Are You Making This Alcohol Mistake?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The famous “small glass of red per day” is, as is quite well-established now in science, but not so much in popular culture, known to be not a good idea.
What most people don’t know
Rethinking “One Drink a Day”:
- Outdated beliefs and flawed studies:
- The idea that “one drink a day is healthy” stems from flawed associative studies that included…
- unhealthy former heavy drinkers in the zero-drinks category, and
- healthy older individuals who continued light drinking due to good health, not because alcohol contributed to it, in the drinkers category
- In other words, they looked at former alcoholics whose health was ruined by drinking and said “aha, non-drinkers have bad health”, and looked at the survivors of survivorship bias and said “aha, light drinking is the key to good health”. Which of course is terrible science propped up by terrible abuse of statistics propped up by shoddy methodology.
- The idea that “one drink a day is healthy” stems from flawed associative studies that included…
- New research findings:
- A 2022 UK Biobank Study showed that even one drink a day leads to brain shrinkage, neuron death, and cognitive decline.
- Another study on CVD disproved the notion that light drinking benefits heart health once confounding variables were removed.
- There are plenty more, and at 10almonds we’ve done a main feature about it, but for now, you get the idea.
Some other things you should know:
Ethanol and acetaldehyde damage neurons responsible for impulse control, judgment, motor coordination, and memory formation, leading to cognitive decline. The feeling of being drunk results from the suppression and damage of these neurons. But while the drunk feeling wears off, the damage to neurons does not.
Alcohol causes cumulative DNA damage in neurons, accelerates brain aging, and prevents the formation of new neurons, similar to a slow, gradual stroke.
Broader Health Impacts of Alcohol
We’ve said it before, and we’ll say it again: alcohol is bad for pretty much everything.
Here are some examples mentioned in the video:
- Neurodegenerative diseases: heavy drinking increases the risk of Alzheimer’s, particularly in those genetically predisposed.
- Sleep disruption: alcohol reduces deep, restful sleep and hampers the brain’s natural detox process overnight, contributing to morning grogginess.
- Inflammation and immune suppression: alcohol increases inflammation, exacerbates autoimmune diseases (like psoriasis and arthritis), and weakens immune function.
- Cancer risk: alcohol is classified as a Group 1 carcinogen by the International Agency for Research on Cancer, linked to various cancers, especially breast cancer. Even light drinking increases breast cancer risk.
- Hormonal imbalances: in women, alcohol heightens PMS symptoms, reduces fertility, and increases testosterone. In men, it lowers sperm quality and disrupts hormones.
For more on all of these and more, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Can We Drink To Good Health? ← this is mostly about red wine and heart health
- How To Reduce Or Quit Alcohol ← this is about the more general reasons to quit, and how to do so
- What Happens To Your Body When You Stop Drinking Alcohol ← a realistic timeline of recovery
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Syphilis Is Killing Babies. The U.S. Government Is Failing to Stop the Disease From Spreading.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ProPublica is a Pulitzer Prize-winning investigative newsroom. Sign up for The Big Story newsletter to receive stories like this one in your inbox.
Karmin Strohfus, the lead nurse at a South Dakota jail, punched numbers into a phone like lives depended on it. She had in her care a pregnant woman with syphilis, a highly contagious, potentially fatal infection that can pass into the womb. A treatment could cure the woman and protect her fetus, but she couldn’t find it in stock at any pharmacy she called — not in Hughes County, not even anywhere within an hour’s drive.
Most people held at the jail where Strohfus works are released within a few days. “What happens if she gets out before I’m able to treat her?” she worried. Exasperated, Strohfus reached out to the state health department, which came through with one dose. The treatment required three. Officials told Strohfus to contact the federal Centers for Disease Control and Prevention for help, she said. The risks of harm to a developing baby from syphilis are so high that experts urge not to delay treatment, even by a day.
Nearly three weeks passed from when Strohfus started calling pharmacies to when she had the full treatment in hand, she said, and it barely arrived in time. The woman was released just days after she got her last shot.
Last June, Pfizer, the lone U.S. manufacturer of the injections, notified the Food and Drug Administration of an “impending stock out” that it anticipated would last a year. The company blamed “an increase in syphilis infection rates as well as competitive shortages.”
Across the country, physicians, clinic staff and public health experts say that the shortage is preventing them from reining in a surge of syphilis and that the federal government is downplaying the crisis. State and local public health authorities, which by law are responsible for controlling the spread of infectious diseases, report delays getting medicine to pregnant people with syphilis. This emergency was predictable: There have been shortages of this drug in eight of the last 20 years.
Yet federal health authorities have not prevented the drug shortages in the past and aren’t doing much to prevent them in the future.
Syphilis, which is typically spread during sex, can be devastating if it goes untreated in pregnancy: About 40% of babies born to women with untreated syphilis can be stillborn or die as newborns, according to the CDC. Infants that survive can suffer from deformed bones, excruciating pain or brain damage, and some struggle to hear, see or breathe. Since this is entirely preventable, a baby born with syphilis is a shameful sign of a failing public health system.
In 2022, the most recent year for which the CDC has data available, more than 3,700 babies were infected with syphilis, including nearly 300 who were stillborn or died as infants. More than 50% of these cases occurred because, even though the pregnant parent was diagnosed with syphilis, they were never properly treated.
That year, there were 200,000 cases identified in the U.S., a 79% increase from five years before. Infection rates among pregnant people and babies increased by more than 250% in that time; South Dakota, where Strohfus works, had the highest rates — including a more than 400% increase among pregnant women. Statewide, the rate of babies born with the disease, a condition known as congenital syphilis, jumped more than 40-fold in just five years.
And that was before the current shortage of shots.
In Mississippi, the state with the second highest rate of syphilis in pregnant women, Dr. Caroline Weinberg started having trouble this summer finding treatments for her clinic’s patients, most of whom are uninsured, live in poverty or lack transportation. She began spending hours each month scouring medicine suppliers’ websites for available doses of the shots, a form of penicillin sold under the brand name Bicillin L-A.
“The way people do it for Taylor Swift, that’s how I’ve been with the Bicillin shortage,” Weinberg said. “Desperately checking the websites to see what I can snag.”
The shortage is driving up infection rates even further.
In a November survey by the National Coalition of STD Directors, 68% of health departments that responded said the drug shortage will cause syphilis rates in their area to increase, further crushing the nation’s most disadvantaged populations.
“This is the most basic medicine,” said Meghan O’Connell, chief public health officer for the Great Plains Tribal Leaders’ Health Board, which represents 18 tribal communities in South Dakota and three other states. “We allow ourselves to continue to not have enough, and it impacts so many people.”
ProPublica examined what the federal government has done to manage the crisis and the ways in which experts say it has fallen short.
The government could pressure Pfizer to be more transparent.
Twenty years ago, there were at least three manufacturers of the syphilis shot. Then Pfizer, one of the manufacturers, purchased the other two companies and became the lone U.S. supplier.
Pfizer’s supply has fallen short since then. In 2016, the company announced a shortage due to a manufacturing issue; it lasted two years. Even during times when Pfizer had not notified the FDA of an official shortage, clinics across the country told ProPublica, the shots were often hard to get.
Several health officials said they would like to see the government use its power as the largest purchaser of the drug to put pressure on Pfizer to produce adequate supplies and to be more transparent about how much of the drug they have on hand, when it will be widely available and how stable the supply will be going forward.
In response to questions, Pfizer said there are two reasons its supply is falling short. One, the company said, was a surge in use of the pediatric form of the drug after a shortage of a different antibiotic last winter. Pfizer also blamed a 70% increase in demand for the adult shots since last February, which it described as unexpected.
Public health experts say the increase in cases and subsequent rise in demand was easy to see coming. Officials have been raising the alarm about skyrocketing syphilis cases for years. “If Pfizer was truly caught completely off guard, it raises significant questions about the competency of the company to forecast obvious infectious disease trends,” a coalition of organizations wrote to the White House Drug Shortage Task Force in September.
Pfizer said it is consistently communicating with the CDC and FDA about its supply and that it has been transparent with public health groups and policymakers.
The FDA has a group dedicated to addressing drug shortages. But Valerie Jensen, associate director of that staff, said the FDA can’t force manufacturers to make more of a drug. “It is up to manufacturers to decide how to respond to that increased demand.” she said. “What we’re here to do is help with those plans.”
Pfizer said it had a target of increasing production by about 20% in 2023 but faced delays toward the end of the year. The company did not explain the reason for those delays.
The company said it has invested $38 million in the last five years in the Michigan facility where it makes the shots and that it is increasing production capacity. It also said it is adding evening shifts at the facility and actively recruiting and training new workers. Pfizer said it also reduced manufacturing time from 110 to 50 days. By the end of June, the company expects the supply to recover, which it described as having eight weeks of inventory based on its forecast demands with no disruptions in sight.
The government could manufacture the drug itself.
Having only one supplier for a drug, especially one of public health importance, makes the country vulnerable to shortages. With just one manufacturer, any disruption — contamination at a plant, a shortage of raw materials, a severe weather event or a flawed prediction of demand — can put lives at risk. What’s ultimately needed, public health experts say, is another manufacturer.
Congressional Democrats recently introduced a bill that would authorize the U.S. Department of Health and Human Services to manufacture generic drugs in exactly this scenario, when there are few manufacturers and regular shortages. Called the Affordable Drug Manufacturing Act, it would also establish an office of drug manufacturing.
This same bill was introduced in 2018, but it didn’t have bipartisan support and was never taken up for a vote. Sen. Elizabeth Warren, the Massachusetts Democrat who introduced the bill in the Senate, said she’s hopeful this time will be different. Lawmakers from both parties understand the risks created by drug shortages, and COVID-19 helped everyone understand the role the government can play to boost manufacturing.
Still, it’s unlikely to be passed with the current gridlock in Congress.
The government could reserve syphilis drugs for infected patients.
Responding to the shortage of shots to treat the disease, the CDC in July asked health care providers nationwide to preserve the scarce remaining doses for people who are pregnant. The shots are considered the gold standard treatment for anyone with syphilis, faster and with fewer side effects than an alternative pill regimen. And for people who are pregnant, the pills are not an option; the shots are the only safe treatment.
Despite that call, the military is giving shots to new recruits who don’t have syphilis, to prevent outbreaks of severe bacterial respiratory infections. The Army has long administered this treatment at boot camps held at Fort Leonard Wood, Fort Moore and Fort Sill. The Army has been unable to obtain the shots several times in the past few years, according to the U.S. Army Center for Initial Military Training. But the Defense Health Agency’s pharmacy operations center has been working with Pfizer to ensure military sites can get them, a spokesperson for the Defense Health Agency said.
“Until we think about public health the way we think about our military, we’re not going to see a difference,” said Dr. John Vanchiere, chief of pediatric infectious diseases at Louisiana State University Health Shreveport.
Some public health officials, including Alaska’s chief medical officer, Dr. Anne Zink, questioned whether the military should be using scarce shots for prevention.
“We should ask if that’s the best use,” she said.
Using antibiotics to prevent streptococcal outbreaks is a well-established, evidence-based public health practice that’s also used by other branches of the armed services, said Lt. Col. Randy Ready, a public affairs officer with the Army’s Initial Military Training center. “The Army continues to work with the CDC and the entire medical community in regards to public health while also taking into account the unique missions and training environments our Soldiers face,” including basic training, Ready said in a written statement.
The government isn’t stockpiling syphilis drugs.
In rare instances, the federal government has created stockpiles of drugs considered key to public health. In 2018, confronting shortages of various drugs to treat tuberculosis, the CDC created a small stockpile of them. And the federal Administration for Strategic Preparedness and Response keeps a national stockpile of supplies necessary for public health emergencies, including vaccines, medical supplies and antidotes needed in case of a chemical warfare attack.
In November, the Biden administration announced it was creating a new syphilis task force. When asked why the federal government doesn’t stockpile syphilis treatments, Adm. Rachel Levine, the HHS official who leads the task force, said officials don’t routinely stockpile drugs, because they have expiration dates.
In a written statement, an HHS spokesperson said that Bicillin has a shelf life of two years and that the Strategic National Stockpile “does not deploy products that are commercially available.” In general, the spokesperson wrote, stockpiles are most effective before a national shortage begins and can’t overcome the problems of limited suppliers or fragile supply chains. “There is also a risk that stockpiles can exacerbate shortages, particularly when supply is already low, by removing drugs from circulation that would have otherwise been available,” the spokesperson wrote.
Stephanie Pang, a senior director with the coalition of STD directors, said that given the critical role of this drug and the severe access concerns, she thinks a stockpile is necessary. “I don’t have another solution that actually gets drugs to patients,” Pang said.
The government could declare a federal emergency.
Some public health officials say the federal government needs to treat the syphilis crisis the way it did Ebola or monkeypox.
Declare a federal emergency, said Dr. Michael Dube, an infectious disease specialist for more than 30 years. That would free up money for more public health staff and fund more creative approaches that could lead to a long-term solution to the near-constant shortages, he said. “I’d hate to have to wait for some horrible anecdotes to get out there in order to get the public’s and the policymakers’ minds on it,” said Dube, who oversees medical care for AIDS Healthcare Foundation wellness clinics across the country.
Citing an alarming surge in syphilis cases, the Great Plains Tribes wrote to the HHS secretary last week asking that the agency declare a public health emergency in their areas. In the request, they asked HHS to work globally to find adequate syphilis treatment and send the needed medicine to the Great Plains region.
During the 2014 outbreak of Ebola in West Africa, Congress gave hundreds of millions of dollars to HHS to help develop new rapid tests and vaccines. Facing a global outbreak of monkeypox in 2022, a White House task force deployed more than a million vaccines, regularly briefed the public and sent extra resources to Pride parades and other places where people at risk were gathered.
Levine, leader of the federal syphilis task force, countered that declaring an emergency wouldn’t make much of a difference. The government, she said, already has a “dramatic and coordinated response” involving several agencies.
The FDA recently approved an emergency import of a similar syphilis treatment made by a French manufacturer that had plenty on hand. According to the company, Provepharm, the imported shots are enough to cover approximately one or two months of typical use by all people in the U.S. (The FDA would not say how many doses Provepharm sent, and the company said it was not allowed to reveal that number under the federal rules governing such emergency imports.)
Clinics applaud that development. But many of them can’t afford the imported shots.
The government could do more to rein in the cost.
Clinics and hospitals that primarily serve low-income patients often qualify for a federal program that allows them to purchase drugs at steeply discounted prices. Pharmaceutical companies that want Medicaid to cover their outpatient drugs must participate in the program.
One factor in determining the discount price is whether a pharmaceutical company has raised the price of a drug by more than the rate of inflation. Because Pfizer has hiked the price of its Bicillin shots significantly over the years, the government requires that it be sold to qualifying clinics for just pennies a dose. Otherwise, a single Pfizer shot can retail for upwards of $500. The French shots are comparable in retail price and not eligible for the discount program.
Several clinic directors also said they worried that drug distributors were reserving the limited supply of the Pfizer shot for organizations that could pay full price. For several days in January, for example, the website of Henry Schein, a medical supplier, showed doses of the shot available at full price, while doses at the penny pricing were out of stock, according to screenshots shared with ProPublica. When asked whether it was only selling shots at full price, a spokesperson for Henry Schein did not respond to the question.
Local health departments that qualify for the discount program told ProPublica they’ve had to pay full price at other distributors, because it was the only stock available.
The Health Resources and Services Administration, the federal agency that regulates the discount program, said that a drug manufacturer is ultimately responsible for ensuring that when supplies are available, they are available at the discounted price. When asked about this, Pfizer said that it has “one inventory that is distributed to our trade partners” and that hospitals and clinics that qualify for the discount program are “responsible for ensuring compliance with the program and orders through the wholesaler accordingly.” The company added, “Pfizer plays no part in this process.”
In October, on Weinberg’s regular search for shots for her Mississippi clinic, she found doses of Bicillin for sale at the discounted price and purchased 40. “The idea that we’re supposed to be hoarding treatment is a horrific compact,” she said. Word got out that the clinic, called Plan A, has some shots, and other clinics began sending pregnant patients there.
The clinic’s supply is dwindling. Weinberg is happy to get the shots to patients who need them. But she’s not sure how much longer her reserve will last — or if she’ll be able to find more when they’re gone.
Share This Post
-
The Circadian Code – by Dr. Satchin Panda
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There’s a lot more to circadian rhythm than “sleep during these hours”. And there’s a lot more to bear in mind than “don’t have blue/white light at night”.
In fact, Dr. Satchin Panda explains, there’s a whole daily symphony of movements in our body as different biochemical processes wax and wane according to what time of day it is.
There are several important things he wants us to know about this:
- Our body needs to know what time it is, for those processes to work correctly
- Because of these daily peaks and troughs of various physiological functions, we get “correct” times for things we do every day. Not just sleeping/waking, but also:
- The best time to eat
- The best time to exercise
- The best time to do mental work
- The best times to take different kinds of supplements/medications
Dr. Panda also looks at what things empower, or disempower, our body to keep track of what time it is.
Bottom line: if you’d like to optimize your days and your health, this book has a lot of very valuable practicable tips.
Click here to check out The Circadian Code, and make the most of yours!
Share This Post
-
Hazelnuts vs Pecans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing hazelnuts to pecans, we picked the hazelnuts.
Why?
In terms of macros, hazelnuts have more protein, carbs, and fiber, though the difference is not big in the latter two cases, and the glycemic indices are resultantly about the same. Meanwhile, pecans have a little more fat, but the fat is healthy in both cases. Everything taken into account, we’re calling it a tie on macros.
When it comes to vitamins, hazelnuts have more of vitamins B3, B5, B6, B7, B9, C, E, K, and choline, while pecans have more of vitamins A, B1, and B2. An easy win for hazelnuts here.
In the category of minerals, hazelnuts have more calcium, copper, iron, magnesium, manganese, phosphorus, and potassium, while pecans have more selenium and zinc. Another clear win for hazelnuts.
In short, enjoy either or both (unless you’re allergic, in which case, don’t), but hazelnuts are ultimately the more nutritionally dense of the two.
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Share This Post
Related Posts
-
Sizing Aside: Are You Wearing The Right Bra For Your Breast Shape?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s well-known that most women wear incorrectly-fitting bras. Even with careful measurements, buying “off-the-rack” can be a challenge, because the sizing system only takes two measurements, when there are actually many more things to consider. Today’s video demystifies a lot of what else is going on!
For example…
Some of the different breast shapes/arrangements to consider:
- Wide-set breasts: likely to find there’s a bit of a gap between your breasts and the inside (nearest to your sternum) parts of the cups—while spilling out a little at the outside edges. The solution? Bras that offer side-support, to keep things pointing more forwards. Central-closing bras can also help gather things together, and a balconette bra can redistribute things more evenly. Any of these options will be a lot more comfortable.
- Small breasts: bralettes are your friend, keeping things comfortable while not wearing more bra than necessary to do the job (of course going braless is also an option, but we’re talking bra-fitting here, not bra-flinging-off never to be seen again)
- Deflated breasts: often the case for someone who used to have larger breasts, but they lost size for hormonal reasons rather than for weight loss reasons. This often occurs a little while after childbirth, and also happens a lot in menopause. The bra recommendation for this? A push-up plunge bra with ¾ coverage not only provides cleavage if that’s wanted, but also, will keep things much more snug and thus more evenly-distributed. If ever you’ve found yourself needing to adjust yourself every now and gain while out, this will fix that and keep you comfortable for much longer.
There’s more, along with a visual guide, so do check it out:
Click Here If The Embedded Video Doesn’t Load Automatically!
Further reading
While we haven’t written about this specifically (maybe we’ll do a “Life Hacks” edition one of these days), we have written about…
Keeping Abreast Of Your Cancer Risk
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
When Doctors Make House Calls, Modern-Style!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
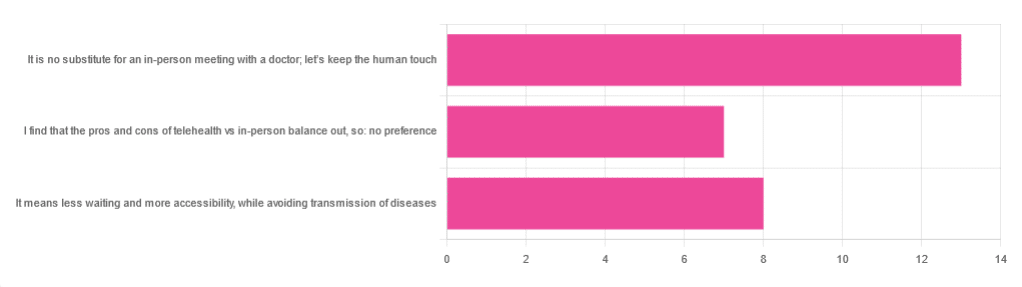
In Tuesday’s newsletter, we asked you foryour opinion of telehealth for primary care consultations*, and got the above-depicted, below-described, set of responses:
- About 46% said “It is no substitute for an in-person meeting with a doctor; let’s keep the human touch”
- About 29% said “It means less waiting and more accessibility, while avoiding transmission of diseases”
- And 25 % said “I find that the pros and cons of telehealth vs in-person balance out, so: no preference”
*We specified that by “primary care” we mean the initial consultation with a non-specialist doctor, before receiving treatment or being referred to a specialist. By “telehealth” we mean by videocall or phonecall.
So, what does the science say?
A quick note first
Because telehealth was barely a thing (statistically speaking) before the first stages of the COVID pandemic, compared to how it is now, most of the science for this is young, and a lot of the science simply hasn’t been done yet, and/or has not been published yet, because the process can take years.
Because of this, some studies we do have aren’t specifically about primary care, and are sometimes about specialists. We think this should not affect the results much, but it bears highlighting.
Nevertheless, we’ll do what we can with the science we have!
Telehealth is more accessible than in-person consultations: True or False?
True, for most people. For example…
❝Data was found from a variety of emergency and non-emergency departments of primary, secondary, and specialised healthcare.
Satisfaction was high among recipients of healthcare, scoring 9-10 on a scale of 0-10 or ranging from 73.3% to 100%.
Convenience was rated high in every specialty examined. Satisfaction of clinicians was high throughout the specialities despite connection failure and concerns about confidentiality of information.❞
whereas…
❝Nonetheless, studies reported perception of increased barriers to accessing care and inequalities for vulnerable patients especially in older people❞
~ Ibid.
Source: Satisfaction with telemedicine use during COVID-19 pandemic in the UK: a systematic review
Now, perception of those things does necessarily equate to an actual increased barrier, but it is reasonable that someone who thinks something is inaccessible will be less inclined to try to access it.
The quality of care provided via telehealth is as good as in-person: True or False?
True, ostensibly, with caveats. The caveats are:
- We’re going offreported patient satisfaction, not objective patient health outcomes (we found little* science as yet for the relative incidence of misdiagnosis, for example—which kind of thing will take time to be revealed).
- We’re also therefore speaking (as statistics do) for the significant majority of people. However, if we happen to be (statistically speaking) an insignificant minority, well, that just sucks for us personally.
*we did find some, but it wasn’t very helpful yet. For example:
An electronic trigger to detect telemedicine-related diagnostic errors
this one does look at the incidence of diagnostic errors, but provides no control group (i.e. otherwise-comparable in-person consultations) for comparison.
While most oft-considered demographic groups reported comparable patient satisfaction (per race, gender, and socioeconomic status, for example), there was one outlier variable, which was age (as we quoted from that first study above).
However!
Looking under the hood of these stats, it seems that age is not the real culprit, so much as technological illiteracy, which is heavily correlated with age:
❝Lower eHealth literacy is associated with more negative attitudes towards I/C technology in healthcare. This trend is consistent across diverse demographics and regions. ❞
Source: Meta-analysis: eHealth literacy and attitudes towards internet/computer technology
There are things that can be done at an in-person consultation that can’t be done by telehealth: True or False?
True, of course. It is incredibly rare that we will cite “common sense”, (as sometimes “common sense” is actually “common mistakes” and is simply and verifiably wrong), but in this case, as one 10almonds subscriber put it:
❝The doctor uses his five senses to assess. This cannot be attained over the phone❞
~ 10almonds subscriber
A quick note first: if your doctor is using their sense of taste to diagnose you, please get a different doctor, because they should definitely not be doing that!
Not in this century, anyway… Once upon a time, diabetes was diagnosed by urine-tasting (and yes, that was a fairly reliable method).
However, nowadays indeed a doctor will use sight, sound, touch, and sometimes even smell.
In a videocall we’re down to two of those senses (sight and sound), and in a phonecall, down to one (sound) and even that is hampered. Your doctor cannot, for example, use a stethoscope over the phone.
With this in mind, it really comes down to what you need from your doctor in that consultation.
- If you’re 99% sure that what you need is to be prescribed an antidepressant, that probably doesn’t need a full physical.
- If you’re 99% sure that what you need is a referral, chances are that’ll be fine by telehealth too.
- If your doctor is 99% sure that what you need is a verbal check-up (e.g. “How’s it been going for you, with the medication that I prescribed for you a month ago?”, then again, a call is probably fine.
If you have a worrying lump, or an unhappy bodily discharge, or an unexplained mysterious pain? These things, more likely an in-person check-up is in order.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Kidney Beans vs Chickpeas – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing kidney beans to chickpeas, we picked the chickpeas.
Why?
Both are great! But there’s a clear winner here today:
In terms of macros, chickpeas have more protein, carbs, and fiber, making them the more nutrient-dense option in this category.
In the category of vitamins, kidney beans have more of vitamins B1, B3, and K, while chickpeas have more of vitamins A, B2, B5, B6, B7, B9, C, E, and choline, taking the victory again here.
When it comes to minerals, it’s a similar story: kidney beans have more potassium, while chickpeas have more calcium, copper, iron, magnesium, manganese, phosphorus, selenium, and zinc. Another easy win for chickpeas.
Adding up the three wins makes chickpeas the clear overall winner, but of course, as ever, enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: