The Fascinating Truth About Aspartame, Cancer, & Neurotoxicity
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Is Aspartame’s Reputation Well-Deserved?
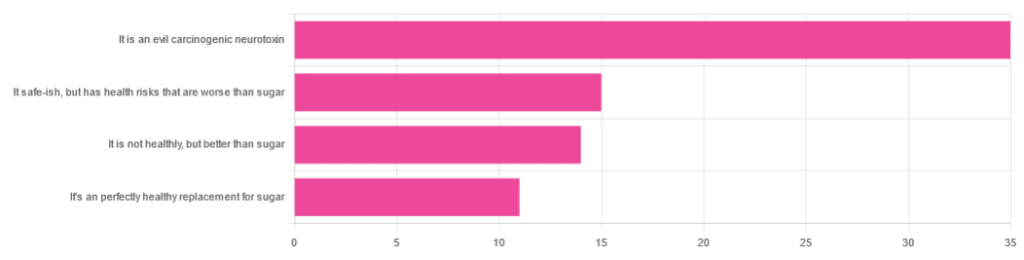
In Tuesday’s newsletter, we asked you for your health-related opinions on aspartame, and got the above-depicted, below-described, set of responses:
- About 47% said “It is an evil carcinogenic neurotoxin”
- 20% said “It is safe-ish, but has health risks that are worse than sugar”
- About 19% said “It is not healthy, but better than sugar”
- About 15% said “It’s a perfectly healthy replacement for sugar”
But what does the science say?
Aspartame is carcinogenic: True or False?
False, assuming consuming it in moderation. In excess, almost anything can cause cancer (oxygen is a fine example). But for all meaningful purposes, aspartame does not appear to be carcinogenic. For example,
❝The results of these studies showed no evidence that these sweeteners cause cancer or other harms in people.❞
~ NIH | National Cancer Institute
Source: Artificial Sweeteners and Cancer
Plenty of studies and reviews have also confirmed this; here are some examples:
- Evaluation of aspartame cancer epidemiology studies based on quality appraisal criteria
- Aspartame, low-calorie sweeteners and disease: Regulatory safety and epidemiological issues
- Aspartame: A review of genotoxicity data
Why then do so many people believe it causes cancer, despite all the evidence against it?
Well, there was a small study involving giving megadoses to rats, which did increase their cancer risk. So of course, the popular press took that and ran with it.
But those results have not been achieved outside of rats, and human studies great and small have all been overwhelmingly conclusive that moderate consumption of aspartame has no effect on cancer risk.
Aspartame is a neurotoxin: True or False?
False, again assuming moderate consumption. If you’re a rat being injected with a megadose, your experience may vary. But a human enjoying a diet soda, the aspartame isn’t the part that’s doing you harm, so far as we know.
For example, the European Food Safety Agency’s scientific review panel concluded:
❝there is still no substantive evidence that aspartame can induce such effects❞
~ Dr. Atkin et al (it was a pan-European team of 21 experts in the field)
Source: Report on the Meeting on Aspartame with National Experts
See also,
❝The data from the extensive investigations into the possibility of neurotoxic effects of aspartame, in general, do not support the hypothesis that aspartame in the human diet will affect nervous system function, learning or behavior.
The weight of existing evidence is that aspartame is safe at current levels of consumption as a nonnutritive sweetener.❞
and
❝The safety testing of aspartame has gone well beyond that required to evaluate the safety of a food additive.
When all the research on aspartame, including evaluations in both the premarketing and postmarketing periods, is examined as a whole, it is clear that aspartame is safe, and there are no unresolved questions regarding its safety under conditions of intended use.❞
Source: Regulatory Toxicology & Pharmacology | Aspartame: Review of Safety
Why then do many people believe it is a neurotoxin? This one can be traced back to a chain letter hoax from about 26 years ago; you can read it here, but please be aware it is an entirely debunked hoax:
Urban Legends | Aspartame Hoax
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Most Anti Aging Exercise
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve referenced this (excellent) video before, but never actually put it under the spotlight in one of these features, so here we go!
Deep squats
It’s about deep squats, also called Slav squats, Asian squats, sitting squats, resting squats, or various other names. However, fear not; you don’t need to be Slavic or Asian to do it; you just need to practice.
As for why this is called “anti-aging”, by the way, it’s because being able to get up off the ground is one of the main tests of age-related mobility decline, and if you can deep-squat comfortably, then you can do that easily. And so long as you continue being able to deep-squat comfortably, you’ll continue to be able to get up off the ground easily too, because you have the strength in the right muscles, as well as the suppleness, comfort with range of motion, and balance (those stabilizing muscles are used constantly in a deep squat, whereas Western lifestyle sitting leaves those muscles very neglected and thus atrophied).
Epidemiological note: chairs, couches, and assorted modern conveniences reduce the need for squatting in daily life, leading to stiffness in joints, muscles, tendons, and ligaments. Many adults in developed countries struggle with deep squats due to lack of use, not aging. Which is a problem, because a lack of full range of motion in joints causes wear and tear, leading to chronic pain and degenerative joint diseases. People in countries where squatting is a common resting position have lower incidences of osteoarthritis, for example—contrary to what some might expect, squatting does not harm joints but rather protects them from arthritis and knee pain. Strengthening leg muscles through squatting can alleviate knee pain, whereas knee pain is often worsened by inactivity.
Notwithstanding the thumbnail, which is showing an interim position, one’s feet should be flat on the ground, by the way, and one’s butt should be nearby, just a few inches off the ground (in other words, the position that we see her in for most of this video).
Troubleshooting: if you’re accustomed to sitting in chairs a lot, then this may be uncomfortable at first. Zuzka advises us to go gently, and/but gradually increase our range of motion and (equally importantly) duration in the resting position.
You can use a wall or doorway to partially support you, at first, if you struggle with mobility or balance. Just try to gradually use it less, until you’re comfortable deep-squatting with no support.
Since this is not an intrinsically very exciting exercise, once you build up the duration for which you’re comfortable deep-squatting, it can be good to get in the habit of “sitting” this way (i.e. deep squatting, still butt-off-the-floor, but doing the job of sitting) while doing other things such as working (if you have an appropriate work set-up for that*), reading, or watching TV.
*this is probably easiest with a laptop placed on an object/surface of appropriate height, such as a coffee table or such. As a bonus, having your hands in front of you while working will also bring your center of gravity forwards a bit, making the position easier and more comfortable to maintain. This writer (hi, it’s me) prefers her standing desk for work in general, with a nice ergonomic keyboard and all that, but if using a laptop from time to time, then squatting is a very good option.
In terms of working up duration, if you can only manage seconds to start with, that’s fine. Just do a few more seconds each time, until it’s 30, 60, 120, and so on until it’s 5 minutes, 10, 15, and so on.
You can even start that habit-forming while you’re still in the “seconds at a time” stage! You can deep-squat just for some seconds while you:
- pick up something from the floor
- check on something in the oven
- get something out of the bottom of the fridge
…etc!
For more on all this, plus many visual demonstrations including interim exercises to get you there if it’s difficult for you at first, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Mobility For Now & For Later: Train For The Marathon That Is Your Life!
Take care!
Share This Post
-
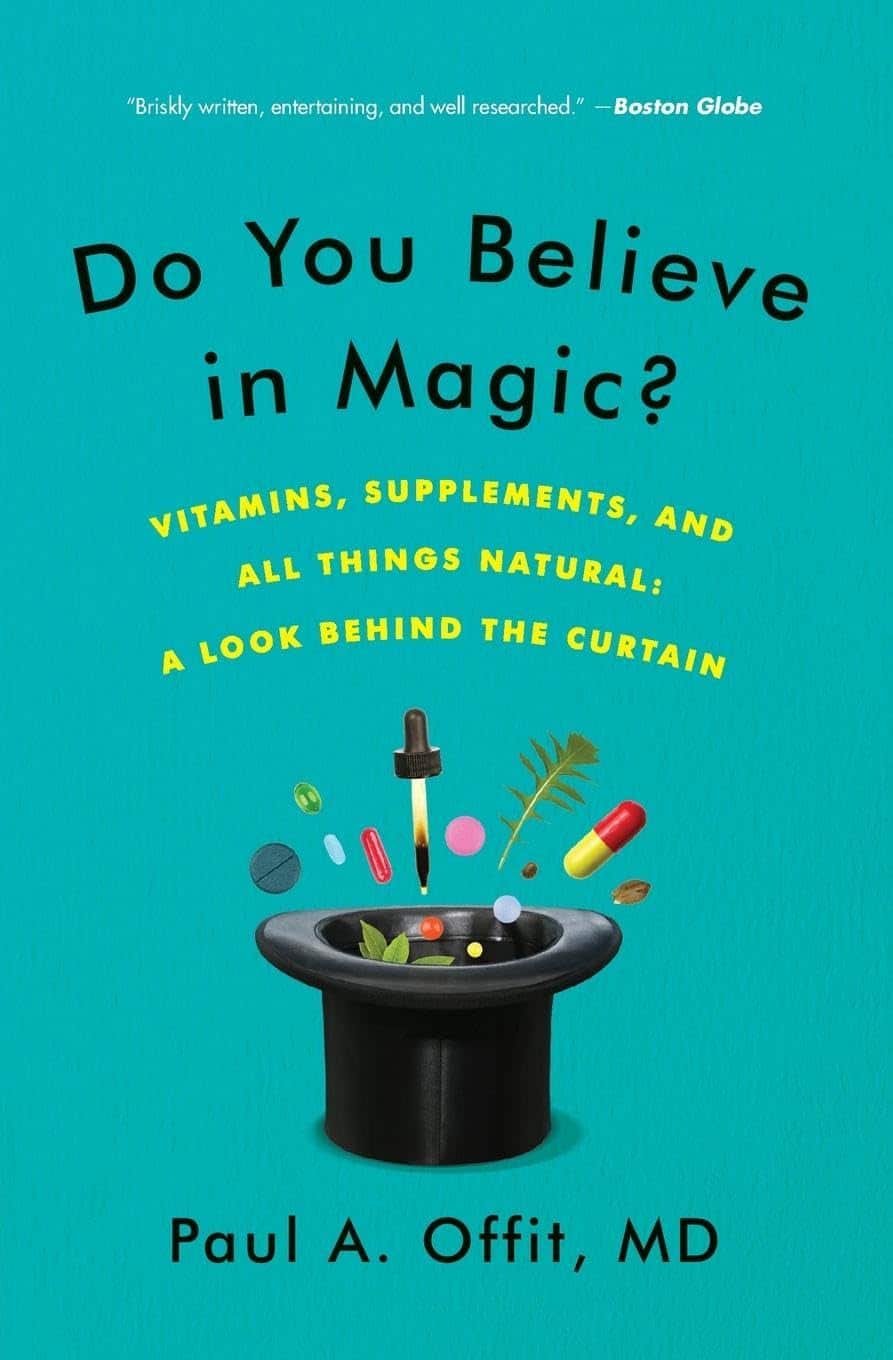
Do You Believe In Magic? – by Dr. Paul Offit
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Here at 10almonds, we like to examine and present the science wherever it leads, so this book was an interesting read.
Dr. Offit, himself a much-decorated vaccine research scientist, and longtime enemy of the anti-vax crowd, takes aim at alternative therapies in general, looking at what does work (and how), and what doesn’t (and what harm it can cause).
The style of the book is largely polemic in tone, but there’s lots of well-qualified information and stats in here too. And certainly, if there are alternative therapies you’ve left unquestioned, this book will probably prompt questions, at the very least.
And science, of course, is about asking questions, and shouldn’t be afraid of such! Open-minded skepticism is a key starting point, while being unafraid to actually reach a conclusion of “this is probably [not] so”, when and if that’s where the evidence brings us. Then, question again when and if new evidence comes along.
To that end, Dr. Offit does an enthusiastic job of looking for answers, and presenting what he finds.
If the book has downsides, they are primarily twofold:
- He is a little quick to dismiss the benefits of a good healthy diet, supplemented or otherwise.
- His keenness here seems to step from a desire to ensure people don’t skip life-saving medical treatments in the hope that their diet will cure their cancer (or liver disease, or be it what it may), but in doing so, he throws out a lot of actually good science.
- He—strangely—lumps menopausal HRT in with alternative therapies, and does the exact same kind of anti-science scaremongering that he rails against in the rest of the book.
- In his defence, this book was published ten years ago, and he may have been influenced by a stack of headlines at the time, and a popular celebrity endorsement of HRT, which likely put him off it.
Bottom line: there’s something here to annoy everyone—which makes for stimulating reading.
Click here to check out Do You Believe In Magic, and expand your knowledge!
Share This Post
- He is a little quick to dismiss the benefits of a good healthy diet, supplemented or otherwise.
-
Instant Quiz Results, No Email Needed
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
❓ Q&A With 10almonds Subscribers!
Q: I like that the quizzes (I’ve done two so far) give immediate results , with no “give us your email to get your results”. Thanks!
A: You’re welcome! That’s one of the factors that influences what things we include here! Our mission statement is “to make health and productivity crazy simple”, and the unwritten part of that is making sure to save your time and energy wherever we reasonably can!
Share This Post
Related Posts
-
When Doctors Make House Calls, Modern-Style!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
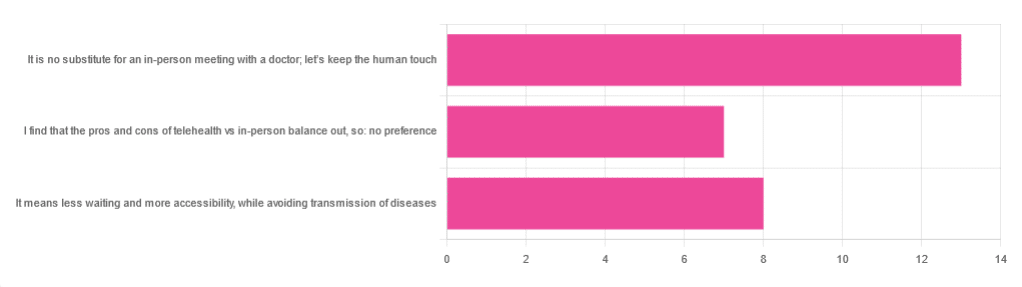
In Tuesday’s newsletter, we asked you foryour opinion of telehealth for primary care consultations*, and got the above-depicted, below-described, set of responses:
- About 46% said “It is no substitute for an in-person meeting with a doctor; let’s keep the human touch”
- About 29% said “It means less waiting and more accessibility, while avoiding transmission of diseases”
- And 25 % said “I find that the pros and cons of telehealth vs in-person balance out, so: no preference”
*We specified that by “primary care” we mean the initial consultation with a non-specialist doctor, before receiving treatment or being referred to a specialist. By “telehealth” we mean by videocall or phonecall.
So, what does the science say?
A quick note first
Because telehealth was barely a thing (statistically speaking) before the first stages of the COVID pandemic, compared to how it is now, most of the science for this is young, and a lot of the science simply hasn’t been done yet, and/or has not been published yet, because the process can take years.
Because of this, some studies we do have aren’t specifically about primary care, and are sometimes about specialists. We think this should not affect the results much, but it bears highlighting.
Nevertheless, we’ll do what we can with the science we have!
Telehealth is more accessible than in-person consultations: True or False?
True, for most people. For example…
❝Data was found from a variety of emergency and non-emergency departments of primary, secondary, and specialised healthcare.
Satisfaction was high among recipients of healthcare, scoring 9-10 on a scale of 0-10 or ranging from 73.3% to 100%.
Convenience was rated high in every specialty examined. Satisfaction of clinicians was high throughout the specialities despite connection failure and concerns about confidentiality of information.❞
whereas…
❝Nonetheless, studies reported perception of increased barriers to accessing care and inequalities for vulnerable patients especially in older people❞
~ Ibid.
Source: Satisfaction with telemedicine use during COVID-19 pandemic in the UK: a systematic review
Now, perception of those things does necessarily equate to an actual increased barrier, but it is reasonable that someone who thinks something is inaccessible will be less inclined to try to access it.
The quality of care provided via telehealth is as good as in-person: True or False?
True, ostensibly, with caveats. The caveats are:
- We’re going offreported patient satisfaction, not objective patient health outcomes (we found little* science as yet for the relative incidence of misdiagnosis, for example—which kind of thing will take time to be revealed).
- We’re also therefore speaking (as statistics do) for the significant majority of people. However, if we happen to be (statistically speaking) an insignificant minority, well, that just sucks for us personally.
*we did find some, but it wasn’t very helpful yet. For example:
An electronic trigger to detect telemedicine-related diagnostic errors
this one does look at the incidence of diagnostic errors, but provides no control group (i.e. otherwise-comparable in-person consultations) for comparison.
While most oft-considered demographic groups reported comparable patient satisfaction (per race, gender, and socioeconomic status, for example), there was one outlier variable, which was age (as we quoted from that first study above).
However!
Looking under the hood of these stats, it seems that age is not the real culprit, so much as technological illiteracy, which is heavily correlated with age:
❝Lower eHealth literacy is associated with more negative attitudes towards I/C technology in healthcare. This trend is consistent across diverse demographics and regions. ❞
Source: Meta-analysis: eHealth literacy and attitudes towards internet/computer technology
There are things that can be done at an in-person consultation that can’t be done by telehealth: True or False?
True, of course. It is incredibly rare that we will cite “common sense”, (as sometimes “common sense” is actually “common mistakes” and is simply and verifiably wrong), but in this case, as one 10almonds subscriber put it:
❝The doctor uses his five senses to assess. This cannot be attained over the phone❞
~ 10almonds subscriber
A quick note first: if your doctor is using their sense of taste to diagnose you, please get a different doctor, because they should definitely not be doing that!
Not in this century, anyway… Once upon a time, diabetes was diagnosed by urine-tasting (and yes, that was a fairly reliable method).
However, nowadays indeed a doctor will use sight, sound, touch, and sometimes even smell.
In a videocall we’re down to two of those senses (sight and sound), and in a phonecall, down to one (sound) and even that is hampered. Your doctor cannot, for example, use a stethoscope over the phone.
With this in mind, it really comes down to what you need from your doctor in that consultation.
- If you’re 99% sure that what you need is to be prescribed an antidepressant, that probably doesn’t need a full physical.
- If you’re 99% sure that what you need is a referral, chances are that’ll be fine by telehealth too.
- If your doctor is 99% sure that what you need is a verbal check-up (e.g. “How’s it been going for you, with the medication that I prescribed for you a month ago?”, then again, a call is probably fine.
If you have a worrying lump, or an unhappy bodily discharge, or an unexplained mysterious pain? These things, more likely an in-person check-up is in order.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Keep Your Mind From Wandering
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Whether your mind keeps wandering more as you get older, or you’re a young student whose super-active brain is more suited to TikTok than your assigned reading, sustained singular focus can be a challenge for everyone—and yet (alas!) it remains a required skill for so much in life.
Today’s edition of 10Almonds presents a nifty trick to get yourself through those tasks! We’ll also be taking some time to reply to your questions and comments, in our weekly interactive Q&A.
First of all though, we’ve a promise to make good on, so…
How To Stay On The Ball (Or The Tomato?) The Easy Way
For most of us, we face three main problems when it comes to tackling our to-dos:
- Where to start?
- The task seems intimidating in its size
- We get distracted and/or run out of energy
If you’re really not sure where to start, we recommended a powerful tool in last Friday’s newsletter!
For the rest, we love the Pomodoro Technique:
- Set a timer for 25 minutes, and begin your task.
- Keep going until the timer is done! No other tasks, just focus.
- Take a 5-minute break.
- Repeat
This approach has three clear benefits:
- No matter the size of the task, you are only committing to 25 minutes—everything is much less overwhelming when there’s an end in sight!
- Being only 25 minutes means we are much more likely to stay on track; it’s easier to defer other activities if we know that there will be a 5-minute break for that soon.
- Even without other tasks to distract us, it can be difficult to sustain attention for long periods; making it only 25 minutes at a time allows us to approach it with a (relatively!) fresh mind.
Have you heard that a human brain can sustain attention for only about 40 minutes before focus starts to decline rapidly?
While that’s been a popular rationale for school classroom lesson durations (and perhaps coincidentally ties in with Zoom’s 40-minute limit for free meetings), the truth is that focus starts dropping immediately, to the point that one-minute attention tests are considered sufficient to measure the ability to focus.
So a 25-minute Pomodoro is a more than fair compromise!
Why’s it called the “Pomodoro” technique?
And why is the 25-minute timed work period called a Pomodoro?
It’s because back in the 80s, university student Francesco Cirillo was struggling to focus and made a deal with himself to focus just for a short burst at a time—and he used a (now “retro” style) kitchen timer in the shape of a tomato, or “pomodoro”, in Italian.
If you don’t have a penchant for kitsch kitchenware, you can use this free, simple Online Pomodoro Timer!
(no registration/login/download necessary; it’s all right there on the web page)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Train For The Event Of Your Life!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Mobility As A Sporting Pursuit
As we get older, it becomes increasingly important to treat life like a sporting event. By this we mean:
As an “athlete of life”, there are always events coming up for which we need to train. Many of these events will be surprise tests!
Such events/tests might include:
- Not slipping in the shower and breaking a hip (or worse)
- Reaching an item from a high shelf without tearing a ligament
- Getting out of the car at an awkward angle without popping a vertebra
- Climbing stairs without passing out light-headed at the top
- Descending stairs without making it a sled-ride-without-a-sled
…and many more.
Train for these athletic events now
Not necessarily this very second; we appreciate you finishing reading first. But, now generally in your life, not after the first time you fail such a test; it can (and if we’re not attentive: will) indeed happen to us all.
With regard to falling, you might like to revisit our…
…which covers how to not fall, and to not injure yourself if you do.
You’ll also want to be able to keep control of your legs (without them buckling) all the way between standing and being on the ground.
Slav squats or sitting squats (same exercise, different names, amongst others) are great for building and maintaining this kind of strength and suppleness:
(Click here for a refresher if you haven’t recently seen Zuzka’s excellent video explaining how to do this, especially if it’s initially difficult for you, “The Most Anti-Aging Exercise”)
this exercise is, by the way, great for pretty much everything below the waist!
You will also want to do resistance exercises to keep your body robust:
Resistance Is Useful! (Especially As We Get Older)
And as for those shoulders? If it is convenient for you to go swimming, then backstroke is awesome for increasing and maintaining shoulder mobility (and strength).
If swimming isn’t a viable option for you, then doing the same motion with your arms, while standing, will build the same flexibility. If you do it while holding a small weight (even just 1kg is fine, but feel free to increase if you so wish and safely can) in each hand will build the necessary strength as you go too.
As for why even just 1kg is fine: read on
About that “and strength”, by the way…
Stretching is not everything. Stretching is great, but mobility without strength (in that joint!) is just asking for dislocation.
You don’t have to be built like the Terminator, but you do need to have the structural integrity to move your body and then a little bit more weight than that (or else any extra physical work could be enough to tip you to breaking point) without incurring damage from the strain. So, it needs to not be a strain! See again, the aforementioned resistance exercises.
That said, even very gentle exercise helps too; see for example the impact of walking on osteoporosis:
Living near green spaces linked to higher bone density and lower osteoporosis risk
and…
So you don’t have to run marathons—although you can if you want:
Marathons in Mid- and Later-Life
…to keep your hips and more in good order.
Want to test yourself now?
Check out:
Building & Maintaining Mobility
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: