Apricot vs Banana – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing apricot to banana, we picked the banana.
Why?
Both are great, and it was close!
In terms of macros, apricot has more protein, while banana has more carbs and fiber; both are low glycemic index foods, and we’ll call this category a tie.
In the category of vitamins, apricot has more of vitamins A, C, E, and K, while banana has more of vitamins B1, B2, B3, B5, B6, B7, B9, and choline, giving banana the win by strength of numbers. It’s worth noting though that apricots are one of the best fruits for vitamin A in particular.
When it comes to minerals, apricot has slightly more calcium, iron, and zinc, while banana has a lot more magnesium, manganese, potassium, and selenium, meaning a moderate win for banana here.
Adding up the sections makes for an overall win for banana—but of course, by all means enjoy either or both!
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer ← we argue for apricots as bonus number 9 on the list
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Creatine, Genomic Screening, & More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In this week’s health news…
Creatine: no difference vs control at 5g/day
A study found, as the title suggests, no difference between creatine and placebo, at the usual dose of 5g/day, while doing a supervised resistance training program.
This was a 12-week trial, and in the first week, the creatine group put on an average of 0.5kg more lean (i.e. not fat) body mass than the control group, however, as this quickly equalized after the first week, it is assumed that the brief extra weight gain was water weight (creatine promotes water retention, especially in the initial phase).
However, it is still possible that it may promote weight gain at higher doses.
This study was done with adult participants under the age of 50; we’ve noted before that it is generally young people who use creatine for bodybuilding, so in principle, this should have been ideal for that, but it wasn’t.
Read in full: Sports supplement creatine makes no difference to muscle gains, trial finds
Related: Creatine’s Brain Benefits Increase With Age ← this, on the other hand, does work—but only for older adults.
Genomics & disease risk: what to know
In a recent study evaluation, 175,500 participants were screened, and 1 in 30 received medically important genetic results. More than 90% of those found to have a genetic risk were previously unaware of it.
This is important, because most current genetic risk assessment for patients is based on personal and family history, which often misses a lot of data due to barriers to care or lack of family history.
Genomic screening helps close these gaps:
Read in full: Genomic screening is important in identifying disease risk, study finds
Related: Do You Have A Personalized Health Plan? (Here’s How)
FDA-Approved Antivirals (Not Vaccines) Ineffective Against H5N1
The H5N1 avian influenza outbreak is now rife amongst dairy farms, with the virus found in cows’ milk and infecting farmworkers. Researchers studied potential treatments, revealing two FDA-approved antivirals (baloxavir and oseltamivir) were generally ineffective in treating severe H5N1 infections.
Oral infections per raw milk consumption, were the most severe and hardest to treat, and the virus spread quickly to the blood and brain (when the infection is respiratory, it is much slower to spread from the respiratory tract).
It wasn’t a complete loss, though:
- Eye infections were better controlled with baloxavir, achieving a 100% survival rate compared to 25% with oseltamivir.
- For nasal infections, baloxavir reduced viral levels better but still allowed the virus to reach the brain. Survival rates were 75% for baloxavir and 50% for oseltamivir.
The researchers in question are urging preventative measures as being of critical importance, given the difficulty of treatment:
Read in full: Current antivirals likely less effective against severe infection caused by bird flu virus in cows’ milk
Related: Bird Flu: Children At High Risk; Older Adults Not So Much
Take care!
Share This Post
-
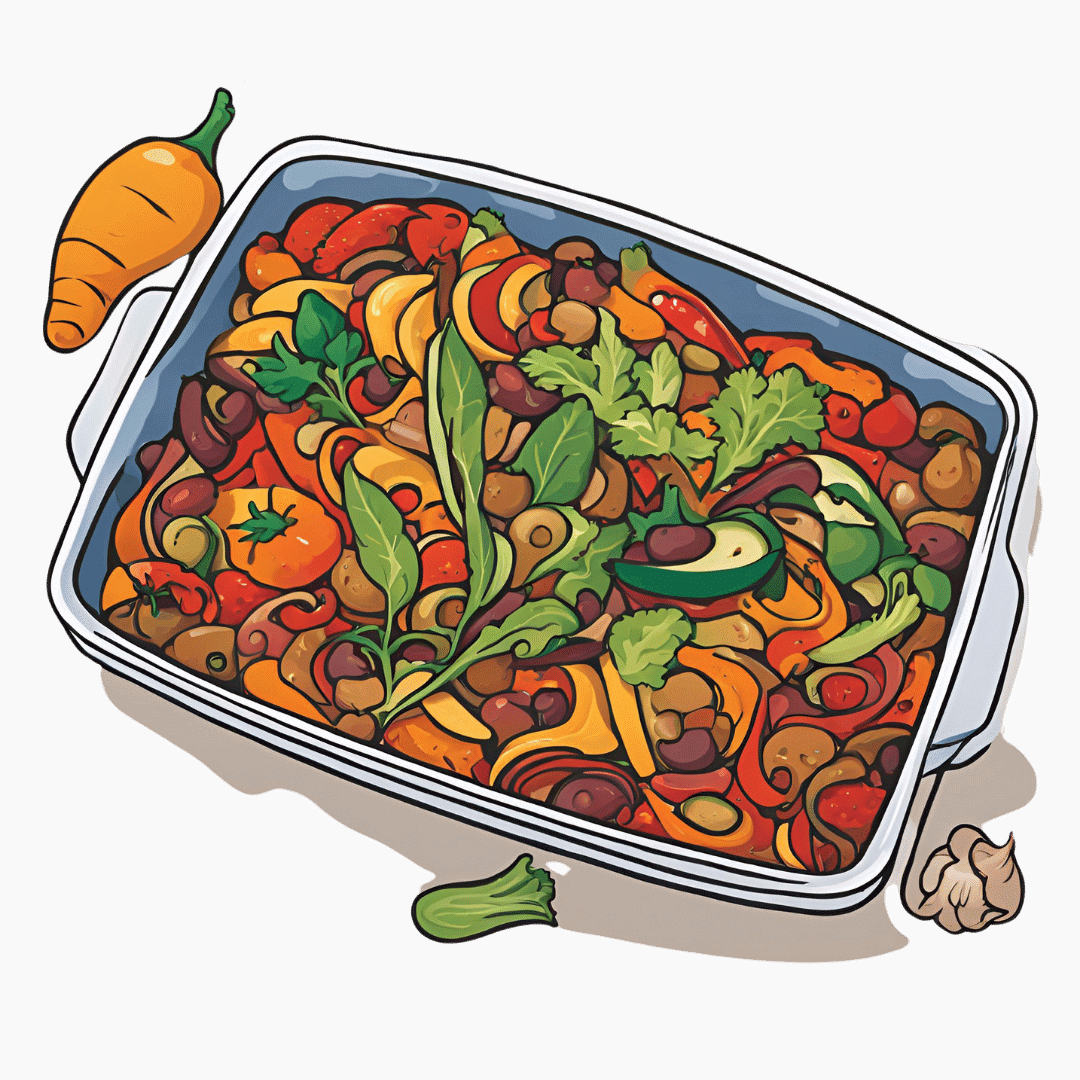
Oven-Roasted Ratatouille
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a supremely low-effort, high-yield dish. It’s a nutritional tour-de-force, and very pleasing to the tastebuds too. We use flageolet beans in this recipe; they are small immature kidney beans. If they’re not available, using kidney beans or really any other legume is fine.
You will need
- 2 large zucchini, sliced
- 2 red peppers, sliced
- 1 large eggplant, sliced and cut into semicircles
- 1 red onion, thinly sliced
- 2 cans chopped tomatoes
- 2 cans flageolet beans, drained and rinsed (or 2 cups same, cooked, drained, and rinsed)
- ½ bulb garlic, crushed
- 2 tbsp extra virgin olive oil
- 1 tbsp balsamic vinegar
- 1 tbsp black pepper, coarse ground
- 1 tbsp nutritional yeast
- 1 tbsp red chili pepper flakes (omit or adjust per your heat preferences)
- ½ tsp MSG or 1 tsp low-sodium salt
- Mixed herbs, per your preference. It’s hard to go wrong with this one, but we suggest leaning towards either basil and oregano or rosemary and thyme. We also suggest having some finely chopped to go into the dish, and some held back to go on the dish as a garnish.
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 350℉ / 180℃.
2) Mix all the ingredients (except the tomatoes and herbs) in a big mixing bowl, ensuring even distribution.
2) Add the tomatoes. The reason we didn’t add these before is because it would interfere with the oil being distributed evenly across the vegetables.
3) Transfer to a deep-walled oven tray or an ovenproof dish, and roast for 30 minutes.
4) Stir, add the chopped herbs, stir again, and return to the oven for another 30 minutes.
5) Serve (hot or cold), adding any herb garnish you wish to use.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Lycopene’s Benefits For The Gut, Heart, Brain, & More
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- Capsaicin For Weight Loss And Against Inflammation
- The Many Health Benefits Of Garlic
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
Take care!
Share This Post
-
Berberine For Metabolic Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Is Berberine Nature’s Ozempic/Wegovy?
Berberine is a compound found in many plants. Of which, some of them are variations of the barberry, hence the name.
It’s been popular this past couple of years, mostly for weight loss. In and of itself, something being good for weight loss doesn’t mean it’s good for the health (just ask diarrhoea, or cancer).
Happily, berberine’s mechanisms of action appear to be good for metabolic health, including:
- Reduced fasting blood sugar levels
- Improved insulin sensitivity
- Reduced LDL and triglycerides
- Increased HDL levels
So, what does the science say?
It’s (mostly!) not nature’s Wegovy/Ozempic
It’s had that title in a number of sensationalist headlines (and a current TikTok trend, apparently), but while both berberine and the popular weight-loss drugs Wegovy/Ozempic act in part on insulin metabolism, they mostly do so by completely different mechanisms.
Wegovy and Ozempic are GLP-1 agonists, which mean they augment the action of glucagon-like-peptide 1, which increases insulin release, decreases glucagon release, and promotes a more lasting feeling of fullness.
Berberine works mostly by other means, not all of which are understood. But, we know that it activates AMP-activated protein kinase, and on the flipside, inhibits proprotein convertase subtilisin/kexin type 9.
In less arcane words: it boosts some enzymes and inhibits others.
Each of these boosts/inhibitions has a positive effect on metabolic health.
However, it does also have a slight GLP-1 agonist effect too! Bacteria in the gut can decompose and metabolize berberine into dihydroberberine, thus preventing the absorption of disaccharides in the intestinal tract, and increasing GLP-1 levels.
See: Effects of Berberine on the Gastrointestinal Microbiota
Does it work for weight loss?
Yes, simply put. And if we’re going to put it head-to-head with Wegovy/Ozempic, it works about half as well. Which sounds like a criticism, but for a substance that’s a lot safer (and cheaper, and easier—if we like capsules over injections) and has fewer side effects.
- Weight Loss Outcomes Associated With Semaglutide Treatment for Patients With Overweight or Obesity ← Wegovy and Ozempic are both brand names of semaglutide
- The effect of berberine supplementation on obesity parameters: A systematic review and meta-analysis of randomized controlled trials ← a good recent research review giving clear data on many factors
- Lipid-lowering effect of berberine in human subjects and rats ← this is an older study, 2012, but it gives 3-month weight loss percentages rather than discrete values in the abstract, so it’s easier to compare to the semaglutide study without grabbing a calculator
❝But more interestingly, the treatment significantly reduced blood lipid levels (23% decrease of triglyceride and 12.2% decrease of cholesterol levels) in human subjects.
However, there was interestingly, an increase in calcitriol levels seen in all human subjects following berberine treatment (mean 59.5% increase)
Collectively, this study demonstrates that berberine is a potent lipid-lowering compound with a moderate weight loss effect, and may have a possible potential role in osteoporosis treatment/prevention.❞
(click through to read in full)
Is it safe?
It appears to be, with one special caveat: remember that paper about the effects of berberine on the gastrointestinal microbiota? It also has some antimicrobial effects, so you could do harm there if not careful. It’s recommended to give it a break every couple of months, to be sure of allowing your gut microbiota to not get too depleted.
Also, as with anything you might take that’s new, always consult your doctor/pharmacist in case of contraindications based on medications you are taking.
Where can I get it?
As ever, we don’t sell it, but here’s an example product on Amazon, for your convenience.
Enjoy!
Share This Post
Related Posts
-
Top Foods Against Neuroinflammation
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Chronic inflammation is something you might feel in your joints, but it will usually be in the brain too. There, neuroinflammation can disrupt brain function, affecting stress responses, mood, cognition, and even alter brain structure. It’s also heavily implicated in the pathogenesis of various forms of dementia.
What to do about it
Dr. Tracey Marks, psychiatrist, bids us eat:
- Fatty fish: omega-3-rich fish like salmon reduce neuroinflammation.
- Leafy greens: spinach, kale, and collards protect brain cells and support neurotransmitter production.
- Berries: blueberries and strawberries improve memory and protect neurons.
- Nuts and seeds: walnuts, almonds, and flaxseeds support brain health and reduce inflammation.
- Turmeric: curcumin combats inflammation and supports neuron growth (best with supplements).
- Fermented foods: yogurt and sauerkraut improve gut health, benefiting the brain via the gut-brain axis; not just the vagus nerve, but also, remember that various neurotransmitters (including serotonin) are made in the gut.
Of course, you should also avoid alcohol, nicotine, red meat, processed meat, and ideally also white flour products, and sugary foods (unless they are also rich in fiber, like whole fruit).
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How to Prevent (or Reduce) Inflammation
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Ikigai – by Héctor García and Francesc Miralles
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ikigai is the Japanese term for what in English we often call “raison d’être”… in French, because English is like that.
But in other words: ikigai is one’s purpose in life, one’s reason for living.
The authors of this work spend some chapters extolling the virtues of finding one’s ikigai, and the health benefits that doing so can convey. It is, quite clearly, an important and relevant factor.
The rest of the book goes beyond that, though, and takes a holistic look at why (and how) healthy longevity is enjoyed by:
- Japanese people in general,
- Okinawans in particular,
- Residents of Okinawa’s “blue zone” village with the highest percentage of supercentenarians, most of all.
Covering considerations from ikigai to diet to small daily habits to attitudes to life, we’re essentially looking at a blueprint for healthy longevity.
For a book whose title and cover suggests a philosophy-heavy content, there’s a lot of science in here too, by the way! From microbiology to psychiatry to nutrition science to cancer research, this book covers all bases.
In short: this book gives a lot of good science-based suggestions for adjustments we can make to our lives, without moving to an Okinawan village!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Good to Go – by Christie Aschwanden
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Many of us may more often need to recover from a day of moving furniture than running a marathon, but the science of recovery can still teach us a lot. The author, herself an endurance athlete and much-decorated science journalist, sets out to do just that.
She explores a lot of recovery methods, and examines whether the science actually backs them up, and if so, to what degree. She also, in true science journalism style, talks to a lot of professionals ranging from fellow athletes to fellow scientists, to get their input too—she is nothing if not thorough, and this is certainly not a book of one person’s opinion with something to sell.
Indeed, on the contrary, her findings show that some of the best recovery methods are the cheapest, or even free. She also looks at the psychological aspect though, and why many people are likely to continue with things that objectively do not work better than placebo.
The style is very easy-reading jargon-free pop-science, while nevertheless being backed up with hundreds of studies cited in the bibliography—a perfect balance of readability and reliability.
Bottom line: for those who wish to be better informed about how to recover quickly and easily, this book is a treasure trove of information well-presented.
Click here to check out Good To Go, and always be good to go!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: