? Imagine visiting your mum who has prepared your favourite childhood meal. How will the diet affect your feelings about these special foods? Will it cause you to feel stressed or guilty about enjoying a birthday cake or a meal cooked by a loved one?
Studies have shown that dieting can negatively impact our mental health, and skipping meals can increase symptoms of depression and anxiety.
Many diets fail to consider the psychological aspects of eating, even though our mental health is just as important as physical health. Eating should not make you feel stressed, anxious, or guilty.
So before starting another diet, consider how it might affect your mental health.
Moving away from a dieting mindset
We’re frequently told that weight loss is the path to better health. Whereas, we can prioritise our health without focusing on our weight. Constant messages about the need to lose weight can also be harmful to mental health, and not necessarily helpful for physical health.
Our research has found eating in a way that prioritises health over weight loss is linked to a range of positive outcomes for our health and wellbeing. These include a more positive relationship with food, and less guilt and stress.
Our research also indicates mindful and intuitive eating practices – which focus on internal cues, body trust, and being present and mindful when eating – are related to lower levels of depression and stress, and greater body image and self-compassion.
But like anything, it takes practice and time to build a positive relationship with food. Be kind to yourself, seek out weight-inclusive health-care professionals, and the changes will come. Finally, remember you’re allowed to find joy in food.
Melissa Eaton, Accredited Practising Dietitian; PhD Candidate, University of Wollongong; Verena Vaiciurgis, Accredited Practising Dietitian; PhD Candidate, University of Wollongong, and Yasmine Probst, Associate Professor, School of Medical, Indigenous and Health Sciences, University of Wollongong
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
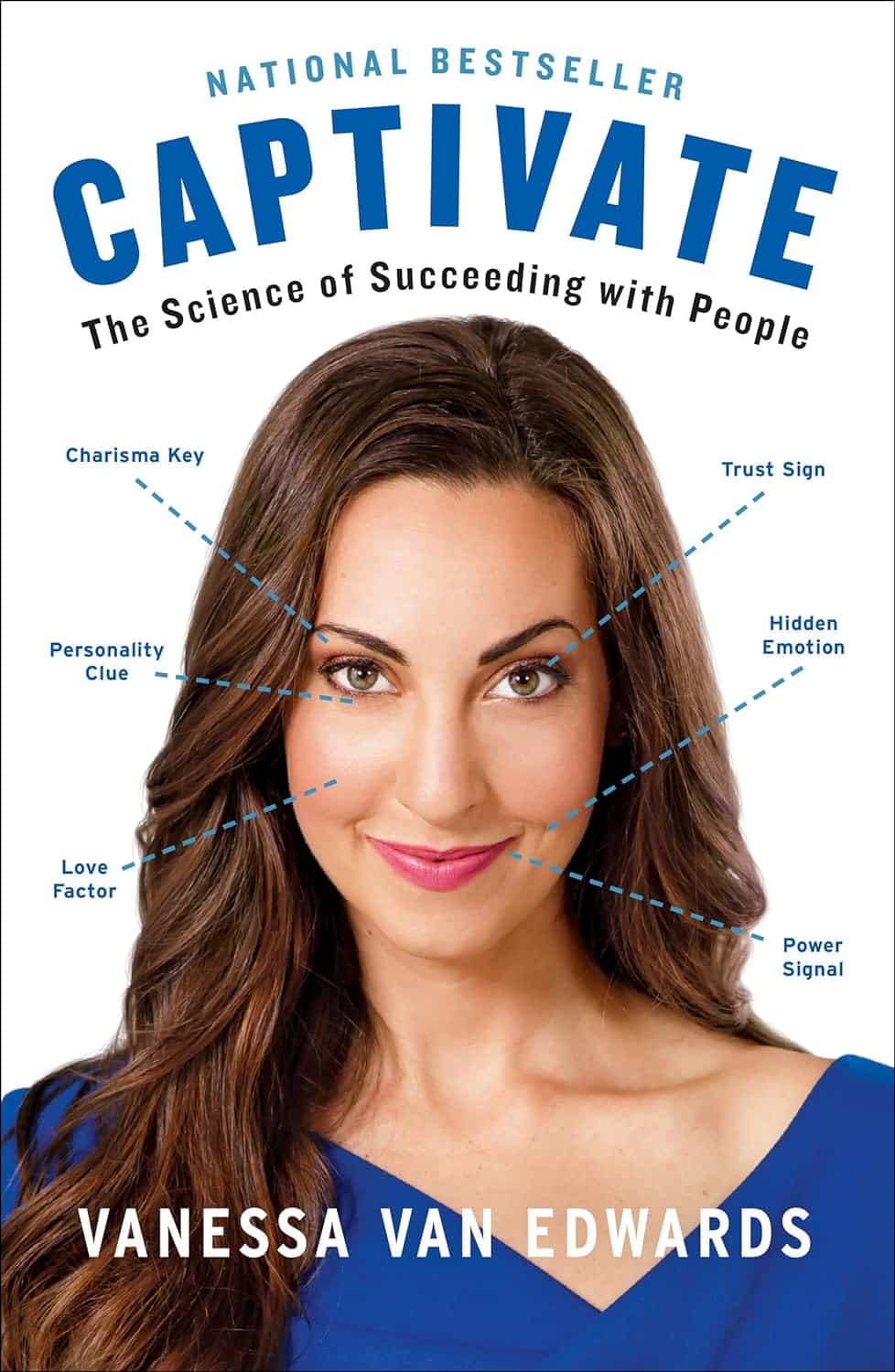
Captivate – by Vanessa van Edwards
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book isn’t just for one area of human interactions. It covers everything from the boardroom to the bedroom (not necessarily a progression with the same person!), business associates, friends, partners, kids, and more.
She presents information in a layered manner, covering for example, chapter-by-chapter:
- the first five minutes
- the first five hours
- the first five days
She also covers such things as:
- starting conversations in a way that makes you memorable (without making it weird!)
- the importance of really listening (and how to do that)
- collecting like-minded people appropriately
- introducing other people! Because a) it’s not all about you, but also b) you’re the person who knows everybody now
- where to stand at parties / networking events!
- dating and early-days dating messages
- reading the room, reading the people
All in all, a great resource for anyone who wants to make (and maintain!) meaningful relationships with those around you.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: