Astaxanthin: Super-Antioxidant & Neuroprotectant
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Think Pink For Brain Health!
Astaxanthin is a carotenoid that’s found in:
- certain marine microalgae
- tiny crustaceans that eat the algae
- fish (and flamingos!) that eat the crustaceans
Yes, it’s the one that makes things pink.
But it does a lot more than that…
Super-antioxidant
Move over, green tea! Astaxanthin has higher antioxidant activity than most carotenoids. For example, it is 2–5 times more effective than alpha-carotene, lutein, beta-carotene, and lycopene:
Antioxidant activities of astaxanthin and related carotenoids
We can’t claim credit for naming it a super-antioxidant though, because:
Astaxanthin: A super antioxidant from microalgae and its therapeutic potential
Grow new brain cells
Axtaxanthin is a neuroprotectant, but that’s to be expected from something with such a powerful antioxidant ability.
What’s more special to astaxanthin is that it assists continued adult neurogenesis (creation of new brain cells):
❝The unique chemical structure of astaxanthin enables it to cross the blood-brain barrier and easily reach the brain, where it may positively influence adult neurogenesis.
Furthermore, astaxanthin appears to modulate neuroinflammation by suppressing the NF-κB pathway, reducing the production of pro-inflammatory cytokines, and limiting neuroinflammation associated with aging and chronic microglial activation.
By modulating these pathways, along with its potent antioxidant properties, astaxanthin may contribute to the restoration of a healthy neurogenic microenvironment, thereby preserving the activity of neurogenic niches during both normal and pathological aging. ❞
That first part is very important, by the way! There are so many things that our brain needs, and we can eat, but the molecules are unable to pass the blood-brain barrier, meaning they either get wasted, or used elsewhere, or dismantled for their constituent parts. In this case, it zips straight into the brain instead.
See also:
How To Grow New Brain Cells (At Any Age)
(Probably) good for the joints, too
First, astaxanthin got a glowing report in a study we knew not to trust blindly:
…and breathe. What a title that was! But, did you catch why it’s not to be trusted blindly? It was down at the bottom…
❝Conflict of interest statement
NOVAREX Co., Ltd. funded the study. Valensa International provided the FlexPro MD® ingredients, and NOVAREX Co., Ltd. encapsulated the test products (e.g., both FlexPro MD® and placebo)❞
Studies where a supplement company funded the study are not necessarily corrupt, but they can certainly sway publication bias, i.e. the company funds a bunch of studies and then pulls funding from the ones that aren’t going the way it wants.
So instead let’s look at:
Astaxanthin attenuates joint inflammation induced by monosodium urate crystals
and
Astaxanthin ameliorates cartilage damage in experimental osteoarthritis
…which had no such conflicts of interest.
They agree that astaxanthin indeed does the things (attenuates joint inflammation & ameliorates cartilage damage).
However, they are animal studies (rats), so we’d like to see studies with humans to be able to say for sure how much it helps these things.
Summary of benefits
Based on the available research, astaxanthin…
- is indeed a super-antioxidant
- is a neuroprotective agent
- also assists adult neurogenesis
- is probablygood for joints too
How much do I take, and is it safe?
A 2019 safety review concluded:
❝Recommended or approved doses varied in different countries and ranged between 2 and 24 mg.
We reviewed 87 human studies, none of which found safety concerns with natural astaxanthin supplementation, 35 with doses ≥12 mg/day.❞
Source: Astaxanthin: How much is too much? A safety review
In short: for most people, it’s very safe and well-tolerated. If you consume it to an extreme, you will likely turn pink, much as you would turn orange if you did the same thing with carrots. But aside from that, the risks appear to be minimal.
However! If you have a seafood allergy, please take care to get a supplement that’s made from microalgae, not one that’s made from krill or other crustaceans, or from other creatures that eat those.
Where can I get it?
We don’t sell it, but here’s an example product on Amazon, for your convenience
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Finish What You Start – by Peter Hollins
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For some people, getting started is the problem. For others of us, getting started is the easy part! We just need a little help not dropping things we started.
There are summaries at the starts and ends of sections, and many “quick tips” to get you back on track.
As a taster: one of these is “temptation bundling“, combining unpleasant things with pleasant. A kind of “spoonful of sugar” approach.
Hollins also discusses hyperbolic discounting (the way we tend to value rewards according to how near they are, and procrastinate accordingly). He offers a tool to overcome this, too, the “10–10–10 rule“.
Also dealt with is “the preparation trap“, and how to know when you have enough information to press on.
For a lot of us, the places we’re most likely to drop a project is 20% in (initial enthusiasm wore off) or 80% in (“it’s nearly done; no need to worry about it”). Those are the times when the advices in this book can be particularly handy!
All in all, a great book for seeing a lot of things to completion.
Share This Post
-
Half of Australians in aged care have depression. Psychological therapy could help
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
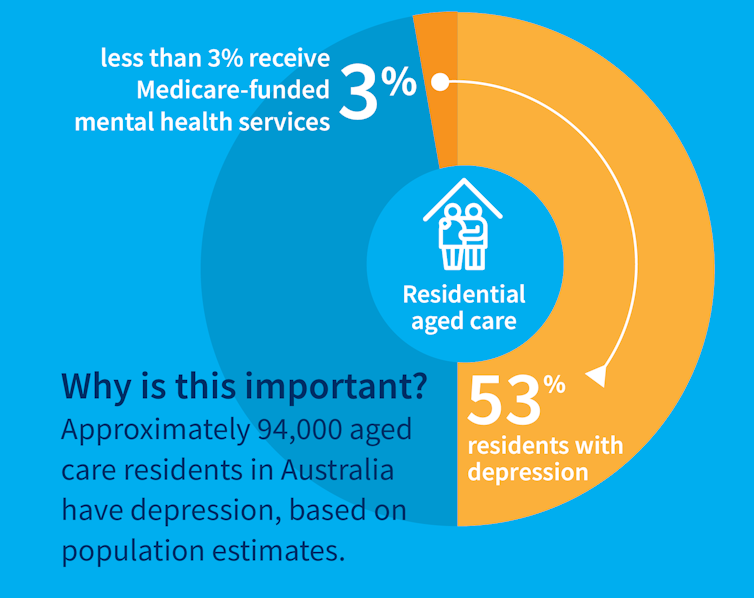
While many people maintain positive emotional wellbeing as they age, around half of older Australians living in residential aged care have significant levels of depression. Symptoms such as low mood, lack of interest or pleasure in life and difficulty sleeping are common.
Rates of depression in aged care appear to be increasing, and without adequate treatment, symptoms can be enduring and significantly impair older adults’ quality of life.
But only a minority of aged care residents with depression receive services specific to the condition. Less than 3% of Australian aged care residents access Medicare-subsidised mental health services, such as consultations with a psychologist or psychiatrist, each year.
Cochrane AustraliaInstead, residents are typically prescribed a medication by their GP to manage their mental health, which they often take for several months or years. A recent study found six in ten Australian aged care residents take antidepressants.
While antidepressant medications may help many people, we lack robust evidence on whether they work for aged care residents with depression. Researchers have described “serious limitations of the current standard of care” in reference to the widespread use of antidepressants to treat frail older people with depression.
Given this, we wanted to find out whether psychological therapies can help manage depression in this group. These treatments address factors contributing to people’s distress and provide them with skills to manage their symptoms and improve their day-to-day lives. But to date researchers, care providers and policy makers haven’t had clear information about their effectiveness for treating depression among older people in residential aged care.
The good news is the evidence we published today suggests psychological therapies may be an effective approach for people living in aged care.
We reviewed the evidence
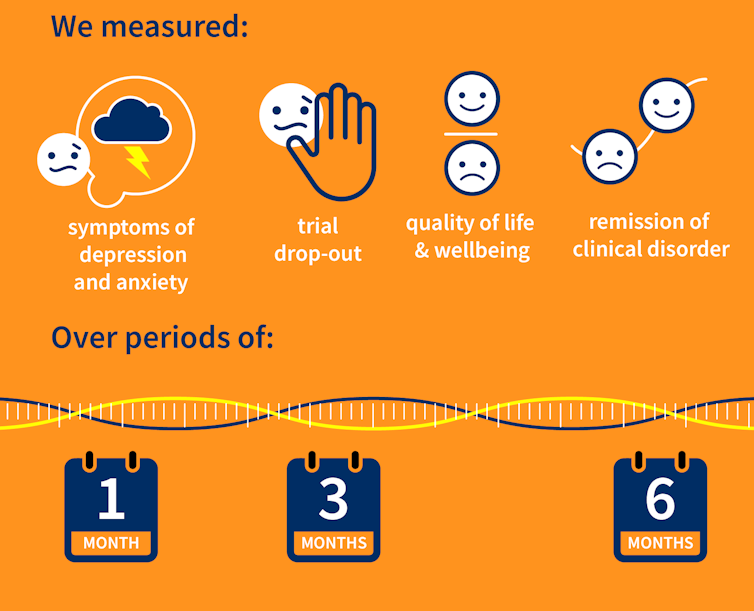
Our research team searched for randomised controlled trials published over the past 40 years that were designed to test the effectiveness of psychological therapies for depression among aged care residents 65 and over. We identified 19 trials from seven countries, including Australia, involving a total of 873 aged care residents with significant symptoms of depression.
The studies tested several different kinds of psychological therapies, which we classified as cognitive behavioural therapy (CBT), behaviour therapy or reminiscence therapy.
CBT involves teaching practical skills to help people re-frame negative thoughts and beliefs, while behaviour therapy aims to modify behaviour patterns by encouraging people with depression to engage in pleasurable and rewarding activities. Reminiscence therapy supports older people to reflect on positive or shared memories, and helps them find meaning in their life history.
The therapies were delivered by a range of professionals, including psychologists, social workers, occupational therapists and trainee therapists.
Cochrane AustraliaIn these studies, psychological therapies were compared to a control group where the older people did not receive psychological therapy. In most studies, this was “usual care” – the care typically provided to aged care residents, which may include access to antidepressants, scheduled activities and help with day-to-day tasks.
In some studies psychological therapy was compared to a situation where the older people received extra social contact, such as visits from a volunteer or joining in a discussion group.
What we found
Our results showed psychological therapies may be effective in reducing symptoms of depression for older people in residential aged care, compared with usual care, with effects lasting up to six months. While we didn’t see the same effect beyond six months, only two of the studies in our review followed people for this length of time, so the data was limited.
Our findings suggest these therapies may also improve quality of life and psychological wellbeing.
Psychological therapies mostly included between two and ten sessions, so the interventions were relatively brief. This is positive in terms of the potential feasibility of delivering psychological therapies at scale. The three different therapy types all appeared to be effective, compared to usual care.
However, we found psychological therapy may not be more effective than extra social contact in reducing symptoms of depression. Older people commonly feel bored, lonely and socially isolated in aged care. The activities on offer are often inadequate to meet their needs for stimulation and interest. So identifying ways to increase meaningful engagement day-to-day could improve the mental health and wellbeing of older people in aged care.
Some limitations
Many of the studies we found were of relatively poor quality, because of small sample sizes and potential risk of bias, for example. So we need more high-quality research to increase our confidence in the findings.
Many of the studies we reviewed were also old, and important gaps remain. For example, we are yet to understand the effectiveness of psychological therapies for people from diverse cultural or linguistic backgrounds.
Separately, we need better research to evaluate the effectiveness of antidepressants among aged care residents.
What needs to happen now?
Depression should not be considered a “normal” experience at this (or any other) stage of life, and those experiencing symptoms should have equal access to a range of effective treatments. The royal commission into aged care highlighted that Australians living in aged care don’t receive enough mental health support and called for this issue to be addressed.
While there have been some efforts to provide psychological services in residential aged care, the unmet need remains very high, and much more must be done.
The focus now needs to shift to how to implement psychological therapies in aged care, by increasing the competencies of the aged care workforce, training the next generation of psychologists to work in this setting, and funding these programs in a cost-effective way.
Tanya Davison, Adjunct professor, Health & Ageing Research Group, Swinburne University of Technology and Sunil Bhar, Professor of Clinical Psychology, Swinburne University of Technology
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Should I get a weighted vest to boost my fitness? And how heavy should it be?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Exercise training while wearing a weighted vest is undergoing somewhat of a renaissance. Social media posts and trainers are promoting them as a potential strategy for improving fitness and health.
Exercising with additional weight attached to the body is nothing new. This idea has been used with soldiers for many centuries if not millennia – think long hikes with a heavy pack.
The modern weighted vest comes in a range of designs that are more comfortable and can be adjusted in terms of the weight added. But could one be helpful for you?
ZR10/Shutterstock What the research says
One of the earliest research studies, reported in 1993, followed 36 older people wearing weighted vests during a weekly exercise class and at home over a 20-week period. Wear was associated with improvements in bone health, pain and physical function.
Since then, dozens of papers have evaluated the exercise effects of wearing a weighted vest, reporting a range of benefits.
Not surprisingly, exercise with a weighted vest increases physiological stress – or how hard the body has to work – as shown by increased oxygen uptake, heart rate, carbohydrate utilisation and energy expenditure.
Adding weight equal to 10% of body weight is effective. But it doesn’t appear the body works significantly harder when wearing 5% extra weight compared to body weight alone.
Does more load mean greater injury risk?
A small 2021 study suggested additional weights don’t alter the biomechanics of walking or running. These are important considerations for lower-limb injury risk.
The safety considerations of exercising with weighted vests have also been reported in a biomechanical study of treadmill running with added weight of 1% to 10% of body weight.
While physiological demand (indicated by heart rate) was higher with additional weight and the muscular forces greater, running motion was not negatively affected.
To date no research studies have reported increased injuries due to wearing weighted vests for recreational exercise. However a 2018 clinical study on weight loss in people with obesity found back pain in 25% of those wearing such vests. Whether this can be translated to recreational use in people who don’t have obesity is difficult to say. As always, if pain or discomfort is experienced then you should reduce the weight or stop vest training.
Better for weight loss or bone health?
While wearing a weighted vest increases the energy expenditure of aerobic and resistance exercise, research to show it leads to greater fat loss or retaining muscle mass is somewhat inconclusive.
One older study investigated treadmill walking for 30 minutes, three times a week in postmenopausal women with osteoporosis. The researchers found greater fat loss and muscle gain in the participants who wore a weighted vest (at 4–8% body weight). But subsequent research in obese older adults could not show greater fat loss in participants who wore weighted vests for an average of 6.7 hours per day.
There has been considerable interest in the use of weighted vests to improve bone health in older people. One 2003 study reported significant improvements in bone density in a group of older women over 32 weeks of weighted vest walking and strength training compared to a sedentary control group.
But a 2012 study found no difference in bone metabolism between groups of postmenopausal women with osteoporosis walking on a treadmill with or without a weighted vest.
Making progress
As with any exercise, there is a risk of injury if it is not done correctly. But the risk of weighted vest training appears low and can be managed with appropriate exercise progression and technique.
If you are new to training, then the priority should be to simply start exercising and not complicate it with wearing a weighted vest. The use of body weight alone will be sufficient to get you on the path to considerable gains in fitness.
Once you have a good foundation of strength, aerobic fitness and resilience for muscles, joints and bones, using a weighted vest could provide greater loading intensity as well as variation.
It is important to start with a lighter weight (such as 5% bodyweight) and build to no more than 10% body weight for ground impact exercises such as running, jogging or walking.
For resistance training such as squats, push-ups or chin-ups, progression can be achieved by increasing loads and adjusting the number of repetitions for each set to around 10 to 15. So, heavier loads but fewer repetitions, then building up to increase the load over time.
While weighted vests can be used for resistance training, it is probably easier and more convenient to use barbells, dumbbells, kettle bells or weighted bags.
The benefits of added weight can also be achieved by adding repetition or duration. Geert Pieters/Unsplash The bottom line
Weighted vest training is just one tool in an absolute plethora of equipment, techniques and systems. Yes, walking or jogging with around 10% extra body weight increases energy expenditure and intensity. But training for a little bit longer or at a higher intensity can achieve similar results.
There may be benefits for bone health in wearing a weighted vest during ground-based exercise such as walking or jogging. But similar or greater stimulus to bone growth can be achieved by resistance training or even the introduction of impact training such as hopping, skipping or bounding.
Exercising with a weighted vest likely won’t increase your injury risk. But it must be approached intelligently considering fitness level, existing and previous injuries, and appropriate progression for intensity and repetition.
Rob Newton, Professor of Exercise Medicine, Edith Cowan University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Becoming a Supple Leopard – by Dr. Kelly Starrett and Glen Cordoza
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed Dr. Starrett’s other book, “Built To Move“, and now today we’ll review his more famous book!
Why is this one so famous? It’s popularly considered “the Bible of Cross-Fit”, even though it’s not at all marketed as such, and nor does it talk about Cross Fit directly. But: people who are interested in being fit, fast, strong, mobile, stable, and so forth, tend to invest in this book at some point if they are serious.
The book is big, heavy, and textbook-like. This isn’t a quick light read. This is a “study over the course of a year or more while doing your physiotherapy degree” book. And yet, it’s written for the widest audience, and as such, everything is explained from the ground up, so no prior knowledge is expected.
It does have pictures, which are clear and helpful, though the print version is better for this than the Kindle edition.
The subtitle of the book is no lie; it does indeed cover all those things, deeply and at length, for everything musculoskeletal.
Bottom line: this book will seriously improve your knowledge and understanding of all things body mechanics and related body maintenance. If you care to get/remain fit/strong/mobile/etc, this book is a fine cornerstone for such endeavors.
Click here to check out Becoming A Supple Leopard, and become a supple leopard!*
*Metaphorically. Furry metamorphosis is not a side-effect. Suppleness, however, is on offer. Yes, even for you, dear reader!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Secret Easy Tips to Loosen Your Hips In 10 Minutes
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Stiff hips can often cause discomfort, and ultimately back pain because of how one thing relies on the other as its seat. However, there are ways to improve it without taking years to get to where you want to be:
One bit at a time
Warm up and massage:
- Massage the front and back of the thighs to loosen tight muscles.
- Use your body weight for effective massaging.
- Relax and breathe slowly while massaging.
Vary your stretches:
- Perform a seated butterfly stretch, but avoid overexertion.
- Move knees gently within a comfortable range of motion.
- Perform stretches like placing one foot on the opposite knee or holding legs to open hips.
- Stretch the hips while lying on the floor with bent knees.
And now for the “magic move”: lie on your stomach, bend one knee, and gently rock to loosen hip stiffness.
Generally speaking, for most stretches one can usually stretch further on one side at once, than both at the same time. So, leverage this in your flexibility training, to get each side of your body accustomed to going that bit further. Then, when your body is comfortable with that, put it together.
For more on all of this plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
How Tight Are Your Hips? Test (And Fix!) With This
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Power of Self-Care – by Dr. Sunil Kumar
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this book is mostly not about: bubble baths and scented candles. We say “mostly”, because stress management is an important aspect given worthy treatment in this book, but there is more emphasis on evidence-based interventions and thus Dr. Kumar is readier to prescribe nature walks and meditation, than product-based pampering sessions.
As is made clear in the subtitle “Transforming Heart Health with Lifestyle Medicine”, the focus is on heart health throughout, but as 10almonds readers know, “what’s good for your heart is good for your brain” is a truism that indeed holds true here too.
Dr. Kumar also gives nutritional tweaks to optimize heart health, and includes a selection of heart-healthy recipes, too. And exercise? Yes, customizable exercise plans, even. And a plan for getting sleep into order if perchance it has got a bit out of hand (most people get less sleep than necessary for maintenance of good health), and he even delves into “social prescribing”, that is to say, making sure that one’s social connectedness does not get neglected—without letting it, conversely, take over too much of one’s life (done badly, social connectedness can be a big source of unmanaged stress).
Perhaps the most value of this book comes from its 10-week self-care plan (again, with a focus on heart health), basically taking the reader by the hand for long enough that, after those 10 weeks, habits should be quite well-ingrained.
A strong idea throughout is that the things we take up should be sustainable, because well, a heart is for life, not just for a weekend retreat.
Bottom line: if you’d like to improve your heart health in a way that feels like self-care rather than an undue amount of work, then this is the book for you.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: