Reishi Mushrooms: Which Benefits Do They Really Have?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Reishi Mushrooms
Another Monday Research Review, another mushroom! If we keep this up, we’ll have to rename it “Mushroom Monday”.
But, there’s so much room for things to say, and these are fun guys to write about, as we check the science for any spore’ious claims…
Why do people take reishi?
Popular health claims for the reishi mushroom include:
- Immune health
- Cardiovascular health
- Protection against cancer
- Antioxidant qualities
- Reduced fatigue and anxiety
And does the science agree?
Let’s take a look, claim by claim:
Immune health
A lot of research for this has been in vitro (ie, with cell cultures in labs), but promising, for example:
Immunomodulating Effect of Ganoderma lucidum (Lingzhi) and Possible Mechanism
(that is the botanical name for reishi, and the Chinese name for it, by the way)
That’s not to say there are no human studies though; here it was found to boost T-cell production in stressed athletes:
Cardiovascular health
Here we found a stack of evidence for statistically insignificant improvements in assorted measures of cardiovascular health, and some studies where reishi did not outperform placebo.
Because the studies were really not that compelling, instead of taking up room (and your time) with them, we’re going to move onto more compelling, exciting science, such as…
Protection against cancer
There’s a lot of high quality research for this, and a lot of good results. The body of evidence here is so large that even back as far as 2005, the question was no longer “does it work” or even “how does it work”, but rather “we need more clinical studies to find the best doses”. Researchers even added:
❝At present, lingzhi is a health food supplement to support cancer patients, yet the evidence supporting the potential of direct in vivo anticancer effects should not be underestimated.❞
Check it out:
Anticancer effects of Ganoderma lucidum: a review of scientific evidence
Just so you know we’re not kidding about the weight of evidence, let’s drop a few extra sources:
- Ganoderma lucidum: a rational pharmacological approach to surmount cancer
- Ganoderma lucidum as an anti-cancer agent
- Extract from Ganoderma lucidum suppresses cervical cancer cell malignancy
- Ganoderma lucidum spore oil induces apoptosis of breast cancer cells
- Ganoderma lucidum enhances carboplatin chemotherapy effect
- Ganoderma lucidum inhibits prostate cancer cell migration
- Ganoderma lucidum fruiting body extracts inhibit colorectal cancer
- Inhibitory activity of medicinal mushroom Ganoderma lucidum on colorectal cancer
- Ganoderma lucidum (reishi mushroom) for cancer treatment
By the way, we shortened most of those titles for brevity, but almost all of the continued with “by” followed by a one-liner of how it does it.
So it’s not a “mysterious action” thing, it’s a “this is a very potent medicine and we know how it works” thing.
Antioxidant qualities
Here we literally only found studies to say no change was found, one that found a slight increase of antioxidant levels in urine. It’s worth noting that levels of a given thing (or its metabolites, in the case of some things) in urine are often quite unhelpful regards knowing what’s going on in the body, because we get to measure only what the body lost, not what it gained/kept.
So again, let’s press on:
Reduced fatigue and anxiety
Most of the studies for this that we could find pertained to health-related quality of life for cancer patients specifically, so (while they universally give glowing reports of reishi’s benefits to health and happiness of cancer patients), that’s a confounding factor when it comes to isolating its effects on reduction of fatigue and anxiety in people without cancer.
Here’s one that looked at it in the case of reduction of fatigue, anxiety, and other factors, in patients without cancer (but with neurathenia), in which they found it was “significantly superior to placebo with respect to the clinical improvement of symptoms”.
Summary:
- Reishi mushroom’s anti-cancer properties are very, very clear
- There is also good science to back immune health claims
- It also has been found to significantly reduce fatigue and anxiety in unwell patients (we’d love to see more studies on its benefits in otherwise healthy people, though)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
It’s Not You, It’s Your Hormones – by Nicki Williams, DipION, mBANT, CNHC
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
So, first a quick note: this book is very similar to the popular bestseller “The Galveston Diet”, not just in content, but all the way down to its formatting. Some Amazon reviewers have even gone so far as to suggest that “It’s Not You, It’s Your Hormones” (2017) brazenly plagiarized “The Galveston Diet” (2023). However, after carefully examining the publication dates, we feel quite confident that this book is not a copy of the one that came out six years after it. As such, we’ve opted for reviewing the original book.
Nicki Williams’ basic principle is that we can manage our hormonal fluctuations, by managing our diet. Specifically, in three main ways:
- Intermittent fasting
- Anti-inflammatory diet
- Eating more protein and healthy fats
Why should these things matter to our hormones? The answer is to remember that our hormones aren’t just the sex hormones. We have hormones for hunger and satedness, hormones for stress and relaxation, hormones for blood sugar regulation, hormones for sleep and wakefulness, and more. These many hormones make up our endocrine system, and affecting one part of it will affect the others.
Will these things magically undo the effects of the menopause? Well, some things yes, other things no. No diet can do the job of HRT. But by tweaking endocrine system inputs, we can tweak endocrine system outputs, and that’s what this book is for.
The style is very accessible and clear, and Williams walks us through the changes we may want to make, to avoid the changes we don’t want.
In the category of criticism, there is some extra support that’s paywalled, in the sense that she wants the reader to buy her personally-branded online plan, and it can feel a bit like she’s holding back in order to upsell to that.
Bottom line: this book is aimed at peri-menopausal and post-menopausal women. It could also definitely help a lot of people with PCOS too, and, when it comes down to it, pretty much anyone with an endocrine system. It’s a well-evidenced, well-established, healthy way of eating regardless of age, sex, or (most) physical conditions.
Click here to check out It’s Not You, It’s Your Hormones, and take control of yours!
Share This Post
-
Plant vs Animal Protein
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Plant vs Animal Protein: Head to Head
Some people will obviously have strong ideological opinions here—for vegetarians and vegans, it’s no question, and for meat-eaters, it’s easy to be reactive to that and double-down on the bacon. But, we’re a health science newsletter, so we’ll be sticking to the science.
Which is better, healthwise?
First, it depends on how you go about it. Consider these options:
- A piece of salmon
- A steak
- A hot dog
- A hot dog, but plant-based
- Textured soy protein (no additives)
- Edamame (young soy) beans
Three animal-based protein sources, three plant-based. We could render the competition simple (but very unfair) by pitting the hotdog against the edamame beans, or the plant-based hot dog against the piece of salmon. So let’s kick this off by saying:
- There are good and bad animal-based protein sources
- There are good and bad plant-based protein sources
Whatever you choose, keep that in mind while you do. Less processed is better in either case. And if you do go for red meat, less is better, period.
Picking the healthiest from each, how do the nutritional profiles look?
They look good in both cases! One factor of importance is that in either case, our bodies will reduce the proteins we consume to their constituent amino acids, and then rebuild them into the specific proteins we actually need. Our bodies will do that regardless of the source, because we are neither a salmon nor a soybean, for example.
We need 20 specific amino acids, for our bodies to make the proteins we will use in our bodies. Of these, 9 are considered “essential”, meaning we cannot synthesize them and must get them from our diet,
Animal protein sources contain all 9 of those (just like we do). Plant based sources often don’t, individually, but by eating soy for example (which does contain them all) and/or getting multiple sources of protein from different plants, the 9 can be covered quite easily with little thought, just by having a varied diet.
Meats are #1!
- They’re number 1 for nutritional density
- They’re number 1 for health risks, too
So while plant-based diet adherents may need to consume more varied things to get all the nutrients necessary, meat-eaters won’t have that problem.
Meat-eaters will instead have a different problem, of more diet-related health risks, e.g.
- Cardiovascular disease
- Metabolic disorders
- Cancers
So again, if eating (especially processed and/or red) meat, moderation is good. The Mediterranean Diet that we so often recommend, by default contains small amounts of lean animal protein.
Which is better for building muscle?
Assuming a broadly healthy balanced diet, and getting sufficient protein from your chosen source, they’re pretty equal:
- Vegan and Omnivorous High Protein Diets Support Comparable Daily Myofibrillar Protein Synthesis Rates and Skeletal Muscle Hypertrophy in Young Adults
- A mycoprotein-based high-protein vegan diet supports equivalent daily myofibrillar protein synthesis rates compared with an isonitrogenous omnivorous diet in older adults: a randomised controlled trial
(both studies showed that both dietary approaches yielded results that showed no difference in muscle synthesis between the two)
The bottom line is…
Healthwise, what’s more important than whether you get your protein from animals or plants is that you eat foods that aren’t processed, and are varied.
And if you want to do a suped-up Mediterranean Diet with less red meat, you might want to try:
A Pesco-Mediterranean Diet With Intermittent Fasting: JACC Review Topic of the Week
^This is from a review in the Journal of the American College of Cardiology, and in few words, they recommend it very highly
Share This Post
-
Never Too Old?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Age Limits On Exercise?
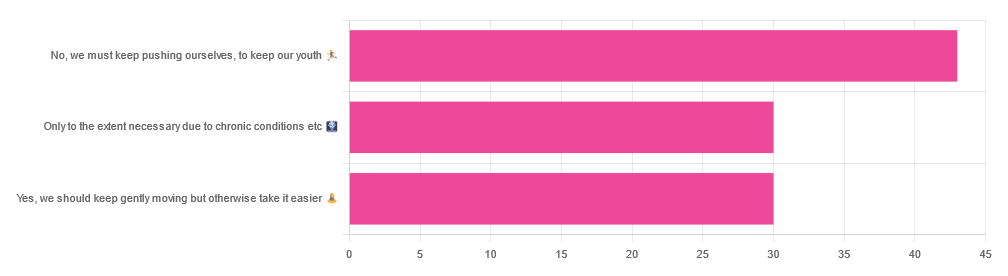
In Tuesday’s newsletter, we asked you your opinion on whether we should exercise less as we get older, and got the above-depicted, below-described, set of responses:
- About 42% said “No, we must keep pushing ourselves, to keep our youth“
- About 29% said “Only to the extent necessary due to chronic conditions etc”
- About 29% said “Yes, we should keep gently moving but otherwise take it easier”
One subscriber who voted for “No, we must keep pushing ourselves, to keep our youth“ wrote to add:
❝I’m 71 and I push myself. I’m not as fast or strong as I used to be but, I feel great when I push myself instead of going through the motions. I listen to my body!❞
~ 10almonds subscriber
One subscriber who voted for “Only to the extent necessary due to chronic conditions etc” wrote to add:
❝It’s never too late to get stronger. Important to keep your strength and balance. I am a Silver Sneakers instructor and I see first hand how helpful regular exercise is for seniors.❞
~ 10almonds subscriber
One subscriber who voted to say “Yes, we should keep gently moving but otherwise take it easier” wrote to add:
❝Keep moving but be considerate and respectful of your aging body. It’s a time to find balance in life and not put yourself into a positon to damage youself by competing with decades younger folks (unless you want to) – it will take much longer to bounce back.❞
~ 10almonds subscriber
These will be important, because we’ll come back to them at the end.
So what does the science say?
Endurance exercise is for young people only: True or False?
False! With proper training, age is no barrier to serious endurance exercise.
Here’s a study that looked at marathon-runners of various ages, and found that…
- the majority of middle-aged and elderly athletes have training histories of less than seven years of running
- there are virtually no relevant running time differences (p<0.01) per age in marathon finishers from 20 to 55 years
- after 55 years, running times did increase on average, but not consistently (i.e. there were still older runners with comparable times to the younger age bracket)
The researchers took this as evidence of aging being indeed a biological process that can be sped up or slowed down by various lifestyle factors.
See also:
Age & Aging: What Can (And Can’t) We Do About It?
this covers the many aspects of biological aging (it’s not one number, but many!) and how our various different biological ages are often not in sync with each other, and how we can optimize each of them that can be optimized
Resistance training is for young people only: True or False?
False! In fact, it’s not only possible for older people, but is also associated with a reduction in all-cause mortality.
Specifically, those who reported strength-training at least once per week enjoyed longer lives than those who did not.
You may be thinking “is this just the horse-riding thing again, where correlation is not causation and it’s just that healthier people (for other reasons) were able to do strength-training more, rather than the other way around?“
…which is a good think to think of, so well-spotted if you were thinking that!
But in this case no; the benefits remained when other things were controlled for:
❝Adjusted for demographic variables, health behaviors and health conditions, a statistically significant effect on mortality remained.
Although the effects on cardiac and cancer mortality were no longer statistically significant, the data still pointed to a benefit.
Importantly, after the physical activity level was controlled for, people who reported strength exercises appeared to see a greater mortality benefit than those who reported physical activity alone.❞
See the study: Is strength training associated with mortality benefits? A 15 year cohort study of US older adults
And a pop-sci article about it: Strength training helps older adults live longer
Closing thoughts
As it happens… All three of the subscribers we quoted all had excellent points!
Because in this case it’s less a matter of “should”, and more a selection of options:
- We (most of us, at least) can gain/regain/maintain the kind of strength and fitness associated with much younger people, and we need not be afraid of exercising accordingly (assuming having worked up to such, not just going straight from couch to marathon, say).
- We must nevertheless be mindful of chronic conditions or even passing illnesses/injuries, but that goes for people of any age
- We also can’t argue against a “safety first” cautious approach to exercise. After all, sure, maybe we can run marathons at any age, but that doesn’t mean we have to. And sure, maybe we can train to lift heavy weights, but if we’re content to be able to carry the groceries or perhaps take our partner’s weight in the dance hall (or the bedroom!), then (if we’re also at least maintaining our bones and muscles at a healthy level) that’s good enough already.
Which prompts the question, what do you want to be able to do, now and years from now? What’s important to you?
For inspiration, check out: Train For The Event Of Your Life!
Take care!
Share This Post
Related Posts
-
Edamame vs Brussels Sprouts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing edamame to Brussels sprouts, we picked the edamame.
Why?
We were curious to see if something could unseat Brussels sprouts from the vegetable throne!
In terms of macros, edamame have more than 3x the protein and and nearly 50% more fiber, for the same amount of carbs. An easy win for edamame.
In the category of vitamins, edamame have more of vitamins B1, B2, B3, B5, B9, and choline, while Brussels sprouts have more of vitamins A, B6, C, E, and K, meaning a marginal 6:5 win for edamame this time.
When it comes to minerals, things are quite one-sided: edamame have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, and zinc, while Brussels sprouts have more selenium. Another easy win for edamame!
Adding up the sections makes it clear that edamame win the day, but of course, by all means, enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
What Do The Different Kinds Of Fiber Do? 30 Foods That Rank Highest
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Walnut, Apricot, & Sage Nut Roast
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s important to have at least one good nut roast recipe in your repertoire. It’s something that’s very good for making a good dish out of odds and ends that are in your house, and done well, it’s not only filling and nutritious, but a tasty treat too. Done badly, everyone knows the results can be unfortunate… Making this the perfect way to show off your skills!
You will need
- 1 cup walnuts
- ½ cup almonds
- ¼ cup whole mixed seeds (chia, pumpkin, & poppy are great)
- ¼ cup ground flax (also called flax meal)
- 1 medium onion, finely chopped
- 1 large carrot, grated
- 4 oz dried apricots, chopped
- 3 oz mushrooms, chopped
- 1 oz dried goji berries
- ½ bulb garlic, crushed
- 2 tbsp fresh sage, chopped
- 1 tbsp nutritional yeast
- 2 tsp dried rosemary
- 2 tsp dried thyme
- 2 tsp black pepper, coarse ground
- 1 tsp yeast extract (even if you don’t like it; trust us; it will work) dissolved in ¼ cup hot water
- ½ tsp MSG or 1 tsp low-sodium salt
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 350℉ / 180℃, and line a 2 lb loaf tin with baking paper.
2) Heat some oil in a skillet over a moderate heat, and fry the onion for a few minutes until translucent. Add the garlic, carrot, and mushrooms, cooking for another 5 minutes, stirring well. Set aside to cool a little once done.
3) Process the nuts in a food processor, pulsing until they are well-chopped but not so much that they turn into flour.
4) Combine the nuts, vegetables, and all the other ingredients in a big bowl, and mix thoroughly. If it doesn’t have enough structural integrity to be thick and sticky and somewhat standing up by itself if you shape it, add more ground flax. If it is too dry, add a little water but be sparing.
5) Spoon the mixture into the loaf tin, press down well (or else it will break upon removal), cover with foil and bake for 30 minutes. Remove the foil, and bake for a further 15 minutes, until firm and golden. When done, allow it to rest in the tin for a further 15 minutes, before turning it out.
6) Serve, as part of a roast dinner (roast potatoes, vegetables, gravy, etc).
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Why You Should Diversify Your Nuts!
- Chia Seeds vs Pumpkin Seeds – Which is Healthier?
- Apricots vs Peaches – Which is Healthier?
- Goji Berries: Which Benefits Do They Really Have?
- Ergothioneine: “The Longevity Vitamin” (That’s Not A Vitamin)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Book of Lymph – by Lisa Levitt Gainsely
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The book starts with an overview of what lymph is and why it matters, before getting into the main meat of the book, which is lymphatic massage techniques to improve lymphatic flow/drainage throughout different parts of the body, and in the context of an assortment of common maladies that may merit particular attention.
There’s an element of aesthetic medicine here, and improving beauty, but there’s also a whole section devoted to such things as breast care and the like (bearing in mind, the lymphatic system is one of our main defenses against cancer). There’s also a lot about managing lymph in the context of chronic health conditions.
The style is light pop-science; the science is explained clearly throughout, but without academic citations every few lines as some books might have. The author is, after all, a practitioner (CLT) and/but not an academic.
Bottom line: if you’d like to improve your lymphatic health, whether for beauty or health maintenance or recovery, this book will walk you through it.
Click here to check out The Book of Lymph, and give yours some love!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: