Where Nutrition Meets Habits!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Where Nutrition Meets Habits…
This is Claudia Canu, MSc., INESEM. She’s on a mission to change the way we eat:
Often, diet is a case of…
- Healthy
- Easy
- Cheap
(choose two)
She wants to make it all three, and tasty too. She has her work cut out for her, but she’s already blazed quite a trail personally:
❝Nine months before turning 40 years old, I set a challenge for myself: Arrive to the day I turn 40 as the best possible version of myself, physically, mentally and emotionally.❞
~ Claudia Canu
In Her Own Words: My Journey To My Healthy 40s
And it really was quite a journey:
- September: Changes That Destabilize
- October: Looking for Focus
- November: New Habits
- December: Analyzing The First Results
- January: Traveling & Perfectionism
- February: Habits & Goals
- March: Connection, Cravings, & Organization
- April: Physical & Emotional Changes After 7 Months
- May: Reflections & Considerations
- June: Challenge Is Over
For those of us who’d like the short-cut rather than a nine-month quasi-spiritual journey… based on both her experience, and her academic and professional background in nutrition, her main priorities that she settled on were:
- Making meals actually nutritionally balanced, which meant re-thinking what she thought a meal “should” be
- Making nutritionally balanced meals that didn’t require a lot of skill and/or resources
- That’s it!
But, easier said than done… Where to begin?
She shares an extensive list of recipes, from meals to snacks (I thought I was the only one who made coffee overnight oats!), but the most important thing from her is:
Claudia’s 10 Guiding Principles:
- Buy only fresh ingredients that you are going to cook yourself. If you decide to buy pre-cooked ones, make sure they do not have added ingredients, especially sugar (in all its forms).
- Use easy and simple cooking methods.
- Change ingredients every time you prepare your meals.
- Prepare large quantities for three or four days.
- Store the food separately in tightly closed Tupperware.
- Organize yourself to always have ready-to-eat food in the fridge.
- When hungry, mix the ingredients in the ideal amounts to cover the needs of your body.
- Chew well and take the time to taste your food.
- Eat foods that you like and enjoy.
- Do not overeat but don’t undereat either.
We have only two quibbles with this fine list, which are:
About Ingredients!
Depending on what’s available around you, frozen and/or tinned “one-ingredient” foods can be as nutritional as (if not more nutritional than) fresh ones. By “one-ingredient” foods here we mean that if you buy a frozen pack of chopped onions, the ingredients list will be: “chopped onions”. If you buy a tin of tomatoes, the ingredients will say “Tomatoes” or at most “Tomatoes, Tomato Juice”, for example.
She does list the ingredients she keeps in; the idea that with these in the kitchen, you’ll never be in the position of “oh, we don’t have much in, I guess it’s a pizza delivery night” or “well there are some chicken nuggets at the back of the freezer”.
Check Out And Plan: 10 Types Of Ingredients You Should Always Keep In Your Kitchen
Here Today, Gone Tomorrow?
Preparing large quantities for three or four days can result in food for one or two days if the food is unduly delicious
But! Claudia has a remedy for that:
Read: How To Eliminate Food Cravings And What To Do When They Win
Anyway, there’s a wealth of resources in the above-linked pages, so do check them out!
Perhaps the biggest take-away is to ask yourself:
“What are my guiding principles when it comes to food?”
If you don’t have a ready answer, maybe it’s time to tackle that—whether Claudia’s way or your own!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
‘Free birthing’ and planned home births might sound similar but the risks are very different
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The death of premature twins in Byron Bay in an apparent “wild birth”, or free birth, last week has prompted fresh concerns about giving birth without a midwife or medical assistance.
This follows another case from Victoria this year, where a baby was born in a critical condition following a reported free birth.
It’s unclear how common free birthing is, as data is not collected, but there is some evidence free births increased during the COVID pandemic.
Planned home births also became more popular during the pandemic, as women preferred to stay away from hospitals and wanted their support people with them.
But while free births and home births might sound similar, they are a very different practice, with free births much riskier. So what’s the difference, and why might people opt for a free birth?
What are home births?
Planned home births involve care from midwives, who are registered experts in childbirth, in a woman’s home.
These registered midwives work privately, or are part of around 20 publicly funded home birth programs nationally that are attached to hospitals.
They provide care during the pregnancy, labour and birth, and in the first six weeks following the birth.
The research shows that for women with low risk pregnancies, planned home births attended by competent midwives (with links to a responsive mainstream maternity system) are safe.
Home births result in less intervention than hospital births and women perceive their experience more positively.
What are free births?
A free birth is when a woman chooses to have a baby, usually at home, without a registered health professional such as a midwife or doctor in attendance.
Different terms such as unassisted birth or wild pregnancy or birth are also used to refer to free birth.
The parents may hire an unregulated birth worker or doula to be a support at the birth but they do not have the training or medical equipment needed to manage emergencies.
Women may have limited or no health care antenatally, meaning risk factors such as twins and breech presentations (the baby coming bottom first) are not detected beforehand and given the right kind of specialist care.
Why do some people choose to free birth?
We have been studying the reasons women and their partners choose to free birth for more than a decade. We found a previous traumatic birth and/or feeling coerced into choices that are not what the woman wants were the main drivers for avoiding mainstream maternity care.
Australia’s childbirth intervention rates – for induction or augmentation of labour, episiotomy (cutting the tissue between the vaginal opening and the anus) and caesarean section – are comparatively high.
One in ten women report disrespectful or abusive care in childbirth and some decide to make different choices for future births.
Lack of options for a natural birth and birth choices such as home birth or birth centre birth also played a major role in women’s decision to free birth.
Publicly funded home birth programs have very strict criteria around who can be accepted into the program, excluding many women.
In other countries such as the United Kingdom, Netherlands and New Zealand, publicly funded home births are easier to access.
It can be difficult to access home birth services in Australia.
Ink Drop/ShutterstockOnly around 200 midwives provide private midwifery services for home births nationally. Private midwives are yet to obtain insurance for home births, which means they are risking their livelihoods if something goes wrong and they are sued.
The cost of a home birth with a private midwife is not covered by Medicare and only some health funds rebate some of the cost. This means women can be out of pocket A$6-8,000.
Access to home birth is an even greater issue in rural and remote Australia.
How to make mainstream care more inclusive
Many women feel constrained by their birth choices in Australia. After years of research and listening to thousands of women, it’s clear more can be done to reduce the desire to free birth.
As my co-authors and I outline in our book, Birthing Outside the System: The Canary in the Coal Mine, this can be achieved by:
- making respectful care a reality so women aren’t traumatised and alienated by maternity care and want to engage with it
- supporting midwifery care. Women are seeking more physiological and social ways of birthing, minimising birth interventions, and midwives are the experts in this space
- supporting women’s access to their chosen place of birth and model of care and not limiting choice with high out-of-pocket expenses
- providing more flexible, acceptable options for women experiencing risk factors during pregnancy and/or birth, such as having a previous caesarean birth, having twins or having a baby in breech position. Women experiencing these complications experience pressure to have a caesarean section
- getting the framework right with policies, guidelines, education, research, regulation and professional leadership.
Ensuring women’s rights and choices are informed and respected means they’re less likely to feel they’re left with no other option.
Hannah Dahlen, Professor of Midwifery, Associate Dean Research and HDR, Midwifery Discipline Leader, Western Sydney University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
How Exercise Rewires Your Brain for Better Mental Wellbeing
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Tracey Marks, psychiatrist, explains what happens immediately, and what happens over the long term:
For now and for later
First of all, a single workout can already alter brain chemistry and protect against stress. In the longer term, exercise promotes neurogenesis, primarily in the hippocampus, improving memory and reversing brain aging. It also strengthens the prefrontal cortex, which is critical for decision-making, focus, and emotional regulation.
In more general terms, exercise boosts brain-derived neurotrophic factor (BDNF) levels, which in turn boost neuron growth and connectivity.
Exercise also promotes angiogenesis (blood vessel construction), improving oxygen and nutrient delivery to the brain.
Timeline of benefits:
- Immediate: increased blood flow and temporary BDNF spike.
- Weeks: new neurons, connections, and blood vessel growth.
- Months: visible brain volume changes and better brain connectivity.
Dr. Marks’ Timing Tips
- Morning: boosts energy and helps regulate the circadian rhythm.
- Midday: resets stress levels (specifically: to low)
- Evening: helps process emotions (but it’s still recommended to avoid high-intensity exercise close to bedtime)
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Wondering what kind of exercise is best?
You might also like to read:
The Neuroscientist In The Gym: Dr. Wendy Suzuki Explains The Exercise That Protects Your Brain
Take care!
Share This Post
-
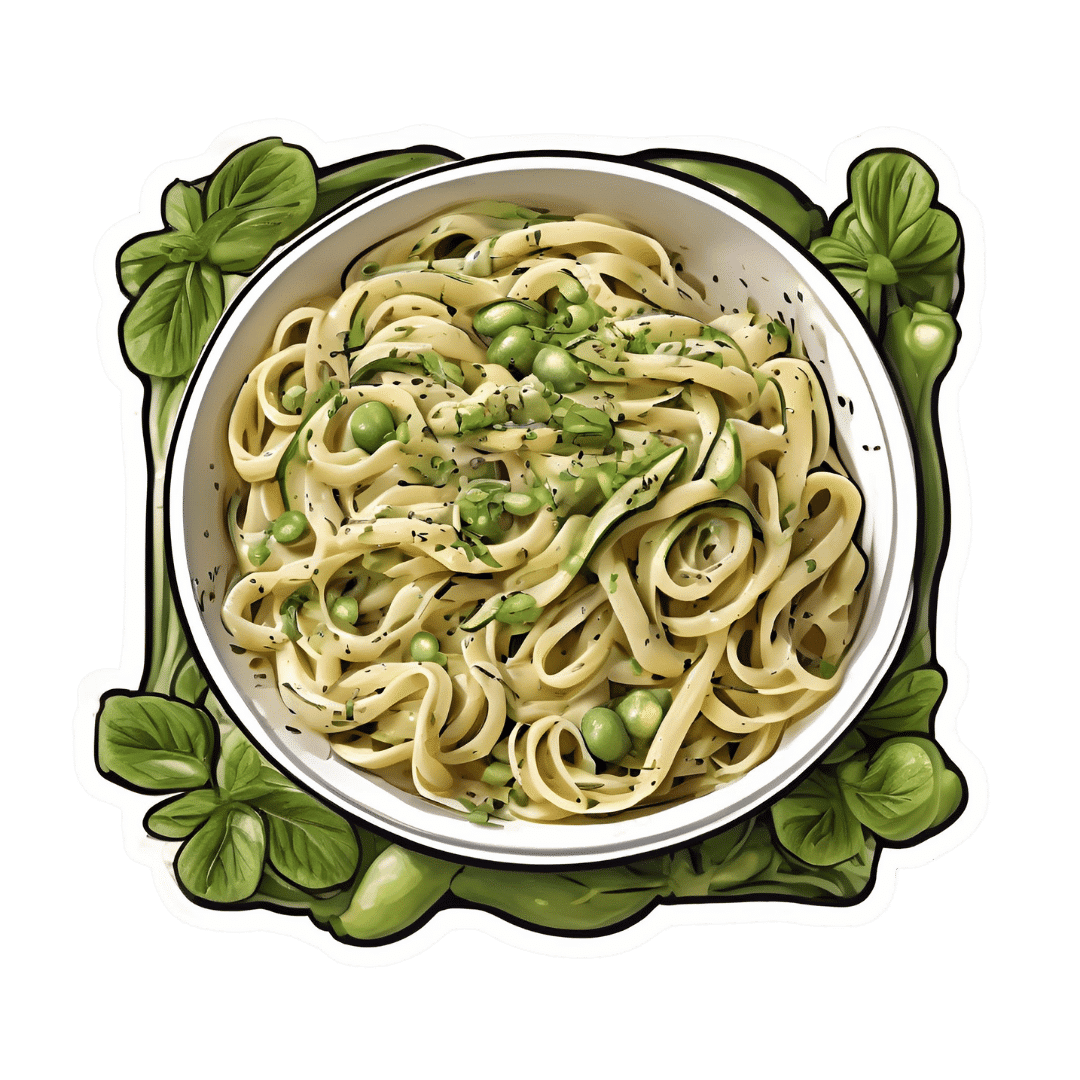
Creamy Zucchini, Edamame, & Asparagus Linguine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Protein, fiber, and polyphenols are the dish of the day here:
You will need
- 1½ cups milk (your choice what kind; we recommend soy for its neutral taste, though hazelnut’s nutty flavor would also work in this recipe)
- 6 oz wholegrain linguine (or your pasta of choice)
- 2 zucchini, thinly sliced
- 5 oz edamame beans (frozen is fine)
- 5 oz asparagus tips, cut into 2″ lengths
- ½ bulb garlic, crushed
- 1 tbsp chia seeds
- 1 small handful arugula
- 1 small handful parsley, chopped
- A few mint leaves, chopped
- Juice of ½ lemon
- 2 tsp black pepper, coarse ground
- ½ tsp MSG or 1 tsp low-sodium salt
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Heat some oil in a sauté pan or similar, over a low to medium heat. Add the zucchini and cook for 5 minutes until they start to soften.
2) Add the garlic and continue cooking for 1 minute, stirring gently.
3) Add the milk, bring to the boil, and add the past, chia seeds (the resistant starch from the pasta will help thicken the sauce, as will the chia seeds), and MSG or salt.
4) Reduce the heat, cover, and simmer for 8 minutes.
5) Add the edamame beans and asparagus, and cook for a further 2 minutes, or until the pasta is cooked but still firm to the bite. The sauce should be quite thick now.
6) Stir in the remaining ingredients and serve, adding a garnish if you wish.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- The Many Health Benefits Of Garlic
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- If You’re Not Taking Chia, You’re Missing Out
Take care!
Share This Post
Related Posts
-
Metabolic Health Roadmap – by Brenda Wollenberg
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The term “roadmap” is often used in informative books, but in this case, Wollenberg (a nutritionist with decades of experience) really does deliver what can very reasonably be described as a roadmap:
She provides chapters in the form of legs of a journey [to better metabolic health], and those legs are broadly divided into an “information center” to deliver new information, a “rest stop” for reflection, “roadwork” to guide the reader through implementing the information we just learned, in a practical fashion, and finally “traveller assistance” to give additional support / resources, as well as any potential troubleshooting, etc.
The information and guidance within are all based on very good science; a lot is what you will have read already about blood sugar management (generally the lynchpin of metabolic health in general), but there’s also a lot about leveraging epigenetics for our benefit, rather than being sabotaged by such.
There’s a little guidance that falls outside of nutrition (sleep, exercise, etc), but for the most part, Wollenberg stays within her own field of expertise, nutrition.
The style is idiosyncratic; it’s very clear that her goal is providing the promised roadmap, and not living up to any editor’s wish or publisher’s hope of living up to industry standard norms of book formatting. However, this pays off, because her delivery is clear and helpful while remaining personable and yet still bringing just as much actual science, and this makes for a very pleasant and informative read.
Bottom line: if you’d like to improve your metabolic health, as well as get held-by-the-hand through your health-improvement journey by a charming guide, this is very much the book for you!
Click here to check out the Metabolic Health Roadmap, and start taking steps!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
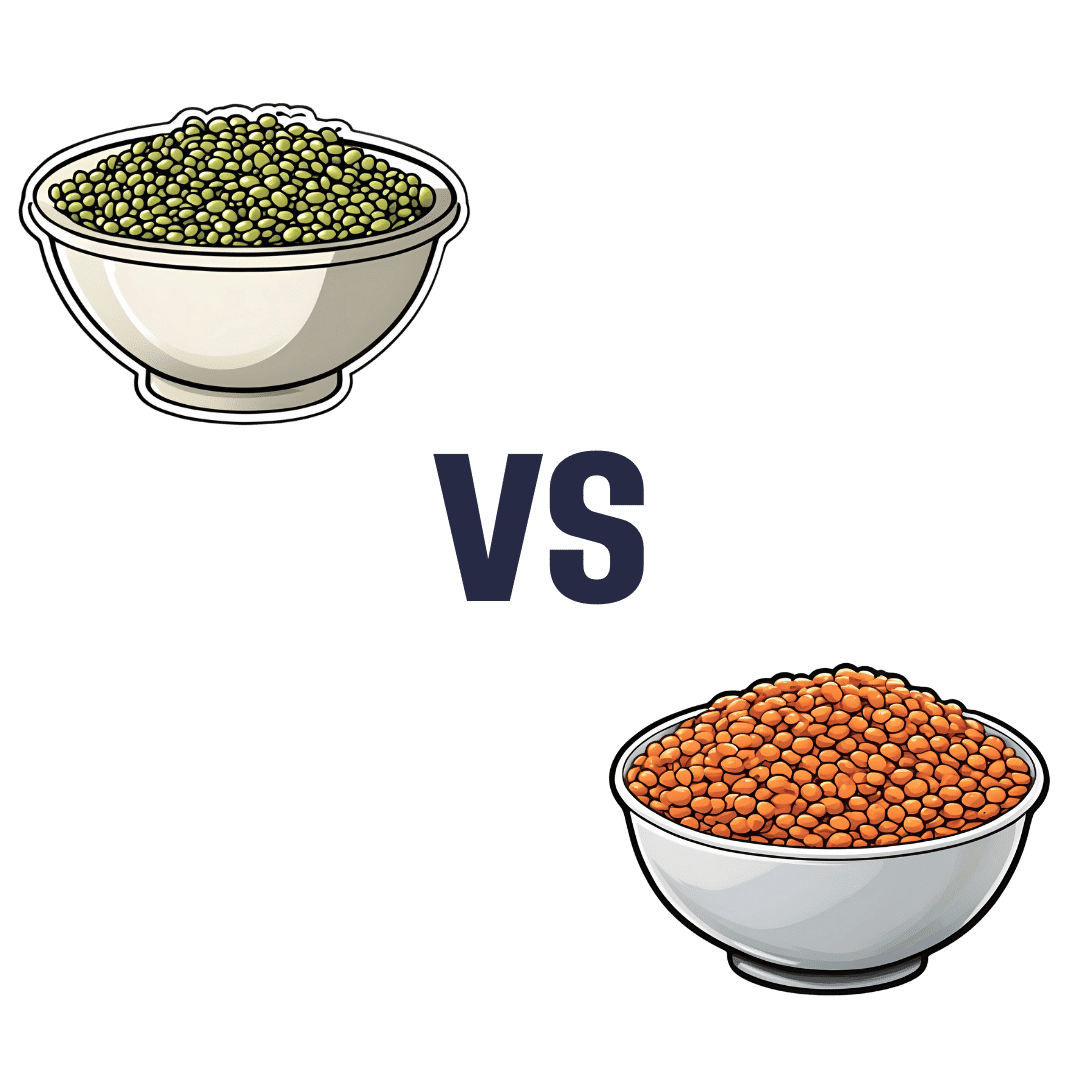
Mung Beans vs Red Lentils – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing mung beans to red lentils, we picked the lentils.
Why?
Both are great! But the lentils win on overall nutritional density.
In terms of macros, they have approximately the same carbs and fiber, and are both low glycemic index foods. The deciding factor is that the lentils have slightly more protein—but it’s not a huge difference; both are very good sources of protein.
In the category of vitamins, mung beans have more of vitamins A, E, and K, while red lentils have more of vitamins B1, B2, B3, B5, B6, B9, C, and choline. An easy win for lentils.
When it comes to minerals, again both are great, but mung beans have more calcium and magnesium (hence the green color) while red lentils have more copper, iron, manganese, phosphorus, potassium, selenium, and zinc. Another clear win for lentils.
Polyphenols are also a worthy category to note here; both have plenty, but red lentils have more, especially flavonols, anthocyanidins, proanthocyanidins, and anthocyanins (whence the red color).
In short: enjoy both, because diversity is almost always best. But if you’re picking one, red lentils are the most nutritious of the two.
Want to learn more?
You might like to read:
Sprout Your Seeds, Grains, Beans, Etc
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
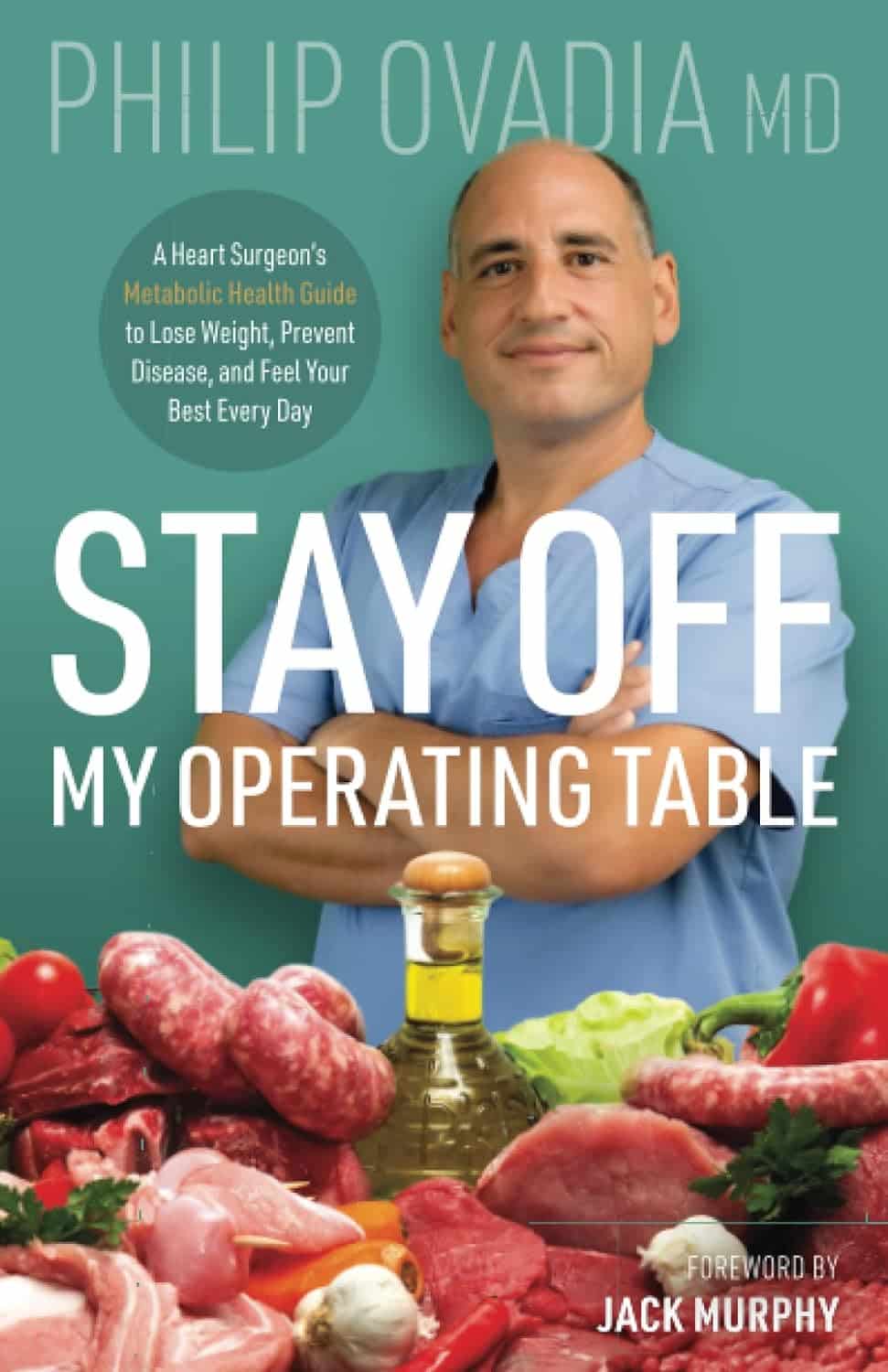
Stay off My Operating Table – by Dr. Philip Ovadia
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
With heart disease as the #1 killer worldwide, and 88% of adults being metabolically unhealthy (leading cause of heart disease), this is serious!
Rather than taking a “quick fix” advise-and-go approach, Dr. Ovadia puts the knowledge and tools in our hands to do better in the long term.
As a heart surgeon himself, his motto here is:
❝What foods to put on your table so you don’t end up on mine❞
There’s a lot more to this book than the simple “eat the Mediterranean diet”:
- While the Mediterranean diet is generally considered the top choice for heart health, he also advises on how to eat healthily on all manner of diets… Carnivore, Keto, Paleo, Atkins, Gluten-Free, Vegan, you-name-it.
- A lot of the book is given to clearing up common misconceptions, things that sounded plausible but are just plain dangerous. This information alone is worth the price of the book, we think.
- There’s also a section given over to explaining the markers of metabolic health, so you can monitor yourself effectively
- Rather than one-size-fits-all, he also talks about common health conditions and medications that may change what you need to be doing
- He also offers advice about navigating the health system to get what you need—including dealing with unhelpful doctors!
Bottom line: A very comprehensive (yet readable!) manual of heart health.
Get your copy of Stay Off My Operating Table from Amazon today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: