Radical CBT
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Radical Acceptance!
A common criticism of Cognitive Behavioral Therapy (CBT) is that much of it hinges on the following process:
- You are having bad feelings
- Which were caused by negative automatic thoughts
- Which can be taken apart logically
- Thus diffusing the feelings
- And then feeling better
For example:
- I feel like I’m an unwanted burden to my friend
- Because he canceled on me today
- But a reasonable explanation is that he indeed accidentally double-booked himself and the other thing wasn’t re-arrangeable
- My friend is trusting me to be an understanding friend myself, and greatly values my friendship
- I feel better and look forward to our next time together
But what if the negative automatic thoughts are, upon examination, reasonable?
Does CBT argue that we should just “keep the faith” and go on looking at a cruel indifferent world through rose-tinted spectacles?
Nope, there’s a back-up tool.
This is more talked-about in Dialectic Behavior Therapy (DBT), and is called radical acceptance:
Click Here If The Embedded Video Doesn’t Load automatically!
Radical acceptance here means accepting the root of things as true, and taking the next step from there. It follows a bad conclusion with “alright, and now what?”
“But all evidence points to the fact that my friend has been avoiding me for months; I really can’t ignore it or explain it away any longer”
“Alright. Now what?”
- Maybe there’s something troubling your friend that you don’t know about (have you asked?)
- Maybe that something is nothing to do with you (or maybe it really is about you!)
- Maybe there’s a way you and he can address it together (how important is it to you?)
- Maybe it’s just time to draw a line under it and move on (with or without him)
Whatever the circumstances, there’s always a way to move forwards.
Feelings are messengers, and once you’ve received and processed the message, the only reason to keep feeling the same thing, is if you want to.
Note that this is true even when you know with 100% certainty that the Bad Thing™ is real and exactly as-imagined. It’s still possible for you to accept, for example:
“Alright, so this person really truly hates me. Damn, that sucks; I think I’ve been nothing but nice to them. Oh well. Shit happens.”
Feel all the feelings you need to about it, and then decide for yourself where you want to go from there.
Get: 25 CBT Worksheets To Help You Find Solutions To A Wide Variety of Problems
Recognizing Emotions
We talked in a previous edition of 10almonds’ Psychology Sunday about how an important part of dealing with difficult emotions is recognizing them as something that you experience, rather than something that’s intrinsically “you”.
But… How?
One trick is to just mentally (or out loud, if your current environment allows for such) greet them when you notice them:
- Hello again, Depression
- Oh, hi there Anxiety, it’s you
- Nice of you to join us, Anger
Not only does this help recognize and delineate the emotion, but also, it de-tooths it and recognizes it for what it is—something that doesn’t actually mean you any harm, but that does need handling.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Toxic Gas That Sterilizes Medical Devices Prompts Safety Rule Update
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Over the past two years, Madeline Beal has heard frustration and even bewilderment during public meetings about ethylene oxide, a cancer-causing gas that is used to sterilize half of the medical devices in the U.S.
Beal, senior risk communication adviser for the Environmental Protection Agency, has fielded questions about why the agency took so long to alert people who live near facilities that emit the chemical about unusually high amounts of the carcinogenic gas in their neighborhoods. Residents asked why the EPA couldn’t close those facilities, and they wanted to know how many people had developed cancer from their exposure.
“If you’re upset by the information you’re hearing tonight, if you’re angry, if it scares you to think about risk to your family, those are totally reasonable responses,” Beal told an audience in Laredo, Texas, in September 2022. “We think the risk levels near this facility are too high.”
There are about 90 sterilizing plants in the U.S. that use ethylene oxide, and for decades companies used the chemical to sterilize medical products without drawing much attention. Many medical device-makers send their products to the plants to be sterilized before they are shipped, typically to medical distribution companies.
But people living around these facilities have been jolted in recent years by a succession of warnings about cancer risk from the federal government and media reports, an awareness that has also spawned protests and lawsuits alleging medical harm.
The EPA is expected to meet a March 1 court-ordered deadline to finalize tighter safety rules around how the toxic gas is used. The proposed changes come in the wake of a 2016 agency report that found that long-term exposure to ethylene oxide is more dangerous than was previously thought.
But the anticipated final rules — the agency’s first regulatory update on ethylene oxide emissions in more than a decade — are expected to face pushback. Medical device-makers worry stricter regulation will increase costs and may put patients at higher risk of infection from devices, ranging from surgical kits to catheters, due to deficient sterilization. The new rules are also not likely to satisfy the concerns of environmentalists or members of the public, who already have expressed frustration about how long it took the federal government to sound the alarm.
“We have been breathing this air for 40 years,” said Connie Waller, 70, who lives with her husband, David, 75, within two miles of such a sterilizing plant in Covington, Georgia, east of Atlanta. “The only way to stop these chemicals is to hit them in their pocketbook, to get their attention.”
The EPA says data shows that long-term exposure to ethylene oxide can increase the risk of breast cancer and cancers of the white blood cells, such as non-Hodgkin lymphoma, myeloma, and lymphocytic leukemia. It can irritate the eyes, nose, throat, and lungs, and has been linked to damage to the brain and nervous and reproductive systems. Children are potentially more vulnerable, as are workers routinely exposed to the chemical, EPA officials say. The agency calculates the risk based on how much of the gas is in the air or near the sterilizing facility, the distance a person is from the plant, and how long the person is exposed.
Waller said she was diagnosed with breast cancer in 2004 and that her husband was found to have non-Hodgkin lymphoma eight years later.
A 2022 study of communities living near a sterilization facility in Laredo found the rates of acute lymphocytic leukemia and breast cancer were greater than expected based on statewide rates, a difference that was statistically significant.
Beal, the EPA risk adviser, who regularly meets with community members, acknowledges the public’s concerns. “We don’t think it’s OK for you to be at increased risk from something that you have no control over, that’s near your house,” she said. “We are working as fast as we can to get that risk reduced with the powers that we have available to us.”
In the meantime, local and state governments and industry groups have scrambled to defuse public outcry.
Hundreds of personal injury cases have been filed in communities near sterilizing plants. In 2020, New Mexico’s then-attorney general filed a lawsuit against a plant in Santa Teresa, and that case is ongoing. In a case that settled last year in suburban Atlanta, a company agreed to pay $35 million to 79 people who alleged ethylene oxide used at the plant caused cancer and other injuries.
In Cook County, Illinois, a jury in 2022 awarded $363 million to a woman who alleged exposure to ethylene oxide gas led to her breast cancer diagnosis. But, in another Illinois case, a jury ruled that the sterilizing company was not liable for a woman’s blood cancer claim.
Greg Crist, chief advocacy officer for the Advanced Medical Technology Association, a medical device trade group that says ethylene oxide is an effective and reliable sterilant, attributes the spate of lawsuits to the litigious nature of trial attorneys.
“If they smell blood in the water, they’ll go after it,” Crist said.
Most states have at least one sterilizing plant. According to the EPA, a handful, like California and North Carolina, have gone further than the agency and the federal Clean Air Act to regulate ethylene oxide emissions. After a media and political firestorm raised awareness about the metro Atlanta facilities, Georgia started requiring sterilizing plants that use the gas to report all leaks.
The proposed rules the EPA is set to finalize would set lower emissions limits for chemical plants and commercial sterilizers and increase some safety requirements for workers within these facilities. The agency is expected to set an 18-month deadline for commercial sterilizers to come into compliance with the emissions rules.
That would help at facilities that “cut corners,” with lax pollution controls that allow emissions of the gas into nearby communities, said Richard Peltier, a professor of environmental health sciences at the University of Massachusetts-Amherst. Stronger regulation also prevents the plants from remaining under the radar. “One of the dirty secrets is that a lot of it is self-regulated or self-policed,” Peltier added.
But the proposed rules did not include protections for workers at off-site warehouses that store sterilized products, which can continue to emit ethylene oxide. They also did not require air testing around the facilities, prompting debate about how effective they would be in protecting the health of nearby residents.
Industry officials also don’t expect an alternative that is as broadly effective as ethylene oxide to be developed anytime soon, though they support researching other methods. Current alternatives include steam, radiation, and hydrogen peroxide vapor.
Increasing the use of alternatives can reduce industry dependence on “the crutch of ethylene oxide,” said Darya Minovi, senior analyst with the Union of Concerned Scientists, an advocacy group.
But meeting the new guidelines will be disruptive to the industry, Crist said. He estimates companies will spend upward of $500 million to comply with the new EPA rules and could struggle to meet the agency’s 18-month timetable. Sterilization companies will also have difficulty adjusting to new rules on how workers handle the gas without a dip in efficiency, Crist said.
The Food and Drug Administration, which regulates drugs and medical devices, is also watching the regulatory moves closely and worries the updated emissions rule could “present some unique challenges” if implemented as proposed, said Audra Harrison, an FDA spokesperson. “The FDA is concerned about the rule’s effects on the availability of medical devices,” she added.
Other groups, like the American Chemistry Council and the Texas Commission on Environmental Quality, the state’s environmental agency, assert that ethylene oxide use isn’t as dangerous as the EPA says. The EPA’s toxicity assessment has “severe flaws” and is “overly conservative,” the council said in an emailed statement. Texas, which has several sterilizing plants, has said ethylene oxide isn’t as high a cancer risk as the agency claims, an assessment that the EPA has rejected.
Tracey Woodruff, a researcher at the University of California-San Francisco who previously worked at the EPA, said it can be hard for the agency to keep up with regulating chemicals like ethylene oxide because of constrained resources, the technical complications of rulemaking, and industry lobbying.
But she’s hopeful the EPA can strike a balance between its desire to reduce exposure and the desire of the FDA not to disrupt medical device sterilization. And scrutiny can also help the device sterilization industry think outside the box.
“We continue to discover these chemicals that we’ve already been exposed to were toxic, and we have high exposures,” she said. “Regulation is an innovation forcer.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
12 Questions For Better Brain Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We usually preface our “Expert Insights” pieces with a nice banner that has a stylish tall cutout that allows us to put a photo of the expert in. Today we’re not doing that, because for today’s camera-shy expert, we could only find one photo, and it’s a small, grainy, square headshot that looks like it was taken some decades ago, and would not fit our template at all. You can see it here, though!
In any case, Dr. Linda Selwa is a neurologist and neurophysiologist with nearly 40 years of professional experience.
The right questions to ask
As a neurologist, she found that one of the problems that results in delayed interventions (and thus, lower efficacy of those interventions) is that people don’t know there’s anything to worry about until a degenerative brain condition has degenerated past a certain point. With that in mind, she bids us ask ourselves the following questions, and discuss them with our primary healthcare providers as appropriate:
- Sleep: Are you able to get sufficient sleep to feel rested?
- Affect, mood and mental health: Do you have concerns about your mood, anxiety, or stress?
- Food, diet and supplements: Do you have concerns about getting enough or healthy enough food, or have any questions about supplements or vitamins?
- Exercise: Do you find ways to fit physical exercise into your life?
- Supportive social interactions: Do you have regular contact with close friends or family, and do you have enough support from people?
- Trauma avoidance: Do you wear seatbelts and helmets, and use car seats for children?
- Blood pressure: Have you had problems with high blood pressure at home or at doctor visits, or do you have any concerns about blood pressure treatment or getting a blood pressure cuff at home?
- Risks, genetic and metabolic factors: Do you have trouble controlling blood sugar or cholesterol? Is there a neurological disease that runs in your family?
- Affordability and adherence: Do you have any trouble with the cost of your medicines?
- Infection: Are you up to date on vaccines, and do you have enough information about those vaccines?
- Negative exposures: Do you smoke, drink more than one to two drinks per day, or use non-prescription drugs? Do you drink well water, or live in an area with known air or water pollution?
- Social and structural determinants of health: Do you have concerns about keeping housing, having transportation, having access to care and medical insurance, or being physically or emotionally safe from harm?
You will note that some of these are well-known (to 10almonds readers, at least!) risk factors for cognitive decline, but others are more about systemic and/or environmental considerations, things that don’t directly pertain to brain health, but can have a big impact on it anyway.
About “concerns”: in the case of those questions that ask “do you have concerns about…?”, and you’re not sure, then yes, you do indeed have concerns.
About “trouble”: as for these kinds of health-related questionnaires in general, if a question asks you “do you have trouble with…?” and your answer is something like “no, because I have a special way of dealing with that problem” then the answer for the purposes of the questionnaire is yes, you do indeed have trouble.
Note that you can “have trouble with” something that you simultaneously “have under control”—just as a person can have no trouble at all with something that they leave very much out of control.
Further explanation on each of the questions
If you’re wondering what is meant by any of these, or what counts, or why the question is even being asked, then we recommend you check out Dr. Selwa et al’s recently-published paper, then all is explained in there, in surprisingly easy-to-read fashion:
Emerging Issues In Neurology: The Neurologist’s Role in Promoting Brain Health
If you scroll past the abstract, introduction, and disclaimers, then you’ll be straight into the tables of information about the above 12 factors.
Want to be even more proactive?
Check out:
How To Reduce Your Alzheimer’s Risk
Take care!
Share This Post
-
Stimulant Users Are Caught in Fatal ‘Fourth Wave’ of Opioid Epidemic
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In Pawtucket, Rhode Island, near a storefront advertising “free” cellphones, J.R. sat in an empty back stairwell and showed a reporter how he tries to avoid overdosing when he smokes crack cocaine. KFF Health News is identifying him by his initials because he fears being arrested for using illegal drugs.
It had been several hours since his last hit, and the chatty, middle-aged man’s hands moved quickly. In one hand, he held a glass pipe. In the other, a lentil-size crumb of cocaine.
Or at least J.R. hoped it was cocaine, pure cocaine — uncontaminated by fentanyl, a potent opioid that was linked to about 75% of all overdose deaths in Rhode Island in 2022. He flicked his lighter to “test” his supply. He believed that if it had a “cigar-like sweet smell,” he said, it would mean that the cocaine was laced with fentanyl. He put the pipe to his lips and took a tentative puff. “No sweet,” he said, reassured.
But this method offers only false and dangerous reassurance. A mistake can be fatal.
It is impossible to tell whether a drug contains fentanyl by the taste or smell. “Somebody can believe that they can smell it or taste it, or see it … but that’s not a scientific test,” said Josiah “Jody” Rich, an addiction specialist and researcher who teaches at Brown University. “People are going to die today because they buy some cocaine that they don’t know has fentanyl in it.”
The first wave of the long-running and devastating opioid epidemic began in the United States with the abuse of prescription painkillers in the early 2000s. The second wave involved an increase in heroin use, starting around 2010. The third wave began when powerful synthetic opioids such as fentanyl started appearing in the supply around 2015. Now experts are observing a fourth phase of the deadly epidemic.
The mix of stimulants such as cocaine and methamphetamines with fentanyl — a synthetic opioid 50 times as powerful as heroin — is driving what experts call the opioid epidemic’s “fourth wave.” The mixture of stimulants and fentanyl presents powerful challenges to efforts to reduce overdoses because many users of stimulants don’t know they are at risk of ingesting opioids, so they don’t take overdose precautions.
The only way to know whether cocaine or other stimulants contain fentanyl is to use drug-checking tools such as fentanyl test strips — a best practice for what’s known as “harm reduction,” now embraced by federal health officials in combating drug overdose deaths. Fentanyl test strips cost as little as $2 for a two-pack online, but many front-line organizations also give them out free.
Nationwide, illicit stimulants mixed with fentanyl were the most common drugs found in fentanyl-related overdoses, according to a study published in 2023 in the scientific journal Addiction. The stimulant in the fatal mixture tends to be cocaine in the Northeast, and methamphetamine in the West and much of the Midwest and South.
“The No. 1 thing that people in the U.S. are dying from in terms of drug overdoses is the combination of fentanyl and a stimulant,’’ said Joseph Friedman, a researcher at UCLA and the study’s lead author. “Black and African Americans are disproportionately affected by this crisis to a large magnitude, especially in the Northeast.”
Friedman was also the lead author of another new study, published in the American Journal of Psychiatry, that shows the fourth wave of the opioid epidemic is driving up the mortality rate among older Black Americans (ages 55-64) and, more recently, Hispanic people. Friedman said part of the reason street fentanyl is so deadly is that there’s no way to tell how potent it is. Hospitals have safely used medical-grade fentanyl for surgical pain because the potency is strictly regulated, but “the potency fluctuates wildly in the illicit market” Friedman said.
Studies of street drugs, he said, show that in illicit drugs the potency can vary from 1% to 70% fentanyl.
“Imagine ordering a mixed drink in a bar and it contains one to 70 shots,” Friedman said, “and the only way you know is to start drinking it. … There would be a huge number of alcohol overdose deaths.”
Drug-checking technology can provide a rough estimate of fentanyl concentration, he said, but to get a precise measure requires sending drugs to a laboratory.
It’s not clear how much of the latest trend in polydrug use — in which users mix substances, such as cocaine and fentanyl, for example — is accidental versus intentional. It can vary for individual users: a recent study from Millennium Health found that most people who use fentanyl do so at times intentionally and other times unintentionally.
People often use stimulants to power through the rapid withdrawal from fentanyl, Friedman said. And the high-risk practice of using cocaine or meth with heroin, known as “speedballing,” has been around for decades. Other factors include manufacturers’ adding the cheap synthetic opioid to a stimulant to stretch their supply, or dealers mixing up bags.
Researchers say many people still think they are using unadulterated cocaine or crack — a misconception that can be deadly. “Folks who are using stimulants, and not intentionally using opioids, are unprepared to respond to an opioid overdose,” said Brown University epidemiologist Jaclyn White Hughto, “because they don’t perceive themselves to be at risk.” Hughto is a principal investigator in a new, unpublished study called “Preventing Overdoses Involving Stimulants.”
Hughto and the team surveyed more than 260 people in Rhode Island and Massachusetts who use drugs, including some who manufacture and distribute stimulants such as cocaine. More than 60% of the people they interviewed in Rhode Island had bought or used stimulants that they later found out had fentanyl in them. And many of the people interviewed in the study also use drugs alone. That means that if they do overdose, they may not be found until it’s too late.
In 2022, Rhode Island had the fourth-highest rate of overdose deaths involving cocaine in 2022, after Washington, D.C., Delaware, and Vermont, according to the Centers for Disease Control and Prevention.
The fourth wave is also hitting stimulant users who choose pills over what they perceive as more dangerous drugs such as cocaine in an effort to avoid fentanyl. That’s what happened to Jennifer Dubois’ son Cliffton.
Dubois was a single mother raising two Black sons. The older son, Cliffton, had been struggling with addiction since he was 14, she said. Cliffton also had been diagnosed with attention-deficit/hyperactivity disorder and a mood disorder.
In March 2020, Cliffton had checked into a rehab program as the pandemic ramped up, Dubois said. Because of the lockdown at rehab, Cliffton was upset about not being able to visit with his mother. “He said, ‘If I can’t see my mom, I can’t do treatment,’” Dubois recalled. “And I begged him” to stay in treatment.
But soon after, Cliffton left the rehab program. He showed up at her door. “And I just cried,” she said.
Dubois’ younger son was living at home. She didn’t want Cliffton doing drugs around his younger brother. So she gave Cliffton an ultimatum: “If you want to stay home, you have to stay drug-free.”
Cliffton went to stay with family friends, first in Atlanta and later in Woonsocket, an old mill city that has Rhode Island’s highest rate of drug overdose deaths.
In August 2020, Cliffton overdosed but was revived. Cliffton later confided that he’d been snorting cocaine in a car with a friend, Dubois said. Hospital records show he tested positive for fentanyl.
“He was really scared,” Dubois said. After the overdose, he tried to “leave the cocaine and the hard drugs alone,” she said. “But he was taking pills.” Eight months later, on April 17, 2021, Cliffton was found unresponsive in the bedroom of a family member’s home.
The night before, Cliffton had bought counterfeit Adderall, according to the police report. What he didn’t know was that the Adderall pill was laced with fentanyl. “He thought by staying away from the street drugs and just taking pills, he was doing better,” Dubois said.
A fentanyl test strip could have saved his life.
This article is from a partnership that includes The Public’s Radio, NPR, and KFF Health News.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
Dial Down Your Pain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is Dr. Christiane Wolf. Is than an MD or a PhD, you ask? The answer is: yes (it is both; the latter being in psychosomatic medicine).
She also teaches Mindfulness-Based Stress Reduction, which as you may recall is pretty much the most well-evidenced* form of meditation there is, in terms of benefits:
No-Frills, Evidence-Based Mindfulness
*which is not to claim it is necessarily the best (although it also could be); rather, this means that it is the form of meditation that’s accumulated the most scientific backing in total. If another equal or better form of meditation enjoyed less scientific scrutiny, then there could an alternative out there languishing with only two and a half scientific papers to its name. However, we at 10almonds are not research scientists, and thus can only comment on the body of evidence that has been published.
In any case, today is going to be about pain.
What does she want us to know?
Your mind does matter
It’s easy to think that anything you can do with your mind is going to be quite small comfort when your nerves feel like they’re on fire.
However, Dr. Wolf makes the case for pain consisting of three components:
- the physical sensation(s)
- the emotions we have about those
- the meaning we give to such (or “the story” that we use to describe it)
To clarify, let’s give an example:
- the physical sensations of burning, searing, and occasionally stabbing pains in the lower back
- the emotions of anguish, anger, despair, self-pity
- the story of “this pain has ruined my life, is making it unbearable, will almost certainly continue, and may get worse”
We are not going to tell you to throw any of those out of the window for now (and, would that you could throw the first line out, of course).
The first thing Dr. Wolf wants us to do to make this more manageable is to break it down.
Because presently, all three of those things are lumped together in a single box labelled “pain”.
If each of those items is at a “10” on the scale of pain, then this is 10×10×10=1000.
If our pain is at 1000/10, that’s a lot. We want to leave the pain in the box, not look at it, and try to distract ourselves. That is one possible strategy, by the way, and it’s not always bad when it comes to giving oneself a short-term reprieve. We balanced it against meditation, here:
Managing Chronic Pain (Realistically)
However, back to the box analogy, if we open that box and take out each of those items to examine them, then even without changing anything, even with them all still at 10, they can each be managed for what they are individually, so it’s now 10+10+10=30.
If our pain is at 30/10, that’s still a lot, but it’s a lot more manageable than 1000/10.
On rating pain, by the way, see:
Get The Right Help For Your Pain
Dealing with the separate parts
It would be nice, of course, for each of those separate parts to not be at 10.
With regard to the physical side of pain, this is not Dr. Wolf’s specialty, but we have some good resources here at 10almonds:
- The 7 Approaches To Pain Management
- 10 Tips To Reduce Morning Pain & Stiffness With Arthritis
- Science-Based Alternative Pain Relief: When Painkillers Aren’t Helping, These Things Might
When it comes to emotions associated with pain, Dr. Wolf (who incidentally is a Buddhist and also a teacher of same, and runs meditation retreats for such), recommends (of course) mindfulness, and what in Dialectical Behavior Therapy (DBT) is called “radical acceptance” (in Buddhism, it may be referred to as being at one with things). We’ve written about this here:
“Hello, Emotions”: Radical Acceptance In CBT & DBT
Once again, the aim here is still not to throw the (often perfectly valid) emotions out of the window (unless you want to), but rather, to neutrally note and acknowledge the emotions as they arrive, á la “Hello, despair. Depression, my old foe, we meet again. Hello again, resentment.” …and so on.
The reason this helps is because emotions, much like the physical sensations of pain, are first and foremost messengers, and sometimes (as in the case of chronic pain) they get broken and keep delivering the message beyond necessity. Acknowledging the message helps your brain (and all that is attached to it) realize “ok, this message has been delivered now; we can chill about it a little”.
Having done that, if you can reasonably tweak any of the emotions (for example, perhaps that self-pity we mentioned could be turned into self-compassion, which is more useful), that’s great. If not, at least you know what’s on the battlefield now.
When we examine the story of our pain, lastly, Dr. Wolf invites us to look at how one of the biggest drivers of distress under pain is the uncertainty of how long the pain will last, whether it will get worse, whether what we are doing will make it worse, and so forth. See for example:
How long does back pain last? And how can learning about pain increase the chance of recovery?
And of course, many things we do specifically in response to pain can indeed make our pain worse, and spread:
Dr. Wolf’s perspective says:
- Life involves pain
- Pain invariably has a cause
- What has a cause, can have an end
- We just need to go through that process
This may seem like small comfort when we are in the middle of the pain, but if we’ve broken it down into parts with Dr. Wolf’s “box method”, and dealt with the first two parts (the sensations and the emotions) as well as reasonably possible, then we can tackle the third one (the story) a little more easily than we could if we were trying to come at it with no preparation.
What used to be:
“This pain has ruined my life, is making it unbearable, will almost certainly continue, and may get worse”
…can now become:
“This pain is a big challenge, but since I’m here for it whether I want to be or not, I will suffer as I must, while calmly looking for ways to reduce that suffering as I go.”
In short: you cannot “think healing thoughts” and expect your pain to go away. But you can do a lot more than you might (if you left it unexamined) expect.
Want to know more from Dr. Wolf?
We reviewed a book of hers recently, which you might enjoy:
Outsmart Your Pain – by Dr. Christiane Wolf
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Broccoli vs Red Cabbage – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing broccoli to red cabbage, we picked the broccoli.
Why?
Both are certainly great! Which is usual for any Brassica oleracea cultivar (as both of these vegetables are). But there is a clear winner:
In terms of macros, broccoli has more fiber and protein, while red cabbage has more carbs. Now, nobody is getting metabolic disease from eating cabbage, but by the numbers, this is a simple win for broccoli, especially on account of the fiber.
In the category of vitamins, broccoli has more of vitamins B1, B2, B3, B5, C, E, K, and choline, while red cabbage has more of vitamins A and B6. Another win for broccoli.
When it comes to minerals, it’s a similar story: broccoli has more copper, magnesium, phosphorus, potassium, selenium, and zinc, while red cabbage has more iron and manganese. They’re equal in calcium, by the way. Broccoli wins again.
Looking at polyphenols, both cultivars have plenty, but broccoli has more in total, as well as more variety, so yet another win for broccoli here.
Now, standing next to broccoli has made red cabbage look bad, but we want to assure you that red cabbage is itself a nutritional powerhouse—broccoli is just even more so.
So of course, by all means do enjoy either or both; diversity is good!
Want to learn more?
You might like:
21 Most Beneficial Polyphenols & What Foods Have Them
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
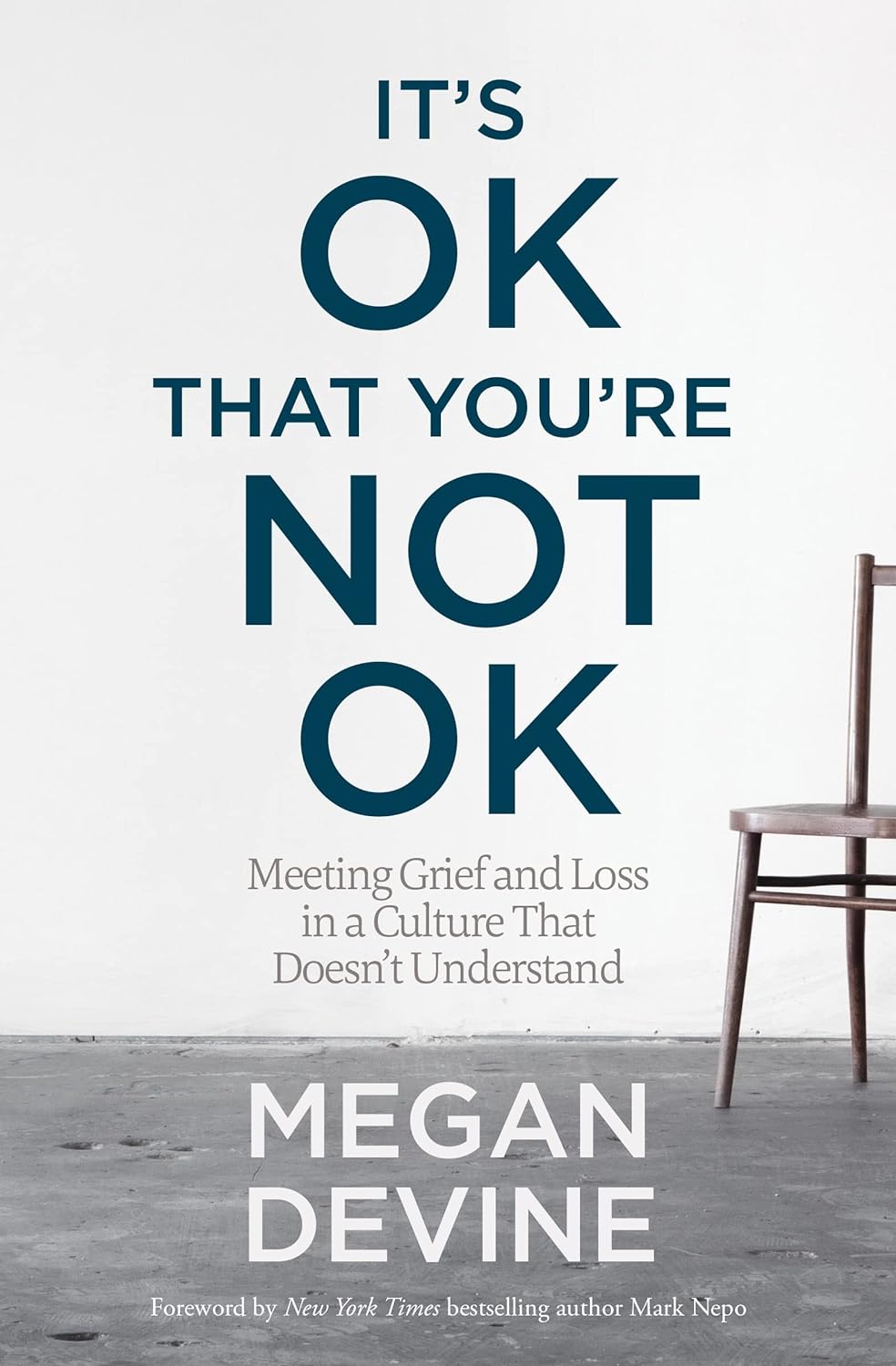
It’s OK That You’re Not OK – by Megan Devine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Firstly, be aware: this is not a cheerful book. If you’re looking for something to life your mood after a loss, it will not be this.
What, then, will you find? A reminder that grief is also the final translation of love, and not necessarily something to be put aside as quickly as possible—or even ever, if we don’t want to.
Too often, society (and even therapists) will correctly note that no two instances of grief are the same (after all, no two people are, so definitely no two relationships are, so how could two instances of grief be?), but will still expect that if most people can move on quickly from most losses, that you should too, and that if you don’t then there is something pathological at hand that needs fixing.
Part one of the book covers this (and more) in a lot of detail; critics have called it a diatribe against the current status quo in the field of grief.
Part two of the book is about “what to do with your grief”, and addresses the reality of grief, how (and why) to stay alive when not doing so feels like a compelling option, dealing with grief’s physical side effects, and calming your mind in ways that actually work (without trying to sweep your grief under a rug).
Parts three and four are more about community—how to navigate the likely unhelpful efforts a lot of people may make in the early days, and when it comes to those people who can and will actually be a support, how to help them to help you.
In the category of criticism, she also plugs her own (paid, subscription-based) online community, which feels a little mercenary, especially as while community definitely can indeed help, the prospect of being promptly exiled from it if you stop paying, doesn’t.
Bottom line: if you have experienced grief and felt like moving on was the right thing to do, then this book isn’t the one for you. If, on the other hand, your grief feels more like something you will carry just as you carry the love you feel for them, then you’ll find a lot about that here.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: