Beetroot vs Pumpkin – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing beetroot to pumpkin, we picked the beetroot.
Why?
It was close! And an argument could be made for either.
In terms of macros, beetroot has about 3x more protein and about 3x more fiber, as well as about 2x more carbs, making it the “more food per food” option. While both have a low glycemic index, we picked the beetroot here for its better numbers overall.
In the category of vitamins, beetroot has more of vitamins B6 and B9, while pumpkin has more of vitamins A, B2, B3, B5, E, and K. So, a fair win for pumpkin this time.
When it comes to minerals, though, beetroot has more calcium, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while pumpkin has a tiny bit more copper. An easy win for beetroot here.
In short, both are great, and although pumpkin shines in the vitamin category, beetroot wins on overall nutritional density.
Want to learn more?
You might like to read:
No, beetroot isn’t vegetable Viagra. But here’s what it can do
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Toe-Tapping Tip For Better Balance
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Balance is critical for health especially in older age, since it’s amazing how much else can go dramatically and suddenly wrong after a fall. So, here’s an exercise to give great balance and stability:
How to do it
You will need:
- Something to hold onto, such as a countertop
- A target on the floor, such as a mark or a coin
The steps:
- Lift one leg up, bring your foot forward, and tap the object in front of you.
- Then, bring that foot back to where it started.
- Next, switch to the other leg and tap.
- Alternate between your right and left legs, shifting back and forth.
- Your goal is to do this for 10 repetitions on each leg without holding on.
How it works:
Whenever you tap, you have to lift one leg up and reach it out in front of you. Doing this requires you to stand on one leg while moving a weight (namely: your other leg), which is something many people, especially upon getting older, are hesitant to do. If you’re unable to stand on one leg, let alone move your center of gravity (per the counterbalance of the other leg) while doing so, you may end up shuffling and walking with your feet sliding across the ground—something you really want to avoid.
For more on all of this plus a visual demonstration, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Fall Special ← this is about not falling, or, failing that, minimizing injury if you do
Take care!
Share This Post
-
Blood-Sugar Balancing Beetroot Cutlets
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
These beetroot cutlets are meaty and proteinous and fibrous and even have a healthy collection of fats, making these much better for your heart and blood than an animal-based equivalent.
You will need
- 1 can kidney beans, drained and rinsed (or 1 cup same, cooked, drained, and rinsed)
- ½ cup chopped roasted or steamed beetroot, blotted dry
- ½ cup chopped walnuts (if allergic, substitute with ¼ cup pumpkin seeds)
- ½ cup cooked (ideally: mixed) grains of your choice (if you need gluten-free, there are plenty of gluten-free grains and pseudocereals)
- ¼ cup finely chopped onion
- ¼ bulb garlic, minced or crushed
- 2 tbsp nutritional yeast
- 2 tbsp ground flaxseeds
- 2 tbsp ground chia seeds
- 2 tsp tomato purée
- 1 tsp black pepper
- ½ tsp white miso paste
- ½ tsp smoked paprika
- ½ tsp cayenne pepper
- ¼ tsp MSG or ½ tsp low-sodium salt
Method
(we suggest you read everything at least once before doing anything)
1) Combine the beetroot, beans, walnuts, grains, and onion in a food processor, and process until a coarse even mixture.
2) Add the remaining ingredients and process to mix thoroughly.
3) Transfer the mixture to a clean work surface and divide into six balls. If the structural integrity is not good (i.e. too soft), add a little more of any or all of these ingredients: chopped walnuts, ground flax, ground chia, nutritional yeast.
4) Press the balls firmly into cutlets, and refrigerate for at least 1 hour, but longer is even better if you have the time. Alternatively, if you’d like to freeze them for later use, then this is the point at which to do that.
5) Preheat the oven to 375℉ / 190℃.
6) Roast the cutlets on a baking tray lined with baking paper, for about 30 minutes, turning over carefully with a spatula halfway through. They should be firm when done; if they’re not, give them a little longer.
7) Serve hot, for example on a bed of greens and with a drizzle of aged balsamic vinegar.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Beetroot’s Many Benefits
- Our Top 5 Spices: How Much Is Enough For Benefits?
- What Omega-3 Fatty Acids Really Do For Us
- Three Daily Servings of Beans?
- If You’re Not Taking Chia, You’re Missing Out
Take care!
Share This Post
-
Without Medicare Part B’s Shield, Patient’s Family Owes $81,000 for a Single Air-Ambulance Flight
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Without Medicare Part B’s Shield, Patient’s Family Owes $81,000 for a Single Air-Ambulance Flight
Debra Prichard was a retired factory worker who was careful with her money, including what she spent on medical care, said her daughter, Alicia Wieberg. “She was the kind of person who didn’t go to the doctor for anything.”
That ended last year, when the rural Tennessee resident suffered a devastating stroke and several aneurysms. She twice was rushed from her local hospital to Vanderbilt University Medical Center in Nashville, 79 miles away, where she was treated by brain specialists. She died Oct. 31 at age 70.
One of Prichard’s trips to the Nashville hospital was via helicopter ambulance. Wieberg said she had heard such flights could be pricey, but she didn’t realize how extraordinary the charge would be — or how her mother’s skimping on Medicare coverage could leave the family on the hook.
Then the bill came.
The Patient: Debra Prichard, who had Medicare Part A insurance before she died.
Medical Service: An air-ambulance flight to Vanderbilt University Medical Center.
Service Provider: Med-Trans Corp., a medical transportation service that is part of Global Medical Response, an industry giant backed by private equity investors. The larger company operates in all 50 states and says it has a total of 498 helicopters and airplanes.
Total Bill: $81,739.40, none of which was covered by insurance.
What Gives: Sky-high bills from air-ambulance providers have sparked complaints and federal action in recent years.
For patients with private insurance coverage, the No Surprises Act, which went into effect in 2022, bars air-ambulance companies from billing people more than they would pay if the service were considered “in-network” with their health insurers. For patients with public coverage, such as Medicare or Medicaid, the government sets payment rates at much lower levels than the companies charge.
But Prichard had opted out of the portion of Medicare that covers ambulance services.
That meant when the bill arrived less than two weeks after her death, her estate was expected to pay the full air-ambulance fee of nearly $82,000. The main assets are 12 acres of land and her home in Decherd, Tennessee, where she lived for 48 years and raised two children. The bill for a single helicopter ride could eat up roughly a third of the estate’s value, said Wieberg, who is executor.
The family’s predicament stems from the complicated nature of Medicare coverage.
Prichard was enrolled only in Medicare Part A, which is free to most Americans 65 or older. That section of the federal insurance program covers inpatient care, and it paid most of her hospital bills, her daughter said.
But Prichard declined other Medicare coverage, including Part B, which handles such things as doctor visits, outpatient treatment, and ambulance rides. Her daughter suspects she skipped that coverage to avoid the premiums most recipients pay, which currently are about $175 a month.
Loren Adler, a health economist for the Brookings Institution who studies ambulance bills, estimated the maximum charge that Medicare would have allowed for Prichard’s flight would have been less than $10,000 if she’d signed up for Part B. The patient’s share of that would have been less than $2,000. Her estate might have owed nothing if she’d also purchased supplemental “Medigap” coverage, as many Medicare members do to cover things like coinsurance, he said.
Nicole Michel, a spokesperson for Global Medical Response, the ambulance provider, agreed with Adler’s estimate that Medicare would have limited the charge for the flight to less than $10,000. But she said the federal program’s payment rates don’t cover the cost of providing air-ambulance services.
“Our patient advocacy team is actively engaged with Ms. Wieberg’s attorney to determine if there was any other applicable medical coverage on the date of service that we could bill to,” Michel wrote in an email to KFF Health News. “If not, we are fully committed to working with Ms. Wieberg, as we do with all our patients, to find an equitable solution.”
The Resolution: In mid-February, Wieberg said the company had not offered to reduce the bill.
Wieberg said she and the attorney handling her mother’s estate both contacted the company, seeking a reduction in the bill. She said she also contacted Medicare officials, filled out a form on the No Surprises Act website, and filed a complaint with Tennessee regulators who oversee ambulance services. She said she was notified Feb. 12 that the company filed a legal claim against the estate for the entire amount.
Wieberg said other health care providers, including ground ambulance services and the Vanderbilt hospital, wound up waiving several thousand dollars in unpaid fees for services they provided to Prichard that are normally covered by Medicare Part B.
But as it stands, Prichard’s estate owes about $81,740 to the air-ambulance company.
More from Bill of the Month
- The Colonoscopies Were Free. But the ‘Surgical Trays’ Came With $600 Price Tags. Jan 25, 2024
- When a Quick Telehealth Visit Yields Multiple Surprises Beyond a Big Bill Dec 19, 2023
- Out for Blood? For Routine Lab Work, the Hospital Billed Her $2,400 Nov 21, 2023
The Takeaway: People who are eligible for Medicare are encouraged to sign up for Part B, unless they have private health insurance through an employer or spouse.
“If someone with Medicare finds that they are having difficulty paying the Medicare Part B premiums, there are resources available to help compare Medicare coverage choices and learn about options to help pay for Medicare costs,” Meena Seshamani, director of the federal Center for Medicare, said in an email to KFF Health News.
She noted that every state offers free counseling to help people navigate Medicare.
In Tennessee, that counseling is offered by the State Health Insurance Assistance Program. Its director, Lori Galbreath, told KFF Health News she wishes more seniors would discuss their health coverage options with trained counselors like hers.
“Every Medicare recipient’s experience is different,” she said. “We can look at their different situations and give them an unbiased view of what their next best steps could be.”
Counselors advise that many people with modest incomes enroll in a Medicare Savings Program, which can cover their Part B premiums. In 2023, Tennessee residents could qualify for such assistance if they made less than $1,660 monthly as a single person or $2,239 as a married couple. Many people also could obtain help with other out-of-pocket expenses, such as copays for medical services.
Wieberg, who lives in Missouri, has been preparing the family home for sale.
She said the struggle over her mother’s air-ambulance bill makes her wonder why Medicare is split into pieces, with free coverage for inpatient care under Part A, but premiums for coverage of other crucial services under Part B.
“Anybody past the age of 70 is likely going to need both,” she said. “And so why make it a decision of what you can afford or not afford, or what you think you’re going to use or not use?”
Bill of the Month is a crowdsourced investigation by KFF Health News and NPR that dissects and explains medical bills. Do you have an interesting medical bill you want to share with us? Tell us about it!
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
Related Posts
-
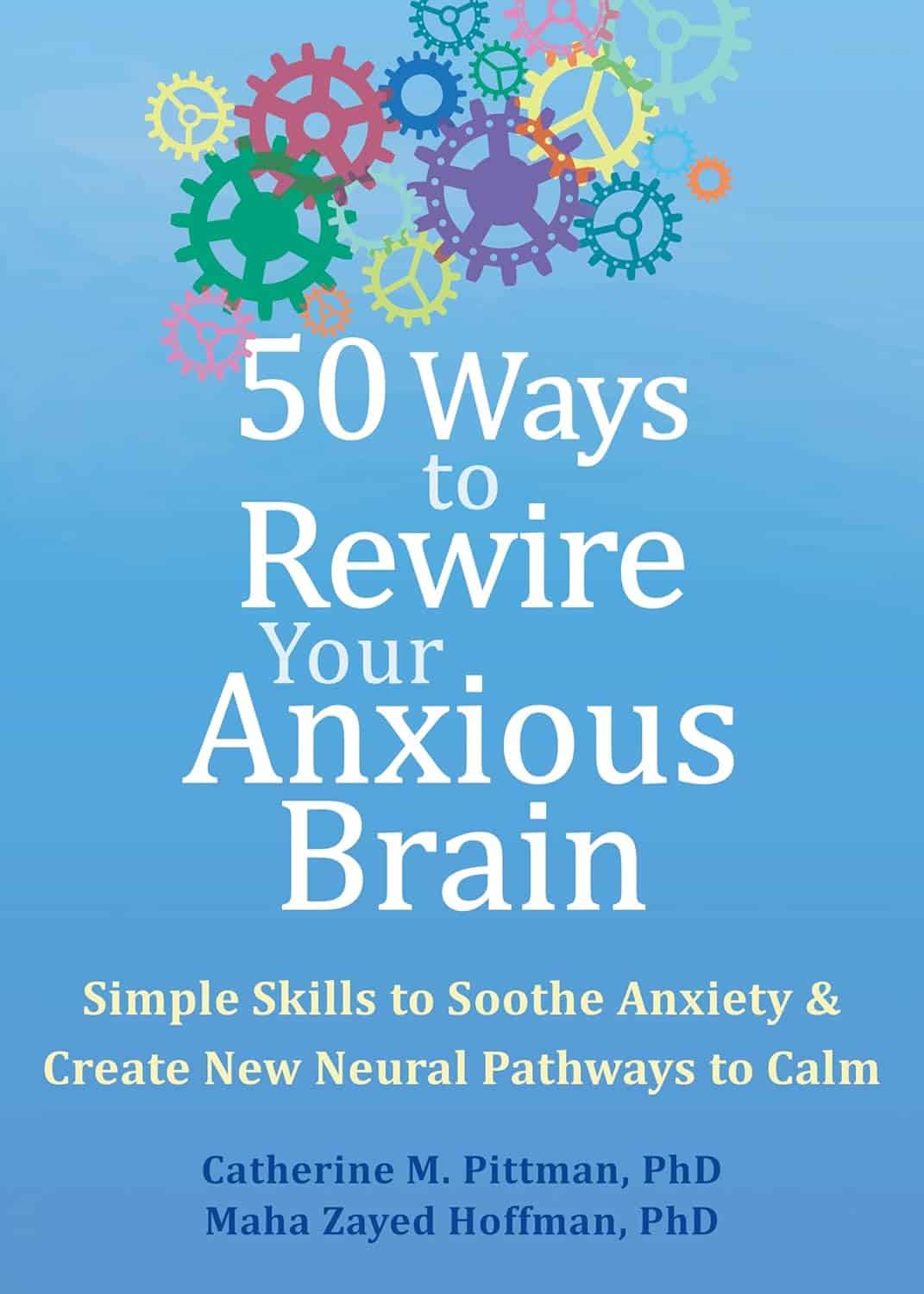
50 Ways To Rewire Your Anxious Brain – by Dr. Catherine Pittman & Dr. Maha Zayed-Hoffman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The book is divided into sections:
- Calming the amygdala
- Rewiring the amygdala
- Calming the cortex
- Resisting cortex traps
…each with a dozen or so ways to do exactly what it says in the title: rewire your anxious brain.
The authors take the stance that since our brain is changing all the time, we might as well choose the direction we prefer. They then set out to provide the tools for the lay reader to do that, and (in that fourth section we mentioned) how to avoid accidentally doing the opposite, no matter how tempting doing the opposite may be.
For a book written by two PhD scientists where a large portion of it is about neuroscience, the style is very light pop science (just a few in-line citations every few pages, where they couldn’t resist the urge), and the focus is on being useful to the reader throughout. This all makes for reassuringly science-based but accessibly readable book.
The fact that the main material comes in the form of 50 very short chapters also makes it a lot more readable for those for whom sitting down to read a lot at a time can be off-putting.
Bottom line: if you experience anxiety and would like to experience it less, this book will guide you through how to get there.
Click here to check out 50 Ways To Rewire Your Anxious Brain, and rewire your anxious brain!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The 5 Love Languages Gone Wrong
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Levelling up the 5 love languages
The saying “happy wife; happy life” certainly goes regardless of gender, and if we’re partnered, it’s difficult to thrive in our individual lives if we’re not thriving as a couple. So, with the usual note that mental health is also just health, let’s take a look at getting beyond the basics of a well-known, often clumsily-applied model:
The 5 love languages
You’re probably familiar with “the 5 love languages”, as developed by Dr. Gary Chapman. If not, they are:
- Acts of Service
- Gift-Giving
- Physical Touch
- Quality Time
- Words of Affirmation
The idea is that we each weight these differently, and problems can arise when a couple are “speaking a different language”.
So, is this a basic compatibility test?
It doesn’t have to be!
We can, if we’re aware of each other’s primary love languages, make an effort to do a thing we wouldn’t necessarily do automatically, to ensure they’re loved the way they need to be.
But…
What a lot of people overlook is that we can also have different primary love languages for giving and for receiving. And, missing that can mean that even taking each other’s primarily love languages into account, efforts to make a partner feel loved, or to feel loved oneself, can miss 50% of the time.
For example, I (your writer here today, hi) could be asked my primary love language and respond without hesitation “Acts of Service!” because that’s my go-to for expressing love.
I’m the person who’ll run around bringing drinks, do all the housework, and without being indelicate, will tend towards giving in the bedroom. But…
A partner trying to act on that information to make me feel loved by giving Acts of Service would be doomed to catastrophic failure, because my knee-jerk reaction would be “No, here, let me do that for you!”
So it’s important for partners to ask each other…
- Not: “what’s your primary love language?” ❌
- But: “what’s your primary way of expressing love?” ✅
- And: “which love language makes you feel most loved?” ✅
For what it’s worth, I thrive on Words of Affirmation, so thanks again to everyone who leaves kind feedback on our articles! It lets me know I provided a good Act of Service
So far, so simple, right? You and your partner (or: other person! Because as we’ve just seen, these go for all kinds of dynamics, not just romantic partnerships) need to be aware of each other’s preferred love languages for giving and receiving.
But…
There’s another pitfall that many fall into, and that’s assuming that the other person has the same idea about what a given love language means, when there’s more to clarify.
For example:
- Acts of Service: is it more important that the service be useful, or that it took effort?
- Gift-Giving: is it better that a gift be more expensive, or more thoughtful and personal?
- Physical Touch: what counts here? If we’re shoulder-to-shoulder on the couch, is that physical touch or is something more active needed?
- Quality Time: does it count if we’re both doing our own thing but together in the same room, comfortable in silence together? Or does it need to be a more active and involved activity together? And is it quality time if we’re at a social event together, or does it need to be just us?
- Words of Affirmation: what, exactly, do we need to hear? For romantic partners, “I love you” can often be important, but is there something else we need to hear? Perhaps a “because…”, or perhaps a “so much that…”, or perhaps something else entirely? Does it no longer count if we have to put the words in our partner’s mouth, or is that just good two-way communication?
Bottom line:
There’s a lot more to this than a “What’s your love language?” click-through quiz, but with a little application and good communication, this model can really resolve a lot of would-be problems that can grow from feeling unappreciated or such. And, the same principles go just the same for friends and others as they do for romantic partners.
In short, it’s one of the keys to good interpersonal relationships in general—something critical for our overall well-being!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The High-Protein, High-Fiber Superfood Salad You’ll Want To Enjoy Daily
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This salad from Nisha Vora at Rainbow Plant Life has 30g protein and takes minutes to prepare, while being tasty enough to look forward to eating each day:
Easy preparation
Prepare the toppings first; you can do a week’s in advance at once:
- Roasted chickpeas:
- Drain, rinse, and dry two cans of chickpeas.
- Toss with olive oil, salt, and pepper.
- Roast at 425°F for 30–35 minutes.
- Roasted walnuts:
- Chop and toss with olive oil, salt, and pepper.
- Roast at 350°F for 12 minutes after chickpeas finish.
As for the salad base:
- Kale:
- Remove tough stems, slice thinly.
- Wash and massage with lemon juice and salt to soften.
- Cabbage:
- Slice thinly with a knife or mandolin.
- Store in a sealed bag in the fridge for up to a week.
Red wine vinaigrette dressing:
- Key ingredients: red wine vinegar, lemon juice, red pepper flakes, garlic, olive oil.
- Can be stored in the fridge for up to 10 days.
Putting it all together:
- Toss kale and cabbage with vinaigrette by hand.
- Add roasted chickpeas and walnuts for crunch.
- Include a protein source like tofu (store-bought curry tofu recommended).
- Mix in fresh vegetables like grated carrots, sliced bell peppers, or beets.
- Add extras like sauerkraut, avocado, pickled onions, and such.
- Top with fresh herbs (she recommends parsley, basil, or dill).
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
21 Most Beneficial Polyphenols & What Foods Have Them
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- Roasted chickpeas: