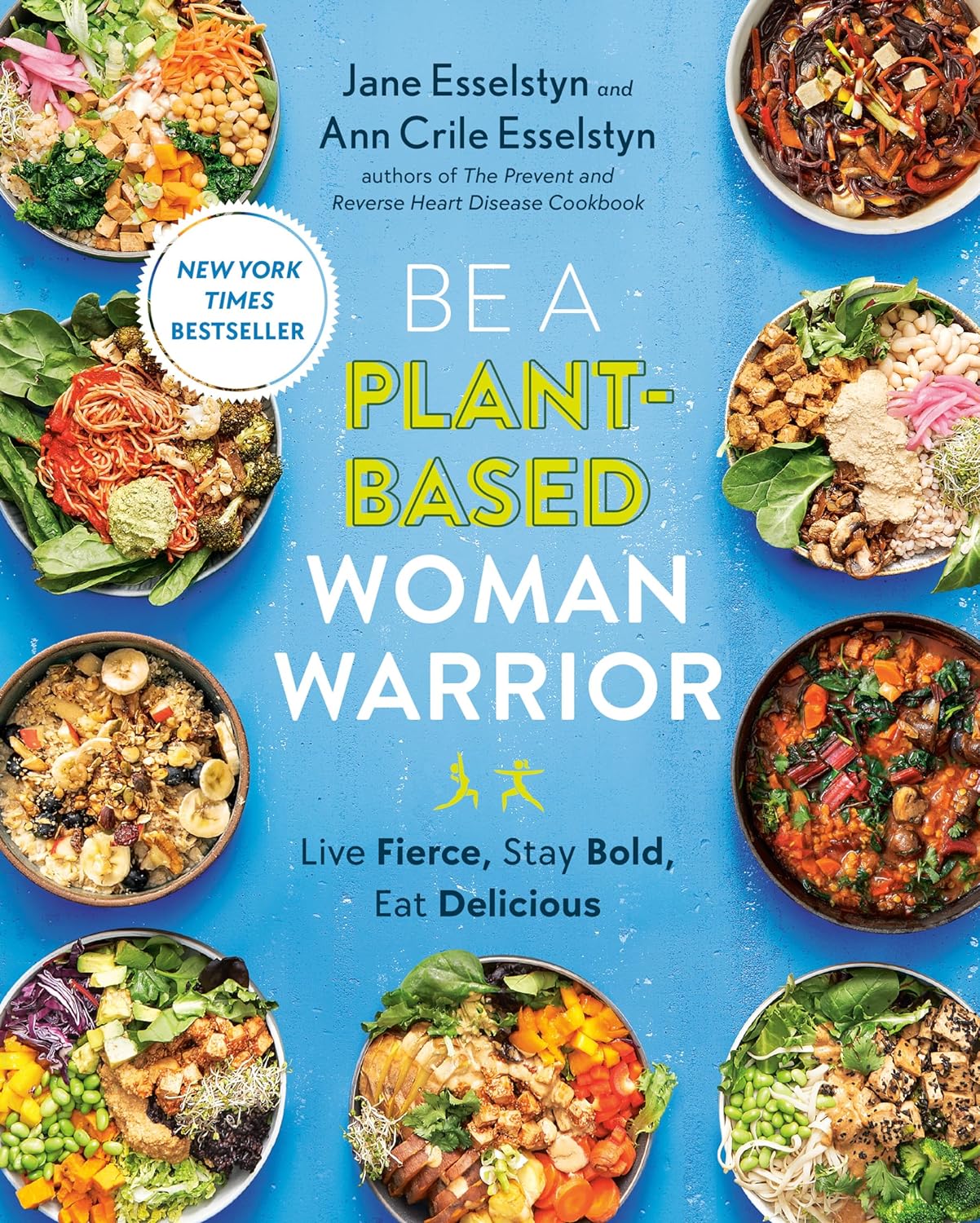
Be A Plant-Based Woman Warrior – by Jane Esselstyn & Ann Esselstyn
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Notwithstanding the title, this book is not about being a woman or a warrior, but let us share what one reviewer on Amazon wrote:
❝I don’t want to become a plant based woman warrior. The sex change would be traumatic for me. However, as a man who proudly takes ballet classes and Pilates, I am old enough not to worry about stereotypes. When I see a good thing, I am going to use it❞
The authors, a mother-and-daughter team in their 80s and 50s respectively, do give a focus on things that disproportionally affect women, and rectifying those things with diet, especially in one of the opening chapters.
Most the book, however, is about preventing/reversing things that can affect everyone, such as heart disease, diabetes, inflammation and the autoimmune diseases associated with such, and cancer in general, hence the dietary advice being good for most people (unless you have an unusually restrictive diet).
We get an overview of the pantry we should cultivate and curate, as well as some basic kitchen skills that will see us well for the rest of the book, such as how to make oat flour and other similar mini-recipes, before getting into the main recipes themselves.
About the recipes: they are mostly quite simple, though often rely on having pre-prepared items from the mini-recipes we mentioned earlier. They’re all vegan, mostly but not all gluten-free, whole foods, no added sugar, and as for oil… Well, it seems to be not necessarily oil-free, but rather oil-taboo. You see, they just don’t mention it. For example, when they say to caramelize onions, they say to heat a skillet, and when it is hot, add the onions, and stir until browned. They don’t mention any oil in the ingredients or in the steps. It is a mystery. 10almonds note: we recommend olive oil, or avocado oil if you prefer a milder taste and/or need a higher smoke point.
Bottom line: the odd oil taboo aside, this is a good book of simple recipes that teaches some good plant-based kitchen skills while working with a healthy, whole food pantry.
Click here to check out Be A Plant-Based Woman Warrior, and be a plant-based woman warrior!
Or at the very least: be a plant-based cook regardless of gender, hopefully without war, and enjoy the additions to your culinary repertoire
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Grains: Bread Of Life, Or Cereal Killer?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Going Against The Grain?
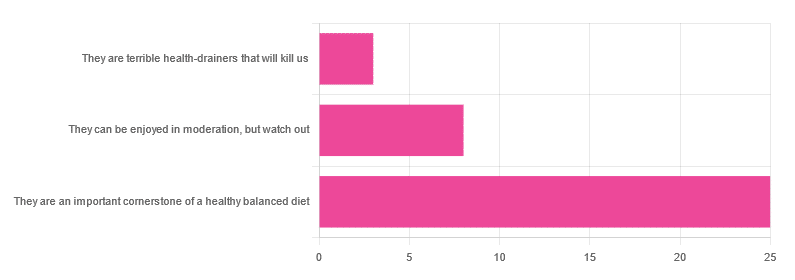
In Wednesday’s newsletter, we asked you for your health-related opinion of grains (aside from any gluten-specific concerns), and got the above-depicted, below-described, set of responses:
- About 69% said “They are an important cornerstone of a healthy balanced diet”
- About 22% said “They can be enjoyed in moderation, but watch out”
- About 8% said “They are terrible health-drainers that will kill us”
So, what does the science say?
They are terrible health-drainers that will kill us: True or False?
True or False depending on the manner of their consumption!
There is a big difference between the average pizza base and a bowl of oats, for instance. Or rather, there are a lot of differences, but what’s most critical here?
The key is: refined and ultraprocessed grains are so inferior to whole grains as to be actively negative for health in most cases for most people most of the time.
But! It’s not because processing is ontologically evil (in reality: some processed foods are healthy, and some unprocessed foods are poisonous). although it is a very good general rule of thumb.
So, we need to understand the “why” behind the “key” that we just gave above, and that’s mostly about the resultant glycemic index and associated metrics (glycemic load, insulin index, etc).
In the case of refined and ultraprocessed grains, our body gains sugar faster than it can process it, and stores it wherever and however it can, like someone who has just realised that they will be entertaining a houseguest in 10 minutes and must tidy up super-rapidly by hiding things wherever they’ll fit.
And when the body tries to do this with sugar from refined grains, the result is very bad for multiple organs (most notably the liver, but the pancreas takes quite a hit too) which in turn causes damage elsewhere in the body, not to mention that we now have urgently-produced fat stored in unfortunate places like our liver and abdominal cavity when it should have gone to subcutaneous fat stores instead.
In contrast, whole grains come with fiber that slows down the absorption of the sugars, such that the body can deal with them in an ideal fashion, which usually means:
- using them immediately, or
- storing them as muscle glycogen, or
- storing them as subcutaneous fat
👆 that’s an oversimplification, but we only have so much room here.
For more on this, see:
Glycemic Index vs Glycemic Load vs Insulin Index
And for why this matters, see:
Which Sugars Are Healthier, And Which Are Just The Same?
And for fixing it, see:
They can be enjoyed in moderation, but watch out: True or False?
Technically True but functionally False:
- Technically true: “in moderation” is doing a lot of heavy lifting here. One person’s “moderation” may be another person’s “abstemiousness” or “gluttony”.
- Functionally false: while of course extreme consumption of pretty much anything is going to be bad, unless you are Cereals Georg eating 10,000 cereals each day and being a statistical outlier, the issue is not the quantity so much as the quality.
Quality, we discussed above—and that is, as we say, paramount. As for quantity however, you might want to know a baseline for “getting enough”, so…
They are an important cornerstone of a healthy balanced diet: True or False?
True! This one’s quite straightforward.
3 servings (each being 90g, or about ½ cup) of whole grains per day is associated with a 22% reduction in risk of heart disease, 5% reduction in all-cause mortality, and a lot of benefits across a lot of disease risks:
❝This meta-analysis provides further evidence that whole grain intake is associated with a reduced risk of coronary heart disease, cardiovascular disease, and total cancer, and mortality from all causes, respiratory diseases, infectious diseases, diabetes, and all non-cardiovascular, non-cancer causes.
These findings support dietary guidelines that recommend increased intake of whole grain to reduce the risk of chronic diseases and premature mortality.❞
~ Dr. Dagfinn Aune et al.
We’d like to give a lot more sources for the same findings, as well as papers for all the individual claims, but frankly, there are so many that there isn’t room. Suffice it to say, this is neither controversial nor uncertain; these benefits are well-established.
Here’s a very informative pop-science article, that also covers some of the things we discussed earlier (it shows what happens during refinement of grains) before getting on to recommendations and more citations for claims than we can fit here:
Harvard School Of Public Health | Whole Grains
“That’s all great, but what if I am concerned about gluten?”
There certainly are reasons you might be, be it because of a sensitivity, allergy, or just because perhaps you’d like to know more.
Let’s first mention: not all grains contain gluten, so it’s perfectly possible to enjoy naturally gluten-free grains (such as oats and rice) as well as gluten-free pseudocereals, which are not actually grains but do the same job in culinary and nutritional terms (such as quinoa and buckwheat, despite the latter’s name).
Finally, if you’d like to know more about gluten’s health considerations, then check out our previous mythbusting special:
Enjoy!
Share This Post
-
Why do I poo in the morning? A gut expert explains
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
No, you’re not imagining it. People really are more likely to poo in the morning, shortly after breakfast. Researchers have actually studied this.
But why mornings? What if you tend to poo later in the day? And is it worth training yourself to be a morning pooper?
To understand what makes us poo when we do, we need to consider a range of factors including our body clock, gut muscles and what we have for breakfast.
Here’s what the science says.
H_Ko/Shutterstock So morning poos are real?
In a UK study from the early 1990s, researchers asked nearly 2,000 men and women in Bristol about their bowel habits.
The most common time to poo was in the early morning. The peak time was 7-8am for men and about an hour later for women. The researchers speculated that the earlier time for men was because they woke up earlier for work.
About a decade later, a Chinese study found a similar pattern. Some 77% of the almost 2,500 participants said they did a poo in the morning.
But why the morning?
There are a few reasons. The first involves our circadian rhythm – our 24-hour internal clock that helps regulate bodily processes, such as digestion.
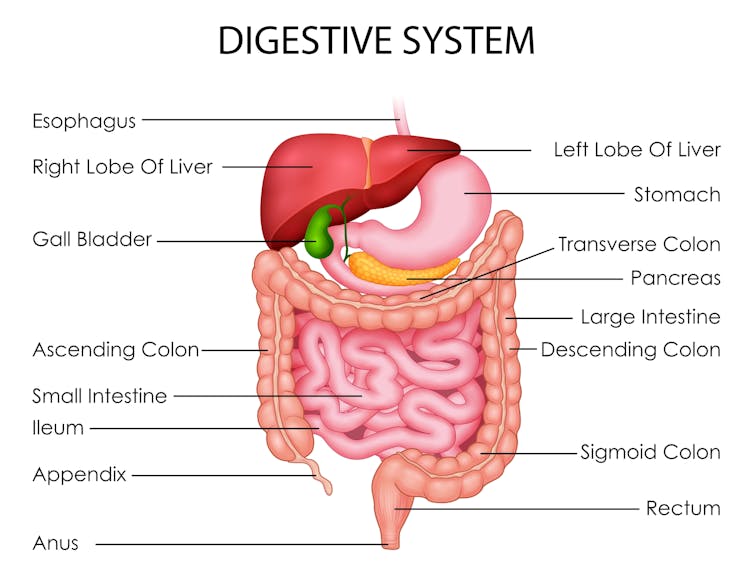
For healthy people, our internal clock means the muscular contractions in our colon follow a distinct rhythm.
There’s minimal activity in the night. The deeper and more restful our sleep, the fewer of these muscle contractions we have. It’s one reason why we don’t tend to poo in our sleep.
Your lower gut is a muscular tube that contracts more strongly at certain times of day. Vectomart/Shutterstock But there’s increasing activity during the day. Contractions in our colon are most active in the morning after waking up and after any meal.
One particular type of colon contraction partly controlled by our internal clock are known as “mass movements”. These are powerful contractions that push poo down to the rectum to prepare for the poo to be expelled from the body, but don’t always result in a bowel movement. In healthy people, these contractions occur a few times a day. They are more frequent in the morning than in the evening, and after meals.
Breakfast is also a trigger for us to poo. When we eat and drink our stomach stretches, which triggers the “gastrocolic reflex”. This reflex stimulates the colon to forcefully contract and can lead you to push existing poo in the colon out of the body. We know the gastrocolic reflex is strongest in the morning. So that explains why breakfast can be such a powerful trigger for a bowel motion.
Then there’s our morning coffee. This is a very powerful stimulant of contractions in the sigmoid colon (the last part of the colon before the rectum) and of the rectum itself. This leads to a bowel motion.
How important are morning poos?
Large international surveys show the vast majority of people will poo between three times a day and three times a week.
This still leaves a lot of people who don’t have regular bowel habits, are regular but poo at different frequencies, or who don’t always poo in the morning.
So if you’re healthy, it’s much more important that your bowel habits are comfortable and regular for you. Bowel motions do not have to occur once a day in the morning.
Morning poos are also not a good thing for everyone. Some people with irritable bowel syndrome feel the urgent need to poo in the morning – often several times after getting up, during and after breakfast. This can be quite distressing. It appears this early-morning rush to poo is due to overstimulation of colon contractions in the morning.
Can you train yourself to be regular?
Yes, for example, to help treat constipation using the gastrocolic reflex. Children and elderly people with constipation can use the toilet immediately after eating breakfast to relieve symptoms. And for adults with constipation, drinking coffee regularly can help stimulate the gut, particularly in the morning.
A disturbed circadian rhythm can also lead to irregular bowel motions and people more likely to poo in the evenings. So better sleep habits can not only help people get a better night’s sleep, it can help them get into a more regular bowel routine.
A regular morning coffee can help relieve constipation. Caterina Trimarchi/Shutterstock Regular physical activity and avoiding sitting down a lot are also important in stimulating bowel movements, particularly in people with constipation.
We know stress can contribute to irregular bowel habits. So minimising stress and focusing on relaxation can help bowel habits become more regular.
Fibre from fruits and vegetables also helps make bowel motions more regular.
Finally, ensuring adequate hydration helps minimise the chance of developing constipation, and helps make bowel motions more regular.
Monitoring your bowel habits
Most of us consider pooing in the morning to be regular. But there’s a wide variation in normal so don’t be concerned if your poos don’t follow this pattern. It’s more important your poos are comfortable and regular for you.
If there’s a major change in the regularity of your bowel habits that’s concerning you, see your GP. The reason might be as simple as a change in diet or starting a new medication.
But sometimes this can signify an important change in the health of your gut. So your GP may need to arrange further investigations, which could include blood tests or imaging.
Vincent Ho, Associate Professor and clinical academic gastroenterologist, Western Sydney University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
I’m iron deficient. Which supplements will work best for me and how should I take them?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Iron deficiency is common and can be debilitating. It mainly affects women. One in three premenopausal women are low in iron compared to just 5% of Australian men. Iron deficiency particularly affects teenage girls, women who do a lot of exercise and those who are pregnant.
The body needs iron to make new red blood cells, and to support energy production, the immune system and cognitive function. If you’re low, you may experience a range of symptoms including fatigue, weakness, shortness of breath, headache, irregular heartbeat and reduced concentration.
If a blood test shows you’re iron deficient, your doctor may recommend you start taking an oral iron supplement. But should you take a tablet or a liquid? With food or not? And when is the best time of day?
Here are some tips to help you work out how, when and what iron supplement to take.
LittlePigPower/Shutterstock How do I pick the right iron supplement?
The iron in your body is called “elemental iron”. Choosing the right oral supplement and dose will depend on how much elemental iron it has – your doctor will advise exactly how much you need.
The sweet spot is between 60-120 mg of elemental iron. Any less and the supplement won’t be effective in topping up your iron levels. Any higher and you risk gastrointestinal symptoms such as diarrhoea, cramping and stomach pain.
Low iron can especially affect people during pregnancy and women who do a lot of sport. Kamil Macniak/Shutterstock In Australia, iron salts are the most common oral supplements because they are cheap, effective and come in different delivery methods (tablets, capsules, liquid formulas). The iron salts you are most likely to find in your local chemist are ferrous sulfate (~20% elemental iron), ferrous gluconate (~12%) and ferrous fumarate (~33%).
These formulations all work similarly, so your choice should come down to dose and cost.
Many multivitamins may look like an iron supplement, but it’s important to note they usually have too little iron – usually less than 20 mg – to correct an iron deficiency.
Should I take tablets or liquid formulas?
Iron contained within a tablet is just as well absorbed as iron found in a liquid supplement. Choosing the right one usually comes down to personal preference.
The main difference is that liquid formulas tend to contain less iron than tablets. That means you might need to take more of the product to get the right dose, so using a liquid supplement could work out to be more expensive in the long term.
What should I eat with my iron supplement?
Research has shown you will absorb more of the iron in your supplement if you take it on an empty stomach. But this can cause more gastrointestinal issues, so might not be practical for everyone.
If you do take your supplement with meals, it’s important to think about what types of food will boost – rather than limit – iron absorption. For example, taking the supplement alongside vitamin C improves your body’s ability to absorb it.
Some supplements already contain vitamin C. Otherwise you could take the supplement along with a glass of orange juice, or other vitamin C-rich foods.
Taking your supplement alongside foods rich in vitamin C, like orange juice or kiwifruit, can help your body absorb the iron. Anete Lusina/Pexels On the other hand, tea, coffee and calcium all decrease the body’s ability to absorb iron. So you should try to limit these close to the time you take your supplement.
Should I take my supplement in the morning or evening?
The best time of day to take your supplement is in the morning. The body can absorb significantly more iron earlier in the day, when concentrations of hepcidin (the main hormone that regulates iron) are at their lowest.
Exercise also affects the hormone that regulates iron. That means taking your iron supplement after exercising can limit your ability to absorb it. Taking your supplement in the hours following exercise will mean significantly poorer absorption, especially if you take it between two and five hours after you stop.
Our research has shown if you exercise every day, the best time to take your supplement is in the morning before training, or immediately after (within 30 minutes).
My supplements are upsetting my stomach. What should I do?
If you experience gastrointestinal side effects such as diarrhoea or cramps when you take iron supplements, you may want to consider taking your supplement every second day, rather than daily.
Taking a supplement every day is still the fastest way to restore your iron levels. But a recent study has shown taking the same total dose can be just as effective when it’s taken on alternate days. For example, taking a supplement every day for three months works as well as every second day for six months. This results in fewer side effects.
Oral iron supplements can be a cheap and easy way to correct an iron deficiency. But ensuring you are taking the right product, under the right conditions, is crucial for their success.
It’s also important to check your iron levels prior to commencing iron supplementation and do so only under medical advice. In large amounts, iron can be toxic, so you don’t want to be consuming additional iron if your body doesn’t need it.
If you think you may be low on iron, talk to your GP to find out your best options.
Alannah McKay, Postdoctoral Research Fellow, Sports Nutrition, Australian Catholic University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Safe Effective Sleep Aids For Seniors
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Safe Efective Sleep Aids For Seniors
Choosing a safe, effective sleep aid can be difficult, especially as we get older. Take for example this research review, which practically says, when it comes to drugs, “Nope nope nope nope nope, definitely not, we don’t know, wow no, useful in one (1) circumstance only, definitely not, fine if you must”:
Review of Safety and Efficacy of Sleep Medicines in Older Adults
Let’s break it down…
What’s not so great
Tranquilizers aren’t very healthy ways to get to sleep, and are generally only well-used as a last resort. The most common of these are benzodiazepines, which is the general family of drugs with names usually ending in –azepam and –azolam.
Their downsides are many, but perhaps their biggest is their tendency to induce tolerance, dependence, and addiction.
Non-benzo hypnotics aren’t fabulous either. Z-drugs such as zolpidem tartrate (popularly known by the brand name Ambien, amongst others), comes with warnings that it shouldn’t be prescribed if you have sleep apnea (i.e., one of the most common causes of insomnia), and should be used only with caution in patients who have depression or are elderly, as it may cause protracted daytime sedation and/or ataxia.
See also: Benzodiazepine and z-drug withdrawal
(and here’s a user-friendly US-based resource for benzodiazepine addiction specifically)
Antihistamines are commonly sold as over-the-counter sleep aids, because they can cause drowsiness, but a) they often don’t b) they may reduce your immune response that you may actually need for something. They’re still a lot safer than tranquilizers, though.
What about cannabis products?
We wrote about some of the myths and realities of cannabis use yesterday, but it does have some medical uses beyond pain relief, and use as a sleep aid is one of them—but there’s another caveat.
How it works: CBD, and especially THC, reduces REM sleep, causing you to spend longer in deep sleep. Deep sleep is more restorative and restful. And, if part of your sleep problem was nightmares, they can only occur during REM sleep, so you’ll be skipping those, too. However, REM sleep is also necessary for good brain health, and missing too much of it will result in cognitive impairment.
Opting for a CBD product that doesn’t contain THC may improve sleep with less (in fact, no known) risk of long-term impairment.
See: Cannabis, Cannabinoids, and Sleep: a Review of the Literature
Melatonin: a powerful helper with a good safety profile
We did a main feature on this recently, so we won’t take up too much space here, but suffice it to say: melatonin is our body’s own natural sleep hormone, and our body is good at scrubbing it when we see white/blue light (so, look at such if you feel groggy upon awakening, and it should clear up quickly), so that and its very short elimination half-life again make it quite safe.
Unlike tranquilizers, we don’t develop a tolerance to it, let alone dependence or addiction, and unlike cannabis, it doesn’t produce long-term adverse effects (after all, our brains are supposed to have melatonin in them every night). You can read our previous main feature (including a link to get melatonin, if you want) here:
Melatonin: A Safe Natural Sleep Supplement
Herbal options: which really work?
Valerian? Probably not, but it seems safe to try. Data on this is very inconsistent, and many studies supporting it had poor methodology. Shinjyo et al. also hypothesized that the inconsistency may be due to the highly variable quality of the supplements, and lack of regulation, as they are provided “based on traditional use only”.
Chamomile? Given the fame of chamomile tea as a soothing, relaxing bedtime drink, there’s surprisingly little research out there for this specifically (as opposed to other medicinal features of chamomile, of which there are plenty).
But here’s one study that found it helped significantly:
The effects of chamomile extract on sleep quality among elderly people: A clinical trial
Unlike valerian, which is often sold as tablets, chamomile is most often sold as a herbal preparation for making chamomile tea, so the quality is probably quite consistent. You can also easily grow your own in most places!
Technological interventions
We may not have sci-fi style regeneration alcoves just yet, but white noise machines, or better yet, pink noise machines, help:
White Noise Is Good; Pink Noise Is Better
Note: the noise machine can be a literal physical device purchased to do that (most often sold as for babies, but babies aren’t the only ones who need to sleep!), but it can also just be your phone playing an appropriate audio file (there are apps available) or YouTube video.
We reviewed some sleep apps; you might like those too:
The Head-To-Head Of Google and Apple’s Top Apps For Getting Your Head Down
Enjoy, and rest well!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Olive oil is healthy. Turns out olive leaf extract may be good for us too
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Olive oil is synonymous with the Mediterranean diet, and the health benefits of both are well documented.
Olive oil reduces the risk of heart disease, cancer, diabetes and premature death. Olives also contain numerous healthy nutrients.
Now evidence is mounting about the health benefits of olive leaves, including from studies in a recent review.
Here’s what’s in olive leaves and who might benefit from taking olive leaf extract.
mtphoto19/Shutterstock What’s in olive leaves?
Olive leaves have traditionally been brewed as a tea in the Mediterranean and drunk to treat fever and malaria.
The leaves contain high levels of a type of antioxidant called oleuropein. Olives and olive oil contain this too, but at lower levels.
Generally, the greener the leaf (the less yellowish) the more oleuropein it contains. Leaves picked in spring also have higher levels compared to ones picked in autumn, indicating levels of oleuropein reduce as the leaves get older.
Olive leaves also contain other antioxidants such as hydroxytyrosol, luteolin, apigenin and verbascoside.
Antioxidants work by reducing the oxidative stress in the body. Oxidative stress causes damage to our DNA, cell membranes and tissues, which can lead to chronic diseases such as cancer and heart disease.
Are olive leaves healthy?
One review and analysis combined data from 12 experimental studies with 819 participants in total. Overall, olive leaf extract improved risk factors for heart disease. This included healthier blood lipids (fats) and lowering blood pressure.
The effect was greater for people who already had high blood pressure.
Most studies in this review gave olive leaf extract as a capsule, with daily doses of 500 milligrams to 5 grams for six to 48 weeks.
Another review and analysis published late last year looked at data from 12 experimental studies, with a total of 703 people. Some of these studies involved people with high blood lipids, people with high blood pressure, people who were overweight or obese, and some involved healthy people.
Daily doses were 250-1,000mg taken as tablets or baked into bread.
Individual studies in the review showed significant benefits in improving blood glucose (sugar) control, blood lipid levels and reducing blood pressure. But when all the data was combined, there were no significant health effects. We’ll explain why this may be the case shortly.
Olive leaves can be brewed into tea. Picture Partners/Shutterstock Another review looked at people who took oleuropein and hydroxytyrosol (the antioxidants in olive leaves). This found significant improvement in body weight, blood lipid profiles, glucose metabolism and improvements in bones, joints and cognitive function.
The individual studies included tested either the two antioxidants or olive leaf incorporated into foods such as bread and cooking oils (but not olive oil). The doses were 6-500mg per day of olive leaf extract.
So what can we make of these studies overall? They show olive leaf extract may help reduce blood pressure, improve blood lipids and help our bodies handle glucose.
But these studies show inconsistent results. This is likely due to differences in the way people took olive leaf extract, how much they took and how long for. This type of inconsistency normally tells us we need some more research to clarify the health effects of olive leaves.
Can you eat olive leaves?
Olive leaves can be brewed into a tea, or the leaves added to salads. Others report grinding olive leaves into smoothies.
However the leaves are bitter, because of the antioxidants, which can make them hard to eat, or the tea unpalatable.
Olive leaf extract has also been added to bread and other baked goods. Researchers find this improves the level of antioxidants in these products and people say the foods tasted better.
Olive leaves can taste bitter, which can put people off. But you can bake the extract into bread. Repina Valeriya/Shutterstock Is olive leaf extract toxic?
No, there seem to be no reported toxic effects of eating or drinking olive leaf extract.
It appears safe up to 1g a day, according to studies that have used olive leaf extract. However, there are no official guidelines about how much is safe to consume.
There have been reports of potential toxicity if taken over 85mg/kg of body weight per day. For an 80kg adult, this would mean 6.8g a day, well above the dose used in the studies mentioned in this article.
Pregnant and breastfeeding women are recommended not to consume it as we don’t know if it’s safe for them.
What should I do?
If you have high blood pressure, diabetes or raised blood lipids you may see some benefit from taking olive leaf extract. But it is important you discuss this with your doctor first and not change any medications or start taking olive leaf extract until you have spoken to them.
But there are plenty of antioxidants in all plant foods, and you should try to eat a wide variety of different coloured plant foods. This will allow you to get a range of nutrients and antioxidants.
Olive leaf and its extract is not going to be a panacea for your health if you’re not eating a healthy diet and following other health advice.
Evangeline Mantzioris, Program Director of Nutrition and Food Sciences, Accredited Practising Dietitian, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
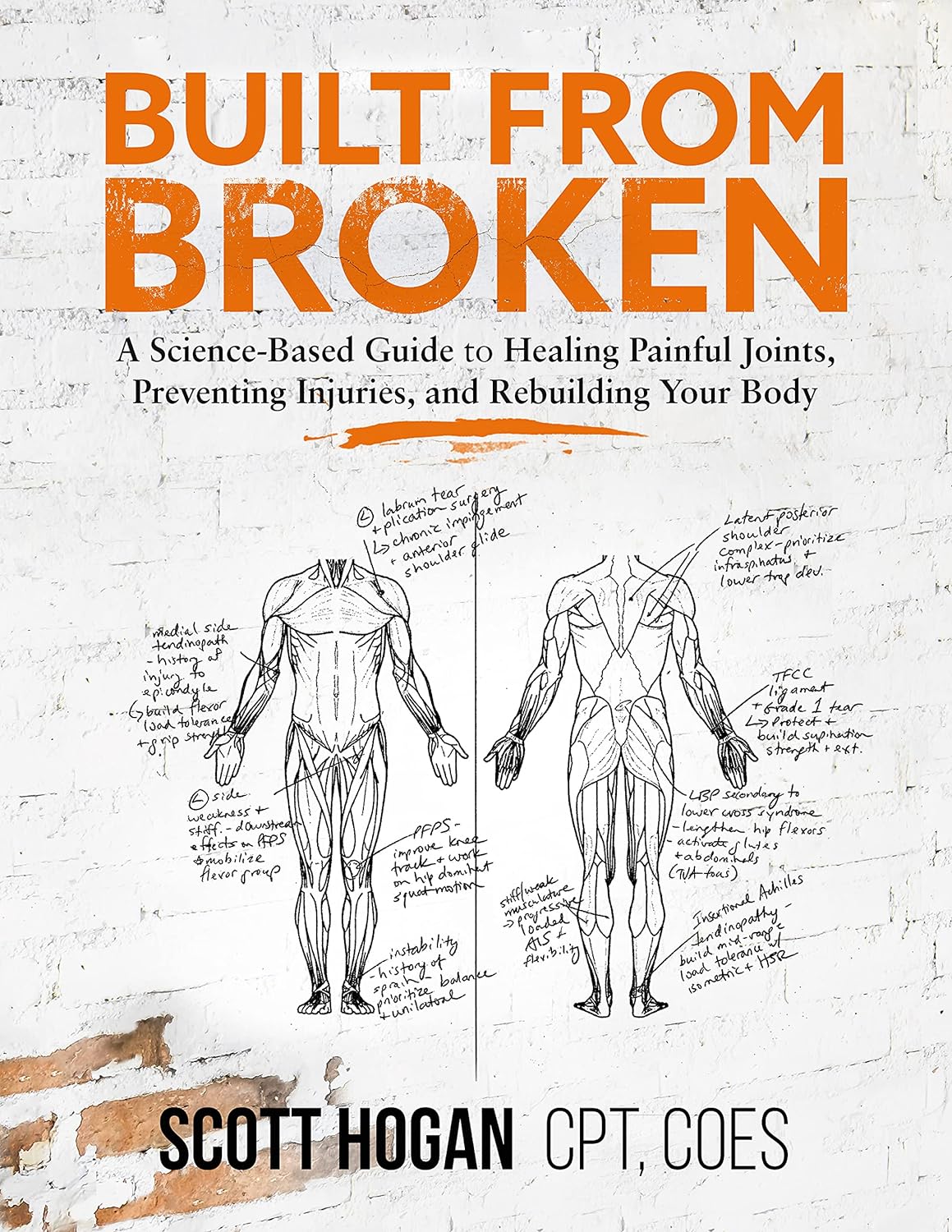
Built from Broken – by Scott Hogan, CPT, COES
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
So many exercise programs come with the caveat “consult your doctor before engaging in any new activity”, and the safe-but-simple “do not try to train through an injury”.
Which is all very well and good for someone in fabulous health who sprained an ankle while running and can just wait a bit, but what about those of us carrying…
- long-term injuries
- recurring injuries
- or just plain unfixable physical disabilities?
That’s where physiotherapist Scott Hogan comes in. The subtitle line goes:
❝A Science-Based Guide to Healing Painful Joints, Preventing Injuries, and Rebuilding Your Body❞
…but he does also recognize that there are some things that won’t bounce back.
On the other hand… There are a lot of things that get written off by doctors as “here’s some ibuprofen” that, with consistent mindful training, could actually be fixed.
Hogan delivers again and again in this latter category! You’ll see on Amazon that the book has thousands of 4- and 5-star ratings and many glowing reviews, and it’s for a reason or three:
- The book first lays a foundational knowledge of the most common injuries likely to impede us from training
- It goes on to give step-by-step corrective exercises to guide your body through healing itself. Your body is trying to heal itself anyway; you might as well help it accomplish that!
- It finishes up with a comprehensive (and essential) guide to train for the strength and mobility that will help you avoid future problems.
In short: a potentially life-changing book if you have some (likely back- or joint-related) problem that needs overcoming!
And if you don’t? An excellent pre-emptive guide all the same. This is definitely one of those “an ounce of prevention is better than a pound of cure” things.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: