Buckwheat vs Oats – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing buckwheat to oats, we picked the oats.
Why?
First of all, for any thinking about the health concerns sometimes associated with wheat: buckwheat is not a kind of wheat, nor is it even in the same family; it’s not a grain, but a flowering plant. Buckwheat is to wheat as a lionfish is to lions.
That said, while these are both excellent foods, one of them is so good it makes the other one look bad in comparison:
In terms of macros, oats have more carbs, but also more protein and more fiber.
When it comes to vitamins, a clear winner emerges: oats have more of vitamins B1, B2, B5, B6, and B9, while buckwheat is higher in vitamin K and choline.
In the category of minerals, things are even more pronounced: oats are higher in calcium, iron, magnesium, manganese, phosphorus, potassium, and zinc. On the other hand, buckwheat is higher in selenium.
All in all: as ever, enjoy both, but if you’re picking one, oats cannot be beaten.
Want to learn more?
You might like to read:
The Best Kind Of Fiber For Overall Health?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
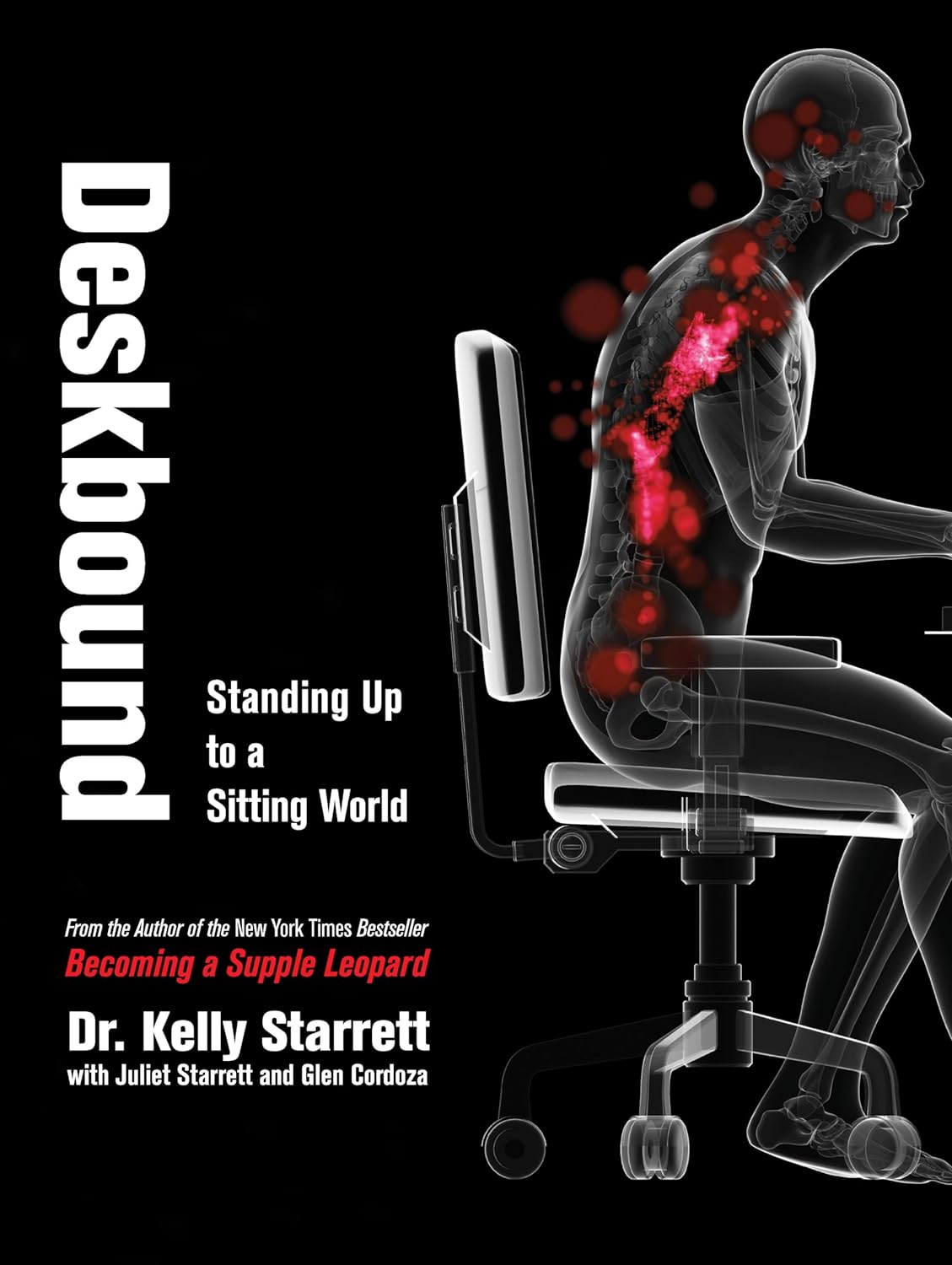
Deskbound – by Kelly Starrett and Glen Cordoza
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve all heard that “sitting is the new smoking”, and whether or not that’s an exaggeration (the jury’s out), one thing that is clear is that sitting is very bad.
Popular advice is “here’s how to sit with good posture and stretch your neck sometimes”… but that advice tends to come from companies that pay people to sit for a long time. They might not be the a very unbiased source.
Starrett and Cordoza offer better. After one opening chapter covering the multifarious ways sitting ruins our health, the rest of the book is all advice, covering:
- The principles of how the body is supposed to be
- The most important movements that we should be doing
- A dynamic workstation setup
- This is great, because “get a standing desk” tends to present more questions than answers, and can cause as much harm as good if done wrong
- The authors also cover how to progressively cut down on sitting, rather than try to go cold-turkey.
- They also recognize that not everyone can stand at all, and…
- Optimizing the sitting position, for when we must sit
- Exercises to maintain our general mobility and compensate about as well as we can for the body-unfriendly nature of modern life.
The book is mostly explanations, so at 682 pages, you can imagine it’s not just “get up, lazybones!”. Rather, things are explained in such detail (and with many high-quality medical diagrams) so that we can truly understand them.
Most of us have gone through life knowing we should have “better posture” and “move more”… but without the details, that can be hard to execute correctly, and worse, we can even sabotage our bodies unknowingly with incorrect form.
This book straightens all that out very comprehensively, and we highly recommend it.
Share This Post
-
It’s OK That You’re Not OK – by Megan Devine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Firstly, be aware: this is not a cheerful book. If you’re looking for something to life your mood after a loss, it will not be this.
What, then, will you find? A reminder that grief is also the final translation of love, and not necessarily something to be put aside as quickly as possible—or even ever, if we don’t want to.
Too often, society (and even therapists) will correctly note that no two instances of grief are the same (after all, no two people are, so definitely no two relationships are, so how could two instances of grief be?), but will still expect that if most people can move on quickly from most losses, that you should too, and that if you don’t then there is something pathological at hand that needs fixing.
Part one of the book covers this (and more) in a lot of detail; critics have called it a diatribe against the current status quo in the field of grief.
Part two of the book is about “what to do with your grief”, and addresses the reality of grief, how (and why) to stay alive when not doing so feels like a compelling option, dealing with grief’s physical side effects, and calming your mind in ways that actually work (without trying to sweep your grief under a rug).
Parts three and four are more about community—how to navigate the likely unhelpful efforts a lot of people may make in the early days, and when it comes to those people who can and will actually be a support, how to help them to help you.
In the category of criticism, she also plugs her own (paid, subscription-based) online community, which feels a little mercenary, especially as while community definitely can indeed help, the prospect of being promptly exiled from it if you stop paying, doesn’t.
Bottom line: if you have experienced grief and felt like moving on was the right thing to do, then this book isn’t the one for you. If, on the other hand, your grief feels more like something you will carry just as you carry the love you feel for them, then you’ll find a lot about that here.
Share This Post
-
Smarter Tomorrow – by Elizabeth Ricker
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Based heavily in hard science, with more than 450 citations in over 300 pages, the exhortation is not just “trust me, lol”.
Instead, she encourages the reader to experiment. Not like “try this and see if it works”, but “here’s how to try this, using scientific method with good controls and good record-keeping”.
The book is divided into sections, each with a projection of time required at the start and a summary at the end. The reading style is easy-reading throughout, without sacrificing substance.
It proposes seven key interventions. If just one works for you, it’ll be worth having bought and read the book. More likely most if not all will… Because that’s how science works.
Share This Post
Related Posts
-
Are You Making This Alcohol Mistake?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The famous “small glass of red per day” is, as is quite well-established now in science, but not so much in popular culture, known to be not a good idea.
What most people don’t know
Rethinking “One Drink a Day”:
- Outdated beliefs and flawed studies:
- The idea that “one drink a day is healthy” stems from flawed associative studies that included…
- unhealthy former heavy drinkers in the zero-drinks category, and
- healthy older individuals who continued light drinking due to good health, not because alcohol contributed to it, in the drinkers category
- In other words, they looked at former alcoholics whose health was ruined by drinking and said “aha, non-drinkers have bad health”, and looked at the survivors of survivorship bias and said “aha, light drinking is the key to good health”. Which of course is terrible science propped up by terrible abuse of statistics propped up by shoddy methodology.
- The idea that “one drink a day is healthy” stems from flawed associative studies that included…
- New research findings:
- A 2022 UK Biobank Study showed that even one drink a day leads to brain shrinkage, neuron death, and cognitive decline.
- Another study on CVD disproved the notion that light drinking benefits heart health once confounding variables were removed.
- There are plenty more, and at 10almonds we’ve done a main feature about it, but for now, you get the idea.
Some other things you should know:
Ethanol and acetaldehyde damage neurons responsible for impulse control, judgment, motor coordination, and memory formation, leading to cognitive decline. The feeling of being drunk results from the suppression and damage of these neurons. But while the drunk feeling wears off, the damage to neurons does not.
Alcohol causes cumulative DNA damage in neurons, accelerates brain aging, and prevents the formation of new neurons, similar to a slow, gradual stroke.
Broader Health Impacts of Alcohol
We’ve said it before, and we’ll say it again: alcohol is bad for pretty much everything.
Here are some examples mentioned in the video:
- Neurodegenerative diseases: heavy drinking increases the risk of Alzheimer’s, particularly in those genetically predisposed.
- Sleep disruption: alcohol reduces deep, restful sleep and hampers the brain’s natural detox process overnight, contributing to morning grogginess.
- Inflammation and immune suppression: alcohol increases inflammation, exacerbates autoimmune diseases (like psoriasis and arthritis), and weakens immune function.
- Cancer risk: alcohol is classified as a Group 1 carcinogen by the International Agency for Research on Cancer, linked to various cancers, especially breast cancer. Even light drinking increases breast cancer risk.
- Hormonal imbalances: in women, alcohol heightens PMS symptoms, reduces fertility, and increases testosterone. In men, it lowers sperm quality and disrupts hormones.
For more on all of these and more, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Can We Drink To Good Health? ← this is mostly about red wine and heart health
- How To Reduce Or Quit Alcohol ← this is about the more general reasons to quit, and how to do so
- What Happens To Your Body When You Stop Drinking Alcohol ← a realistic timeline of recovery
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- Outdated beliefs and flawed studies:
-
90% Of People Skip This Essential Exercise—Are You One Of Them?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Single-leg strengthening is essential for joint health at any age (unless you want to bunny-hop up and down the stairs with both feet at once, for example), yet many people overlook it. This neglect often leads to pain, stiffness, and a higher risk of injury.
Dr. Alyssa Kuhn, arthritis specialist, explains how to do it:
On the rise
In this video, different exercise variations—beginner, intermediate, and advanced—are presented to help you build strength at your own pace:
Beginner: start by using a chair, adding a cushion for support if needed. Sit at the edge and position one foot slightly in front of the other in a staggered stance. Stand up and sit down in a controlled manner, allowing the back leg to bear more weight and work harder than the front leg. Do 8–10 repetitions per side and pay attention to whether one side feels weaker. To build strength, incorporate this movement into daily activities, such as standing up from the couch. Master this variation before progressing, to avoid knee injury.
Intermediate: to make the exercise more challenging, you can either use a lower chair, or extend your front foot further out, shifting more weight to your back leg. Only modify one variable at a time to maintain control. Do 8–10 repetitions per side, ensuring proper form. A common mistake is allowing the back knee to move inward, which can cause knee stress. To prevent this, use a mirror to check your form and keep the knee and ankle aligned during movement.
Advanced: when you’re ready, extend your front leg completely with the heel on the ground and toes up, removing its stability and forcing the back leg to work even harder. Maintain controlled movement while keeping your knee and ankle aligned. Repeat the exercise on both sides, focusing extra effort on the weaker leg to build balanced strength.
For more on each of these, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
The Secret To Better Squats: Foot, Knee, & Ankle Mobility
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Never Too Late To Start Over: Finding Purpose At Any Age
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dana Findwell’s late 50s were not an easy time, but upon now hitting 60 (this week, at time of writing), she’s enthusiastically throwing herself into the things that bring her purpose, and so can you.
Start where you are
Findwell was already no stranger to starting again, having been married and divorced twice, and having moved frequently, requiring constant “life resets”.
Nevertheless, she always had her work to fall back on; she was a graphic designer and art director for 30 years… Until burnout struck.
And when burnout struck, so did COVID, resulting in the loss of her job. Her job wasn’t the only thing she lost though, as her mother died around the same time. All in all, it was a lot, and not the fun kind of “a lot”.
Struggling to find a new career direction, she ended up starting a small business for herself, so that she could direct the pace; pressing forwards as and when she had the energy. This became her new “ikigai“, the main thing that brings a sense of purpose to her life, but getting one part of her life back into order brought her attention to the rest; she realized she’d neglected her health, so she joined a gym. And a weightlifting class. And a hip-hop class. And she took up the practice of Japanese drumming (for the unfamiliar, this can be a rather athletic ability; it’s not a matter of sitting at a drum kit).
And now? Her future is still not clear, but that’s ok, because she’s making it as she goes, and she’s doing it her way, trusting in her ability to handle what may come up, and doing the things now that future-her will be glad of having done (e.g. laying the groundwork of both financial security and good health).
Change can sometimes be triggered by adverse circumstances, but there’s always the opportunity to find something better. For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: