The 5 Love Languages Gone Wrong
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Levelling up the 5 love languages
The saying “happy wife; happy life” certainly goes regardless of gender, and if we’re partnered, it’s difficult to thrive in our individual lives if we’re not thriving as a couple. So, with the usual note that mental health is also just health, let’s take a look at getting beyond the basics of a well-known, often clumsily-applied model:
The 5 love languages
You’re probably familiar with “the 5 love languages”, as developed by Dr. Gary Chapman. If not, they are:
- Acts of Service
- Gift-Giving
- Physical Touch
- Quality Time
- Words of Affirmation
The idea is that we each weight these differently, and problems can arise when a couple are “speaking a different language”.
So, is this a basic compatibility test?
It doesn’t have to be!
We can, if we’re aware of each other’s primary love languages, make an effort to do a thing we wouldn’t necessarily do automatically, to ensure they’re loved the way they need to be.
But…
What a lot of people overlook is that we can also have different primary love languages for giving and for receiving. And, missing that can mean that even taking each other’s primarily love languages into account, efforts to make a partner feel loved, or to feel loved oneself, can miss 50% of the time.
For example, I (your writer here today, hi) could be asked my primary love language and respond without hesitation “Acts of Service!” because that’s my go-to for expressing love.
I’m the person who’ll run around bringing drinks, do all the housework, and without being indelicate, will tend towards giving in the bedroom. But…
A partner trying to act on that information to make me feel loved by giving Acts of Service would be doomed to catastrophic failure, because my knee-jerk reaction would be “No, here, let me do that for you!”
So it’s important for partners to ask each other…
- Not: “what’s your primary love language?” ❌
- But: “what’s your primary way of expressing love?” ✅
- And: “which love language makes you feel most loved?” ✅
For what it’s worth, I thrive on Words of Affirmation, so thanks again to everyone who leaves kind feedback on our articles! It lets me know I provided a good Act of Service
So far, so simple, right? You and your partner (or: other person! Because as we’ve just seen, these go for all kinds of dynamics, not just romantic partnerships) need to be aware of each other’s preferred love languages for giving and receiving.
But…
There’s another pitfall that many fall into, and that’s assuming that the other person has the same idea about what a given love language means, when there’s more to clarify.
For example:
- Acts of Service: is it more important that the service be useful, or that it took effort?
- Gift-Giving: is it better that a gift be more expensive, or more thoughtful and personal?
- Physical Touch: what counts here? If we’re shoulder-to-shoulder on the couch, is that physical touch or is something more active needed?
- Quality Time: does it count if we’re both doing our own thing but together in the same room, comfortable in silence together? Or does it need to be a more active and involved activity together? And is it quality time if we’re at a social event together, or does it need to be just us?
- Words of Affirmation: what, exactly, do we need to hear? For romantic partners, “I love you” can often be important, but is there something else we need to hear? Perhaps a “because…”, or perhaps a “so much that…”, or perhaps something else entirely? Does it no longer count if we have to put the words in our partner’s mouth, or is that just good two-way communication?
Bottom line:
There’s a lot more to this than a “What’s your love language?” click-through quiz, but with a little application and good communication, this model can really resolve a lot of would-be problems that can grow from feeling unappreciated or such. And, the same principles go just the same for friends and others as they do for romantic partners.
In short, it’s one of the keys to good interpersonal relationships in general—something critical for our overall well-being!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Red Cabbage vs Brussels Sprouts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing red cabbage to Brussels sprouts, we picked the sprouts.
Why?
First let’s note that we have an interesting comparison today, because these two plants are the exact same species (and indeed, also the exact same species as broccoli, cauliflower. and kale)—just a different cultivar. All of these plants and more are simply cultivars of Brassica oleracea.
Them being the same species notwithstanding, there are nutritional differences:
In terms of macros, the sprouts have more than 2x the protein, slightly more carbs, and nearly 2x the fiber. An easy win for sprouts here.
Looking at vitamins next, red cabbage has more vitamin A (whence the color), while Brussels sprouts have more of vitamins B1, B2, B3, B5, B6, B7, B9, C, E, K, and choline. Another easy win for sprouts.
In the category of minerals, red cabbage has a tiny bit more calcium, while Brussels sprouts have more copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc—while being literally just a few mg/100g behind red cabbage on calcium anyway. So, once again, sprouts are sweeping the victory.
Both vegetables are a rich source of assorted polyphenols; for most polyphenols, Brussels sprouts scores higher—an exception being that red cabbage is very slightly higher in quercetin. So, we’ll call this category a win for Brussels sprouts, too.
In short: enjoy both; diversity is great and so is pretty much any iteration of Brassica oleracea. Standing next to Brussels sprouts made red cabbage look bad, but we assure you that cabbage in general is a nutritional powerhouse, and in this case it was hot the heels of sprouts in most of those micronutrients. If you’re going to pick one though, the Brussels sprouts are indeed the more nutritionally dense.
Want to learn more?
You might like to read:
Sprout Your Seeds, Grains, Beans, Etc ← sprout your Brassica oleracea, too!
Take care!
Share This Post
-
The Best Kind Of Fiber For Overall Health?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Fiber Of Good Health
We’ve written before about how most people in industrialized nations in general, and N. America in particular, do not get nearly enough fiber:
Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
Fiber’s important for many aspects of health, not least of all the heart:
What Matters Most For Your Heart? Eat More (Of This) For Lower Blood Pressure
As well, of course, as being critical for gut health:
Gut Health 101: Making Friends With Your Gut (You Can Thank Us Later)
But is all fiber “prebiotic fiber”, and/or are some better than others?
Beta-glucan
A recent study (it’s a mouse study, but promising in its applicability for humans) examined the health impacts of 5 different fiber types:
- pectin
- β-glucan
- wheat dextrin
- resistant starch
- cellulose (control)
As for health metrics, they measured:
- body weight
- adiposity
- indirect calorimetry
- glucose tolerance
- gut microbiota
- metabolites thereof
What they found was…
❝Only β-glucan supplementation during HFD-feeding decreased adiposity and body weight gain and improved glucose tolerance compared with HFD-cellulose, whereas all other fibers had no effect. This was associated with increased energy expenditure and locomotor activity in mice compared with HFD-cellulose.
All fibers supplemented into an HFD uniquely shifted the intestinal microbiota and cecal short-chain fatty acids; however, only β-glucan supplementation increased cecal butyrate concentrations. Lastly, all fibers altered the small-intestinal microbiota and portal bile acid composition. ❞
If you’d like to read more, the study itself is here:
If you’d like to read less, the short version is that they are all good but β-glucan scored best in several metrics.
It also acts indirectly as a GLP-1 agonist, by the way:
The right fiber may help you lose weight
You may be wondering: what is β-glucan found in?
It’s found in many (non-animal product) foods, but oats, barley, mushrooms, and yeasts are all good sources.
Is it available as a supplement?
More or less; there are supplements that contain it generously, here’s an example product on Amazon, a cordyceps extract, of which >30% is β-glucan.
As an aside, cordyceps itself has many other healthful properties too:
Cordyceps: Friend Or Foe? ← the answer is, it depends! If you’re human, it’s a friend.
Enjoy!
Share This Post
-
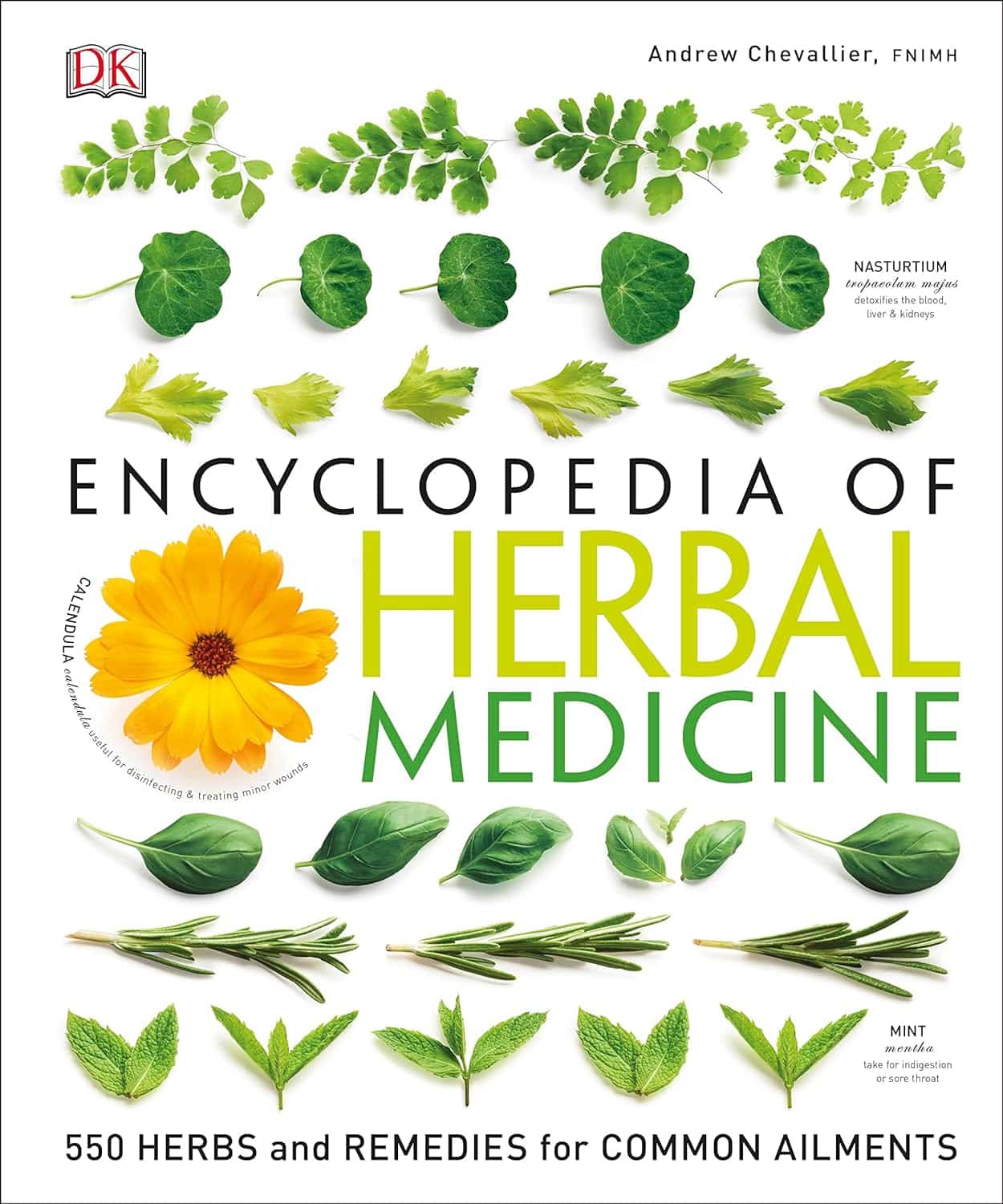
Encyclopedia Of Herbal Medicine – by Andrew Chevallier
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A common problem with a lot of herbal medicine is it’s “based on traditional use only”, while on the other hand, learning about the actual science of it can mean poring through stacks of Randomized Clinical Trials, half of which are paywalled.
This beautifully and clearly-illustrated book bridges that gap. It gives not just the history, but also the science, of the use of many medicinal herbs (spotlight on 100 key ones; details on 450 more).
It gives advice on growing, harvesting, processing, and using the herbs, as well as what not to do (with regard to safety). And in case you don’t fancy yourself a gardener, you’ll also find advice on places one can buy herbs, and what you’ll need to know to choose them well (controlling for quality etc).
You can read it cover-to-cover, or look up what you need by plant in its general index, or by ailment (200 common ailments listed). As for its bibliography, it does list many textbooks, but not individual papers—though it does cite 12 popular scientific journals too.
Bottom line: if you want a good, science-based, one-stop book for herbal medicine, this is a top-tier choice.
Click here to check out the Encyclopedia of Herbal Medicine, and expand your home remedy repertoire!
Share This Post
Related Posts
-
Psychoactive Drugs Are Having a Moment. The FDA Will Soon Weigh In.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Lori Tipton is among the growing number of people who say that MDMA, also known as ecstasy, saved their lives.
Raised in New Orleans by a mother with untreated bipolar disorder who later killed herself and two others, Tipton said she endured layers of trauma that eventually forced her to seek treatment for crippling anxiety and hypervigilance. For 10 years nothing helped, and she began to wonder if she was “unfixable.”
Then she answered an ad for a clinical trial for MDMA-assisted therapy to treat post-traumatic stress disorder. Tipton said the results were immediate, and she is convinced the drug could help a lot of people. But even as regulators weigh approval of the first MDMA-based treatment, she’s worried that it won’t reach those who need it most.
“The main thing that I’m always concerned about is just accessibility,” the 43-year-old nonprofit project manager said. “I don’t want to see this become just another expensive add-on therapy for people who can afford it when people are dying every day by their own hand because of PTSD.”
MDMA is part of a new wave of psychoactive drugs that show great potential for treating conditions such as severe depression and PTSD. Investors are piling into the nascent field, and a host of medications based on MDMA, LSD, psychedelic mushrooms, ketamine, the South American plant mixture ayahuasca, and the African plant ibogaine are now under development, and in some cases vying for approval by the Food and Drug Administration.
Proponents hope the efforts could yield the first major new therapies for mental illness since the introduction of modern antidepressants in the 1980s. But not all researchers are convinced that their benefits have been validated, or properly weighed against the risks. And they can be difficult to assess using traditional clinical trials.
The first MDMA-assisted assisted therapy appeared to be on track for FDA approval this August, but a recent report from an independent review committee challenged the integrity of the trial data from the drug’s maker, Lykos Therapeutics, a startup founded by a psychedelic research and advocacy group. The FDA will convene a panel of independent investigators on June 4 to determine whether to recommend the drug’s approval.
Proponents of the new therapies also worry that the FDA will impose treatment protocols, such as requiring multiple trained clinicians to monitor a patient for extended periods, that will render them far too expensive for most people.
Tipton’s MDMA-assisted therapy included three eight-hour medication sessions overseen by two therapists, each followed by an overnight stay at the facility and an integration session the following day.
“It does seem that some of these molecules can be administered safely,” said David Olson, director of the University of California-Davis Institute for Psychedelics and Neurotherapeutics. “I think the question is can they be administered safely at the scale needed to really make major improvements in mental health care.”
Breakthrough Therapies?
Psychedelics and other psychoactive substances, among the medicines with the oldest recorded use, have long been recognized for their potential therapeutic benefits. Modern research on them started in the mid-20th century, but clinical trial results didn’t live up to the claims of advocates, and they eventually got a bad name both from their use as party drugs and from rogue CIA experiments that involved dosing unsuspecting individuals.
The 1970 Controlled Substances Act made most psychoactive drugs illegal before any treatments were brought to market, and MDMA was classified as a Schedule 1 substance in 1985, which effectively ended any research. It wasn’t until 2000 that scientists at Johns Hopkins University were granted regulatory approval to study psilocybin anew.
Ketamine was in a different category, having been approved as an anesthetic in 1970. In the early 2000s, researchers discovered its antidepressant effects, and a ketamine-based therapy, Spravato, received FDA approval in 2019. Doctors can also prescribe generic ketamine off-label, and hundreds of clinics have sprung up across the nation. A clinical trial is underway to evaluate ketamine’s effectiveness in treating suicidal depression when used with other psychiatric medications.
Ketamine’s apparent effectiveness sparked renewed interest in the therapeutic potential of other psychoactive substances.
They fall into distinct categories: MDMA is an entactogen, also known as an empathogen, which induces a sense of connectedness and emotional communion, while LSD, psylocibin, and ibogaine are psychedelics, which create altered perceptual states. Ketamine is a dissociative anesthetic, though it can produce hallucinations at the right dose.
Despite the drugs’ differences, Olson said they all create neuroplasticity and allow the brain to heal damaged neural circuits, which imaging shows can be shriveled up in patients with addiction, depression, and PTSD.
“All of these brain conditions are really disorders of neural circuits,” Olson said. “We’re basically looking for medicines that can regrow these neurons.”
Psychedelics are particularly good at doing this, he said, and hold promise for treating diseases including Alzheimer’s.
A number of psychoactive drugs have now received the FDA’s “breakthrough therapy” designation, which expedites development and review of drugs with the potential to treat serious conditions.
But standard clinical trials, in which one group of patients is given the drug and a control group is given a placebo, have proven problematic, for the simple reason that people have no trouble determining whether they’ve gotten the real thing.
The final clinical trial for Lykos’ MDMA treatment showed that 71% of participants no longer met the criteria for PTSD after 18 weeks of taking the drug versus 48% in the control group.
A March report by the Institute for Clinical and Economic Review, an independent research group, questioned the company’s clinical trial results and challenged the objectivity of MDMA advocates who participated in the study as both patients and therapists. The institute also questioned the drug’s cost-effectiveness, which insurers factor into coverage decisions.
Lykos, a public benefit company, was formed in 2014 as an offshoot of the Multidisciplinary Association for Psychedelic Studies, a nonprofit that has invested more than $150 million into psychedelic research and advocacy.
The company said its researchers developed their studies in partnership with the FDA and used independent raters to ensure the reliability and validity of the results.
“We stand behind the design and results of our clinical trials,” a Lykos spokesperson said in an email.
There are other hazards too. Psychoactive substances can put patients in vulnerable states, making them potential victims for financial exploitation or other types of abuse. In Lykos’ second clinical trial, two therapists were found to have spooned, cuddled, blindfolded, and pinned down a female patient who was in distress.
The substances can also cause shallow breathing, heart issues, and hyperthermia.
To mitigate risks, the FDA can put restrictions on how drugs are administered.
“These are incredibly potent molecules and having them available in vending machines is probably a bad idea,” said Hayim Raclaw of Negev Capital, a venture capital fund focused on psychedelic drug development.
But if the protocols are too stringent, access is likely to be limited.
Rachel del Dosso, a trauma therapist in the greater Los Angeles area who offers ketamine-assisted therapy, said she’s been following the research on drugs like MDMA and psilocybin and is excited for their therapeutic potential but has reservations about the practicalities of treatment.
“As a therapist in clinical practice, I’ve been thinking through how could I make that accessible,” she said. “Because it would cost a lot for [patients] to have me with them for the whole thing.”
Del Dosso said a group therapy model, which is sometimes used in ketamine therapy, could help scale the adoption of other psychoactive treatments, too.
Artificial Intelligence and Analogs
Researchers expect plenty of new discoveries in the field. One of the companies Negev has invested in, Mindstate Design Labs, uses artificial intelligence to analyze “trip reports,” or self-reported drug experiences, to identify potentially therapeutic molecules. Mindstate has asked the FDA to green-light a clinical trial of the first molecule identified through this method, 5-MeO-MiPT, also known as moxy.
AlphaFold, an AI program developed by Google’s DeepMind, has identified thousands of potential psychedelic molecules.
There’s also a lot of work going into so-called analog compounds, which have the therapeutic effects of hallucinogens but without the hallucinations. The maker of a psilocybin analog announced in March that the FDA had granted it breakthrough therapy status.
“If you can harness the neuroplasticity-promoting properties of LSD while also creating an antipsychotic version of it, then that can be pretty powerful,” Olson said.
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Get The Right Help For Your Pain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How Much Does It Hurt?
Sometimes, a medical professional will ask us to “rate your pain on a scale of 1–10”.
It can be tempting to avoid rating one’s pain too highly, because if we say “10” then where can we go from there? There is always a way to make pain worse, after all.
But that kind of thinking, however logical, is folly—from a practical point of view. Instead of risking having to give an 11 later, you have now understated your level-10 pain as a “7” and the doctor thinks “ok, I’ll give Tylenol instead of morphine”.
A more useful scale
First, know this:
Zero is not “this is the lowest level of pain I get to”.
Zero is “no pain”.
As for the rest…
- My pain is hardly noticeable.
- I have a low level of pain; I am aware of my pain only when I pay attention to it.
- My pain bothers me, but I can ignore it most of the time.
- I am constantly aware of my pain, but can continue most activities.
- I think about my pain most of the time; I cannot do some of the activities I need to do each day because of the pain.
- I think about my pain all of the time; I give up many activities because of my pain.
- I am in pain all of the time; It keeps me from doing most activities.
- My pain is so severe that it is difficult to think of anything else. Talking and listening are difficult.
- My pain is all that I can think about; I can barely move or talk because of my pain.
- I am in bed and I can’t move due to my pain; I need someone to take me to the emergency room because of my pain.
10almonds tip: are you reading this on your phone? Screenshot the above, and keep it for when you need it!
One extra thing to bear in mind…
Medical staff will be more likely to believe a pain is being overstated, on a like-for-like basis, if you are a woman, or not white, or both.
There are some efforts to compensate for this:
A new government inquiry will examine women’s pain and treatment. How and why is it different?
Some other resources of ours:
- The 7 Approaches To Pain Management ← a pain specialist discusses the options available
- Managing Chronic Pain (Realistically!) ← when there’s no quick fix, but these things can buy you some hours’ relief at least / stop the pain from getting worse in the moment
- Science-Based Alternative Pain Relief ← for when you’re maxxed out on painkillers, and need something more/different, these are the things the science says will work
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Self-Compassion – by Dr. Kristin Neff
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of people struggle with self-esteem, and depending on one’s surrounding culture, it can even seem socially obligatory to be constantly valuing oneself highly (or else, who else will if we do not?). But, as Dr. Neff points out, there’s an inherent problem with reinforcing for oneself even a positive message like “I am smart, strong, and capable!” because sometimes all of us have moments of being stupid, weak, and incapable (occasionally all three at once!), which places us in a position of having to choose between self-deceit and self-deprecation, neither of which are good.
Instead, Dr. Neff advocates for self-compassion, for treating oneself as one (hopefully) would a loved one—seeing their/our mistakes, weaknesses, failures, and loving them/ourself anyway.
She does not, however, argue that we should accept just anything from ourselves uncritically, but rather, we identify our mistakes, learn, grow, and progress. So not “I should have known better!”, nor even “How was I supposed to know?!”, but rather, “Now I have learned a thing”.
The style of the book is quite personal, as though having a heart-to-heart over a hot drink perhaps, but the format is organized and progresses naturally from one idea to the next, taking the reader to where we need to be.
Bottom line: if you have trouble with self-esteem (as most people do), then that’s a trap that there is a way out of, and it doesn’t require being perfect or lowering one’s standards, just being kinder to oneself along the way—and this book can help inculcate that.
Click here to check out Self-Compassion, and indeed be kind to yourself!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: