Brown Rice vs Wild Rice – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing brown rice to wild rice, we picked the wild.
Why?
It’s close! But there are important distinctions.
First let’s clarify: despite the name and appearance, wild rice is botanically quite different from rice per se; it’s not the same species, it’s not even the same genus, though it is the same umbrella family. In other words, they’re about as closely related as humans and gorillas are to each other.
In terms of macros, wild rice has considerably more protein and a little more fiber, for slightly lower carbs.
Notably, however, wild rice’s carbs are a close-to-even mix of sucrose, fructose, and glucose, while brown rice’s carbs are 99% starch. Given the carb to fiber ratio, it’s worth noting that wild rice also has lower net carbs, and the lower glycemic index.
In the category of vitamins, wild rice leads with more of vitamins A, B2, B9, E, K, and choline. In contrast, brown rice has more of vitamins B1, B3, and B5. So, a moderate win for wild rice.
When it comes to minerals, brown rice finally gets a tally in its favor, even if only slightly: brown rice has more magnesium, manganese, phosphorus, and selenium, while wild rice has more copper, potassium, and zinc. They’re equal in calcium and iron, by the way. Still, this category stands as a 4:3 win for brown rice.
Adding up the categories makes a modest win for wild rice, and additionally, if we had to consider one of these things more important than the others, it’d be wild rice being higher in fiber and protein and lower in total carbs and net carbs.
Still, enjoy either or both, per your preference!
Want to learn more?
You might like to read:
- Brown Rice Protein: Strengths & Weaknesses
- Rice vs Buckwheat – Which is Healthier? ← it’s worth noting, by the way, that buckwheat is so unrelated from wheat that it’s not even the same family of plants. They are about as closely related as a lion and a lionfish are to each other.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Longevity… Simplified – by Dr. Howard Luks
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In the spirit of the book itself, we’ll keep this one simple:
The information in this book will not be new to regular readers of 10almonds, or at least, not if you’ve been with us for a while (because we can only cover so much per day, so long-time readers will have accumulated more knowledge).
On the other hand, the information is clear, correct, and very much stripped down to the most important basics. Not the very simplest basics, which would be an oversimplification to the point of inutility, but the most important basics.
To take an example, when it comes to exercise, he doesn’t say “exercise more” but rather that “a complete exercise program has four pillars: aerobic training, resistance training, balance training, and high-intensity interval training (HIIT)”, and then he goes about explaining, in clear and simple terms, how to do those.
The style is similar when it comes to diet, sleep, and body-part-specific chapters such as about heart health, brain health, and so forth.
Bottom line: if you’re a long-time 10almonds reader, you probably don’t need this one, but it’d be a great book for someone else who has expressed an interest in getting healthier, as it really is a top-tier “primer” in increasing health and healthspan.
Click here to check out Longevity… Simplified, and enjoy simplified longevity!
Share This Post
-
Walnuts vs Cashews – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing walnuts to cashews, we picked the walnuts.
Why?
It was close! In terms of macros, walnuts have about 2x the fiber, while cashews have slightly more protein. In the specific category of fats, walnuts have more fat. Looking further into it: walnuts’ fats are mostly polyunsaturated, while cashews’ fats are mostly monounsaturated, both of which are considered healthy.
Notwithstanding being both high in calories, neither nut is associated with weight gain—largely because of their low glycemic indices (of which, walnuts enjoy the slightly lower GI, but both are low-GI foods)
When it comes to vitamins, walnuts have more of vitamins A, B2, B3 B6, B9, and C, while cashews have more of vitamins B1, B5, E, and K. Because of the variation in their respective margins of difference, this is at best a moderate victory for walnuts, though.
In the category of minerals, cashews get their day, as walnuts have more calcium and manganese, while cashews have more copper, iron, magnesium, phosphorus, potassium, selenium, and zinc.
In short: unless you’re allergic, we recommend enjoying both of these nuts (and others) for a full range of benefits. However, if you’re going to pick one, walnuts win the day.
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Share This Post
-
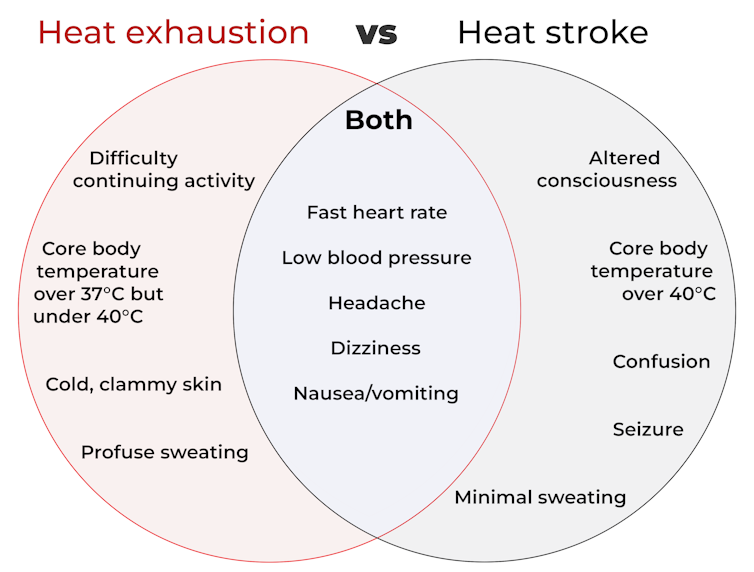
What’s the difference between heat exhaustion and heat stroke? One’s a medical emergency
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When British TV doctor Michael Mosley died last year in Greece after walking in extreme heat, local police said “heat exhaustion” was a contributing factor.
Since than a coroner could not find a definitive cause of death but said this was most likely due to an un-identified medical reason or heat stroke.
Heat exhaustion and heat stroke are two illnesses that relate to heat.
So what’s the difference?
Studio Nut/Shutterstock A spectrum of conditions
Heat-related illnesses range from mild to severe. They’re caused by exposure to excessive heat, whether from hot conditions, physical exertion, or both. The most common ones include:
- heat oedema: swelling of the hands, feet and ankles
- heat cramps: painful, involuntary muscle spasms usually after exercise
- heat syncope: fainting due to overheating
- heat exhaustion: when the body loses water due to excessive sweating, leading to a rise in core body temperature (but still under 40°C). Symptoms include lethargy, weakness and dizziness, but there’s no change to consciousness or mental clarity
- heat stroke: a medical emergency when the core body temperature is over 40°C. This can lead to serious problems related to the nervous system, such as confusion, seizures and unconsciousness including coma, leading to death.
As you can see from the diagram below, some symptoms of heat stroke and heat exhaustion overlap. This makes it hard to recognise the difference, even for medical professionals.
CC BY-SA How does this happen?
The human body is an incredibly efficient and adaptable machine, equipped with several in-built mechanisms to keep our core temperature at an optimal 37°C.
But in healthy people, regulation of body temperature begins to break down when it’s hotter than about 31°C with 100% humidity (think Darwin or Cairns) or about 38°C with 60% humidity (typical of other parts of Australia in summer).
This is because humid air makes it harder for sweat to evaporate and take heat with it. Without that cooling effect, the body starts to overheat.
Once the core temperature rises above 37°C, heat exhaustion can set in, which can cause intense thirst, weakness, nausea and dizziness.
If the body heat continues to build and the core body temperature rises above 40°C, a much more severe heat stroke could begin. At this point, it’s a life-threatening emergency requiring immediate medical attention.
At this temperature, our proteins start to denature (like an egg on a hotplate) and blood flow to the intestines stops. This makes the gut very leaky, allowing harmful substances such as endotoxins (toxic substances in some bacteria) and pathogens (disease causing microbes) to leak into the bloodstream.
The liver can’t detoxify these fast enough, leading to the whole body becoming inflamed, organs failing, and in the worst-case scenario, death.
Who’s most at risk?
People doing strenuous exercise, especially if they’re not in great shape, are among those at risk of heat exhaustion or heat stroke. Others at risk include those exposed to high temperatures and humidity, particularly when wearing heavy clothing or protective gear.
Outdoor workers such as farmers, firefighters and construction workers are at higher risk too. Certain health conditions, such as diabetes, heart disease, or lung conditions (such as COPD or chronic obstructive pulmonary disease), and people taking blood pressure medications, can also be more vulnerable.
Adults over 65, infants and young children are especially sensitive to heat as they are less able to physically cope with fluctuations in heat and humidity.
Firefighters are among those at risk of heat-related illness. structuresxx/Shutterstock How are these conditions managed?
The risk of serious illness or death from heat-related conditions is very low if treatment starts early.
For heat exhaustion, have the individual lie down in a cool, shady area, loosen or remove excess clothing, and cool them by fanning, moistening their skin, or immersing their hands and feet in cold water.
As people with heat exhaustion almost always are dehydrated and have low electrolytes (certain minerals in the blood), they will usually need to drink fluids.
However, emergency hospital care is essential for heat stroke. In hospital, health professionals will focus on stabilising the patient’s:
- airway (ensure no obstructions, for instance, vomit)
- breathing (look for signs of respiratory distress or oxygen deprivation)
- circulation (check pulse, blood pressure and signs of shock).
Meanwhile, they will use rapid-cooling techniques including immersing the whole body in cold water, or applying wet ice packs covering the whole body.
Take home points
Heat-related illnesses, such as heat stroke and heat exhaustion, are serious health conditions that can lead to severe illness, or even death.
With climate change, heat-related illness will become more common and more severe. So recognising the early signs and responding promptly are crucial to prevent serious complications.
Matthew Barton, Senior lecturer, School of Nursing and Midwifery, Griffith University and Michael Todorovic, Associate Professor of Medicine, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Say That Again: Using Hearing Aids Can Be Frustrating for Older Adults, but Necessary
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It was an every-other-day routine, full of frustration.
Every time my husband called his father, who was 94 when he died in 2022, he’d wait for his dad to find his hearing aids and put them in before they started talking.
Even then, my father-in-law could barely hear what my husband was saying. “What?” he’d ask over and over.
Then, there were the problems my father-in-law had replacing the devices’ batteries. And the times he’d end up in the hospital, unable to understand what people were saying because his hearing aids didn’t seem to be functioning. And the times he’d drop one of the devices and be unable to find it.
How many older adults have problems of this kind?
There’s no good data about this topic, according to Nicholas Reed, an assistant professor of epidemiology at Johns Hopkins Bloomberg School of Public Health who studies hearing loss. He did a literature search when I posed the question and came up empty.
Reed co-authored the most definitive study to date of hearing issues in older Americans, published in JAMA Open Network last year. Previous studies excluded people 80 and older. But data became available when a 2021 survey by the National Health and Aging Trends Study included hearing assessments conducted at people’s homes.
The results, based on a nationally representative sample of 2,803 people 71 and older, are eye-opening. Hearing problems become pervasive with advancing age, exceeding 90% in people 85 and older, compared with 53% of 71- to 74-year-olds. Also, hearing worsens over time, with more people experiencing moderate or severe deficits once they reach or exceed age 80, compared with people in their 70s.
However, only 29% of those with hearing loss used hearing aids. Multiple studies have documented barriers that inhibit use. Such devices, which Medicare doesn’t cover, are pricey, from nearly $1,000 for a good over-the-counter set (OTC hearing aids became available in 2022) to more than $6,000 for some prescription models. In some communities, hearing evaluation services are difficult to find. Also, people often associate hearing aids with being old and feel self-conscious about wearing them. And they tend to underestimate hearing problems that develop gradually.
Barbara Weinstein, a professor of audiology at the City University of New York Graduate Center and author of the textbook “Geriatric Audiology,” added another concern to this list when I reached out to her: usability.
“Hearing aids aren’t really designed for the population that most needs to use them,” she told me. “The move to make devices smaller and more sophisticated technologically isn’t right for many people who are older.”
That’s problematic because hearing loss raises the risk of cognitive decline, dementia, falls, depression, and social isolation.
What advice do specialists in hearing health have for older adults who have a hard time using their hearing aids? Here are some thoughts they shared.
Consider larger, customized devices. Many older people, especially those with arthritis, poor fine motor skills, compromised vision, and some degree of cognitive impairment, have a hard time manipulating small hearing aids and using them properly.
Lindsay Creed, associate director of audiology practices at the American Speech-Language-Hearing Association, said about half of her older clients have “some sort of dexterity issue, whether numbness or reduced movement or tremor or a lack of coordination.” Shekinah Mast, owner of Mast Audiology Services in Seaford, Delaware, estimates nearly half of her clients have vision issues.
For clients with dexterity challenges, Creed often recommends “behind-the-ear hearing aids,” with a loop over the ear, and customized molds that fit snugly in the ear. Customized earpieces are larger than standardized models.
“The more dexterity challenges you have, the better you’ll do with a larger device and with lots of practice picking it up, orienting it, and putting it in your ear,” said Marquitta Merkison, associate director of audiology practices at ASHA.
For older people with vision issues, Mast sometimes orders hearing aids in different colors for different ears. Also, she’ll help clients set up stands at home for storing devices, chargers, and accessories so they can readily find them each time they need them.
Opt for ease of use. Instead of buying devices that require replacing tiny batteries, select a device that can be charged overnight and operate for at least a day before being recharged, recommended Thomas Powers, a consultant to the Hearing Industries Association. These are now widely available.
People who are comfortable using a smartphone should consider using a phone app to change volume and other device settings. Dave Fabry, chief hearing health officer at Starkey, a major hearing aid manufacturer, said he has patients in their 80s and 90s “who’ve found that being able to hold a phone and use larger visible controls is easier than manipulating the hearing aid.”
If that’s too difficult, try a remote control. GN ReSound, another major manufacturer, has designed one with two large buttons that activate the volume control and programming for its hearing aids, said Megan Quilter, the company’s lead audiologist for research and development.
Check out accessories. Say you’re having trouble hearing other people in restaurants. You can ask the person across the table to clip a microphone to his shirt or put the mike in the center of the table. (The hearing aids will need to be programmed to allow the sound to be streamed to your ears.)
Another low-tech option: a hearing aid clip that connects to a piece of clothing to prevent a device from falling to the floor if it becomes dislodged from the ear.
Wear your hearing aids all day. “The No. 1 thing I hear from older adults is they think they don’t need to put on their hearing aids when they’re at home in a quiet environment,” said Erika Shakespeare, who owns Audiology and Hearing Aid Associates in La Grande, Oregon.
That’s based on a misunderstanding. Our brains need regular, not occasional, stimulation from our environments to optimize hearing, Shakespeare explained. This includes noises in seemingly quiet environments, such as the whoosh of a fan, the creak of a floor, or the wind’s wail outside a window.
“If the only time you wear hearing aids is when you think you need them, your brain doesn’t know how to process all those sounds,” she told me. Her rule of thumb: “Wear hearing aids all your waking hours.”
Consult a hearing professional. Everyone’s needs are different, so it’s a good idea to seek out an audiologist or hearing specialist who, for a fee, can provide guidance.
“Most older people are not going to know what they need” and what options exist without professional assistance, said Virginia Ramachandran, the head of audiology at Oticon, a major hearing aid manufacturer, and a past president of the American Academy of Audiology.
Her advice to older adults: Be “really open” about your challenges.
If you can’t afford hearing aids, ask a hearing professional for an appointment to go over features you should look for in over-the-counter devices. Make it clear you want the appointment to be about your needs, not a sales pitch, Reed said. Audiology practices don’t routinely offer this kind of service, but there’s good reason to ask since Medicare started covering once-a-year audiologist consultations last year.
We’re eager to hear from readers about questions you’d like answered, problems you’ve been having with your care, and advice you need in dealing with the health care system. Visit http://kffhealthnews.org/columnists to submit your requests or tips.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Science Of Sounds
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We Think You Might Like The Sound Of This…
We’ve written before about the benefits of mindfulness meditation, and how to do it.
We also reviewed a great book on a related topic:
This is Your Brain On Music – by Dr. Daniel Levitin
(yes, that’s the same neuroscientist that we featured as an expert talking about The Five Keys of Aging Healthily)
But what happens when we combine the two?
Mantra meditation & music
Most scientific studies that have been undertaken with regard to meditation tend to focus on mindfulness meditation. It’s easy, effective, and (which makes a difference when it comes to publication bias) is a very safe bet when it comes to funding.
However, today we’re going to look at mantra meditation, which has a lot in common, neurologically speaking, with music. Indeed, when the two were compared separately in a randomized control trial:
❝Daily mantra meditation or classical music listening may be beneficial for cognitive outcomes and quality of life of breast cancer survivors with cancer-related cognitive impairment.
The cognitive benefits appear to be sustained beyond the initial intervention period.❞
One possible reason for some of the similar benefits is the vagus nerve—whether intoning a mantra, or humming along to music, the vibrations can stimulate the vagus nerve, which in turn activates the parasympathetic nervous system, resulting in body-wide relaxation:
The Vagus Nerve (And How You Can Make Use Of It)
How effective is mantra meditation?
According to a large recent narrative review, it depends on your goal:
❝Based on the studies in the four important areas presented, there is no doubt of a strong connection between mantra meditation and human health.
Strong evidence has been found that practicing mantra meditation is effective in relieving stress and in coping with hypertension.
For the other two areas: anxiety and immunity, the evidence is inconclusive or not strong enough to firmly support the claim that the mantra meditation can be used to reduce anxiety or to improve immunity. ❞
Read in full: Scientific Evidence of Health Benefits by Practicing Mantra Meditation: Narrative Review
this is a very interesting read if you do have the time!
How do I practice mantra meditation?
The definition is broad, but the critical criteria are:
- You meditate…
- …using a mantra
Lest that seem flippant: those really are the two key points!
Meditation comes in various forms, and mantra meditation is a form of focussed meditation. While some focussed meditation forms may use a candle or some other focal point, in mantra meditation, the mantra itself provides the focus.
You may be wondering: what should the mantra be?
Classic and well-tested mantras include such simple things as the monosyllabic Sanskrit “Om” or “Ham”. We’re a health science newsletter, so we’ll leave esoteric meanings to other publications as they are beyond our scope, but we will say that these result, most naturally, in the humming sound that we mentioned earlier stimulates the vagus nerve.
But that’s not the only way. Practitioners of religions that have repetitive prayer systems (e.g. anything that uses prayer beads, for example) also provide the basis of focused meditation, using a mantra (in this case, usually a very short oft-repeated prayer phrase).
How long is needed for benefits?
Most studies into mantra meditation have used timed sessions of 15–30 minutes, with 20 minutes being a commonly-used session length, once per day. However…
- Vagus nerve benefits should appear a lot more quickly than that (under 5 minutes) in the case of mantras that cause that vibration we mentioned.
- Repetitive spoken prayers (or similar repeated short phrases, for the irreligious) will generally effect relaxation in whatever period of time it takes for your brain to be fully focused on what you are doing now, instead of what you were thinking about before. If using counting beads, then you probably already know what number works for you.
(again, as a health science publication, we cannot comment on any otherworldly benefits, but the worldly benefits seem reason enough to consider these practices for their potential therapeutic effects)
10almonds tip: for any meditative practice that you want to take approximately a given period of time, we recommend investing in a nice sand timer like this one, as this will not result in a jarring alarm going off!
Like to jazz things up a little?
Enjoy: Meditation That You’ll Actually Enjoy ← Meditation games!
Prefer to keep things to the basics?
Enjoy: No Frills, Evidence-Based Mindfulness ← The simplest scientific approach
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Being Mortal – by Dr. Atul Gawande
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Maybe you want to “live forever or die trying”, and that’s an understandable goal… But are you prepared for “or die trying” being the outcome?
This is not a cheerful book, if you’re anything like this reviewer, you will need a little towel or something to mop up the tears while you read. But it’s worth it.
Dying is one thing; fighting for life is even generally considered a noble endeavor. Suffering alone isn’t fun, losing independence can feel humiliating, and seeing someone who was always a tower of strength, now a frail shadow of their former self, reduced to begging for something that they’re “not allowed”, can be worse.
Do we want that for ourselves? For our loved ones? Can there be a happy medium between that, and the alternative to indeed “go gentle into that good night”?
Dr. Gawande, a surgeon well-acquainted with death and dying, thinks so. But it involves work on our part, and being prepared for hard decisions.
- What is most important to us, and what tradeoffs are we willing to make for it?
- What, even, is actually an option to us with the resources available?
- Can we make peace with a potentially bad lot? And… Should we?
- When is fighting important, and when is it self-destructive?
These (and others) are all difficult questions posed by Dr. Gawande, but critical ones.
We don’t usually quote other people’s reviews when reviewing books here, but let’s consider the following words from the end of a long review on Amazon:
❝If “dying as we lived” is some kind of standard for how we should go, then maybe alone and medicalized makes some sense right now after all.❞
Bottom line: we all deserve better than that. And if we don’t take the time to think about what’s most important, then time will take it from us. This very insightful book may not have all the answers, but it has the questions, and it can help a lot in exploring them and deciding what matters most to us in the end, really.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: