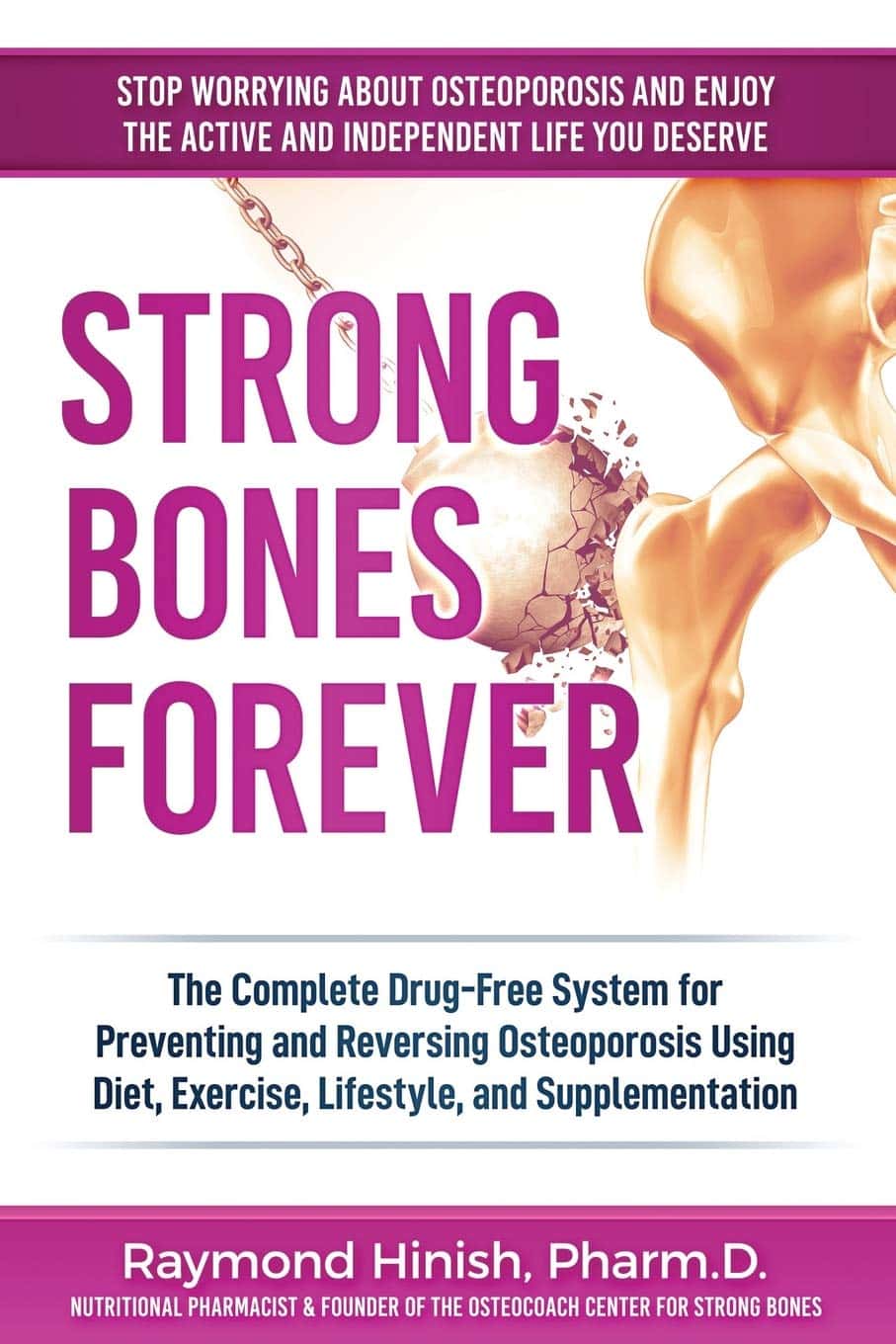
Strong Bones Forever − by Dr. Raymond Hinish
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This doctor of pharmacy would like for fewer people to take (or need to take) osteoporosis medications. Indeed, as the subtitle suggests, the focus here is on drug-free solutions.
And not just because “natural is better” as an argument without evidence, rather, he talks about the limitations and drawbacks of osteoporosis medications (which we wrote about previously, but he has more room to go into more detail), whereupon some osteoporosis meds may do more harm than good.
His method boasts improvements in bone density by 11% or more in two years, and covers such topics as:
- which calcium (and why no, dairy is not what you want; it contains things that inhibit calcium absorption, so the calcium will be stuck in your arteries instead of your bones)
- which minerals are more important than calcium, and why
- common mistakes that many people make that sabotage their bone density
It’s about more than just diet though; he does also talk about hormones, and not just other lifestyle factors, but also many “industry secrets” that aren’t really secrets per se, it’s just, people outside of the industry don’t usually know them—pertaining to things like how to get the most out of bone density tests (i.e. how to get better accuracy), how to meaningfully assess fracture risk, and, if choosing to take osteoporosis meds, how to minimize the risks and maximize the benefits.
The style is very direct and informational, very easy to read, remarkably jargon-free, and our only criticism is that there is no bibliography.
Bottom line: if you’d like to improve your bone density, this book can certainly help with that.
Click here to check out Strong Bones Forever, and have strong bones forever!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Peas vs Green Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing peas to green beans, we picked the peas.
Why?
Looking at macros first, peas have nearly 6x the protein, nearly 2x the fiber, and nearly 2x the carbs, making them the “more food per food” choice.
In terms of vitamins, peas have more of vitamins A, B1, B2, B3, B5, B6, B7, B9, C, and choline, while green beans have more of vitamins E and K. An easy win for peas.
In the category of minerals, peas have more copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while green beans have more calcium. Another overwhelming win for peas.
In short, enjoy both (diversity is good), but there’s a clear winner here and it’s peas.
Want to learn more?
You might like to read:
Peas vs Broad Beans – Which is Healthier?
Take care!
Share This Post
-
We don’t all need regular skin cancer screening – but you can know your risk and check yourself
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Australia has one of the highest skin cancer rates globally, with nearly 19,000 Australians diagnosed with invasive melanoma – the most lethal type of skin cancer – each year.
While advanced melanoma can be fatal, it is highly treatable when detected early.
But Australian clinical practice guidelines and health authorities do not recommend screening for melanoma in the general population.
Given our reputation as the skin cancer capital of the world, why isn’t there a national screening program? Australia currently screens for breast, cervical and bowel cancer and will begin lung cancer screening in 2025.
It turns out the question of whether to screen everyone for melanoma and other skin cancers is complex. Here’s why.
Pixel-Shot/Shutterstock The current approach
On top of the 19,000 invasive melanoma diagnoses each year, around 28,000 people are diagnosed with in-situ melanoma.
In-situ melanoma refers to a very early stage melanoma where the cancerous cells are confined to the outer layer of the skin (the epidermis).
Instead of a blanket screening program, Australia promotes skin protection, skin awareness and regular skin checks (at least annually) for those at high risk.
About one in three Australian adults have had a clinical skin check within the past year.
Those with fairer skin or a family history may be at greater risk of skin cancer. Halfpoint/Shutterstock Why not just do skin checks for everyone?
The goal of screening is to find disease early, before symptoms appear, which helps save lives and reduce morbidity.
But there are a couple of reasons a national screening program is not yet in place.
We need to ask:
1. Does it save lives?
Many researchers would argue this is the goal of universal screening. But while universal skin cancer screening would likely lead to more melanoma diagnoses, this might not necessarily save lives. It could result in indolent (slow-growing) cancers being diagnosed that might have never caused harm. This is known as “overdiagnosis”.
Screening will pick up some cancers people could have safely lived with, if they didn’t know about them. The difficulty is in recognising which cancers are slow-growing and can be safely left alone.
Receiving a diagnosis causes stress and is more likely to lead to additional medical procedures (such as surgeries), which carry their own risks.
2. Is it value for money?
Implementing a nationwide screening program involves significant investment and resources. Its value to the health system would need to be calculated, to ensure this is the best use of resources.
Narrower targets for better results
Instead of screening everyone, targeting high-risk groups has shown better results. This focuses efforts where they’re needed most. Risk factors for skin cancer include fair skin, red hair, a history of sunburns, many moles and/or a family history.
Research has shown the public would be mostly accepting of a risk-tailored approach to screening for melanoma.
There are moves underway to establish a national targeted skin cancer screening program in Australia, with the government recently pledging $10.3 million to help tackle “the most common cancer in our sunburnt country, skin cancer” by focusing on those at greater risk.
Currently, Australian clinical practice guidelines recommend doctors properly evaluate all patients for their future risk of melanoma.
Looking with new technological eyes
Technological advances are improving the accuracy of skin cancer diagnosis and risk assessment.
For example, researchers are investigating 3D total body skin imaging to monitor changes to spots and moles over time.
Artificial intelligence (AI) algorithms can analyse images of skin lesions, and support doctors’ decision making.
Genetic testing can now identify risk markers for more personalised screening.
And telehealth has made remote consultations possible, increasing access to specialists, particularly in rural areas.
Check yourself – 4 things to look for
Skin cancer can affect all skin types, so it’s a good idea to become familiar with your own skin. The Skin Cancer College Australasia has introduced a guide called SCAN your skin, which tells people to look for skin spots or areas that are:
1. sore (scaly, itchy, bleeding, tender) and don’t heal within six weeks
2. changing in size, shape, colour or texture
3. abnormal for you and look different or feel different, or stand out when compared to your other spots and moles
4. new and have appeared on your skin recently. Any new moles or spots should be checked, especially if you are over 40.
If something seems different, make an appointment with your doctor.
You can self-assess your melanoma risk online via the Melanoma Institute Australia or QIMR Berghofer Medical Research Institute.
H. Peter Soyer, Professor of Dermatology, The University of Queensland; Anne Cust, Professor of Cancer Epidemiology, The Daffodil Centre and Melanoma Institute Australia, University of Sydney; Caitlin Horsham, Research Manager, The University of Queensland, and Monika Janda, Professor in Behavioural Science, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Do We Simply Not Care About Old People?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The covid-19 pandemic would be a wake-up call for America, advocates for the elderly predicted: incontrovertible proof that the nation wasn’t doing enough to care for vulnerable older adults.
The death toll was shocking, as were reports of chaos in nursing homes and seniors suffering from isolation, depression, untreated illness, and neglect. Around 900,000 older adults have died of covid-19 to date, accounting for 3 of every 4 Americans who have perished in the pandemic.
But decisive actions that advocates had hoped for haven’t materialized. Today, most people — and government officials — appear to accept covid as a part of ordinary life. Many seniors at high risk aren’t getting antiviral therapies for covid, and most older adults in nursing homes aren’t getting updated vaccines. Efforts to strengthen care quality in nursing homes and assisted living centers have stalled amid debate over costs and the availability of staff. And only a small percentage of people are masking or taking other precautions in public despite a new wave of covid, flu, and respiratory syncytial virus infections hospitalizing and killing seniors.
In the last week of 2023 and the first two weeks of 2024 alone, 4,810 people 65 and older lost their lives to covid — a group that would fill more than 10 large airliners — according to data provided by the CDC. But the alarm that would attend plane crashes is notably absent. (During the same period, the flu killed an additional 1,201 seniors, and RSV killed 126.)
“It boggles my mind that there isn’t more outrage,” said Alice Bonner, 66, senior adviser for aging at the Institute for Healthcare Improvement. “I’m at the point where I want to say, ‘What the heck? Why aren’t people responding and doing more for older adults?’”
It’s a good question. Do we simply not care?
I put this big-picture question, which rarely gets asked amid debates over budgets and policies, to health care professionals, researchers, and policymakers who are older themselves and have spent many years working in the aging field. Here are some of their responses.
The pandemic made things worse. Prejudice against older adults is nothing new, but “it feels more intense, more hostile” now than previously, said Karl Pillemer, 69, a professor of psychology and gerontology at Cornell University.
“I think the pandemic helped reinforce images of older people as sick, frail, and isolated — as people who aren’t like the rest of us,” he said. “And human nature being what it is, we tend to like people who are similar to us and be less well disposed to ‘the others.’”
“A lot of us felt isolated and threatened during the pandemic. It made us sit there and think, ‘What I really care about is protecting myself, my wife, my brother, my kids, and screw everybody else,’” said W. Andrew Achenbaum, 76, the author of nine books on aging and a professor emeritus at Texas Medical Center in Houston.
In an environment of “us against them,” where everybody wants to blame somebody, Achenbaum continued, “who’s expendable? Older people who aren’t seen as productive, who consume resources believed to be in short supply. It’s really hard to give old people their due when you’re terrified about your own existence.”
Although covid continues to circulate, disproportionately affecting older adults, “people now think the crisis is over, and we have a deep desire to return to normal,” said Edwin Walker, 67, who leads the Administration on Aging at the Department of Health and Human Services. He spoke as an individual, not a government representative.
The upshot is “we didn’t learn the lessons we should have,” and the ageism that surfaced during the pandemic hasn’t abated, he observed.
Ageism is pervasive. “Everyone loves their own parents. But as a society, we don’t value older adults or the people who care for them,” said Robert Kramer, 74, co-founder and strategic adviser at the National Investment Center for Seniors Housing & Care.
Kramer thinks boomers are reaping what they have sown. “We have chased youth and glorified youth. When you spend billions of dollars trying to stay young, look young, act young, you build in an automatic fear and prejudice of the opposite.”
Combine the fear of diminishment, decline, and death that can accompany growing older with the trauma and fear that arose during the pandemic, and “I think covid has pushed us back in whatever progress we were making in addressing the needs of our rapidly aging society. It has further stigmatized aging,” said John Rowe, 79, professor of health policy and aging at Columbia University’s Mailman School of Public Health.
“The message to older adults is: ‘Your time has passed, give up your seat at the table, stop consuming resources, fall in line,’” said Anne Montgomery, 65, a health policy expert at the National Committee to Preserve Social Security and Medicare. She believes, however, that baby boomers can “rewrite and flip that script if we want to and if we work to change systems that embody the values of a deeply ageist society.”
Integration, not separation, is needed. The best way to overcome stigma is “to get to know the people you are stigmatizing,” said G. Allen Power, 70, a geriatrician and the chair in aging and dementia innovation at the Schlegel-University of Waterloo Research Institute for Aging in Canada. “But we separate ourselves from older people so we don’t have to think about our own aging and our own mortality.”
The solution: “We have to find ways to better integrate older adults in the community as opposed to moving them to campuses where they are apart from the rest of us,” Power said. “We need to stop seeing older people only through the lens of what services they might need and think instead of all they have to offer society.”
That point is a core precept of the National Academy of Medicine’s 2022 report Global Roadmap for Healthy Longevity. Older people are a “natural resource” who “make substantial contributions to their families and communities,” the report’s authors write in introducing their findings.
Those contributions include financial support to families, caregiving assistance, volunteering, and ongoing participation in the workforce, among other things.
“When older people thrive, all people thrive,” the report concludes.
Future generations will get their turn. That’s a message Kramer conveys in classes he teaches at the University of Southern California, Cornell, and other institutions. “You have far more at stake in changing the way we approach aging than I do,” he tells his students. “You are far more likely, statistically, to live past 100 than I am. If you don’t change society’s attitudes about aging, you will be condemned to lead the last third of your life in social, economic, and cultural irrelevance.”
As for himself and the baby boom generation, Kramer thinks it’s “too late” to effect the meaningful changes he hopes the future will bring.
“I suspect things for people in my generation could get a lot worse in the years ahead,” Pillemer said. “People are greatly underestimating what the cost of caring for the older population is going to be over the next 10 to 20 years, and I think that’s going to cause increased conflict.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
Related Posts
-
Kale vs Watercress – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing kale to watercress, we picked the kale.
Why?
It was very close! If ever we’ve been tempted to call something a tie, this has been the closest so far.
Their macros are close; watercress has a tiny amount more protein and slightly lower carbs, but these numbers are tiny, so it’s not really a factor. Nevertheless, on macros alone we’d call this a slight nominal win for watercress.
In terms of vitamins, they’re even. Watercress has higher vitamin E and choline (sometimes considered a vitamin), as well as being higher in some B vitamins. Kale has higher vitamins A and K, as well as being higher in some other B vitamins.
In the category of minerals, watercress has higher calcium, magnesium, phosphorus, and potassium, while kale has higher copper, iron, manganese, and zinc. The margins are slightly wider for kale’s more plentiful minerals though, so we’ll call this section a marginal win for kale.
When it comes to polyphenols, kale takes and maintains the lead here, with around 2x the quercetin and 27x the kaempferol. Watercress does have some lignans that kale doesn’t, but ultimately, kale’s strong flavonoid content keeps it in the lead.
So of course: enjoy both if both are available! But if we must pick one, it’s kale.
Want to learn more?
You might like to read:
- Fight Inflammation & Protect Your Brain, With Quercetin
- Spinach vs Kale – Which is Healthier?
- Thai-Style Kale Chips (recipe)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Apple vs Peach – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing apples to peaches, we picked the peaches.
Why?
Both have their merits, but apples can’t compete with peaches’ micronutrient profile!
In terms of macros, apples have more carbs and fiber, for a comparable glycemic index, so we give apples a marginal win in the macros category to start with.
In the category of vitamins, apples have more vitamin B6, while peaches have more of vitamins A, B1, B2, B3, B5, B7, B9, C, E, K, and choline—an easy win for peaches.
When it comes to minerals, apples are not higher in any minerals, while peaches have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. Another clear win for peaches!
Looking at polyphenols, peaches have a higher total amount (in mg/100g) of polyphenols, as well as more variety thereof. One more win for peaches.
Adding up the sections makes for a clear win for peaches, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
Top 8 Fruits That Prevent & Kill Cancer ← peaches are number 2 on the list! They contain phytochemicals that induce cell death in cancer cells while sparing healthy ones 😎
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
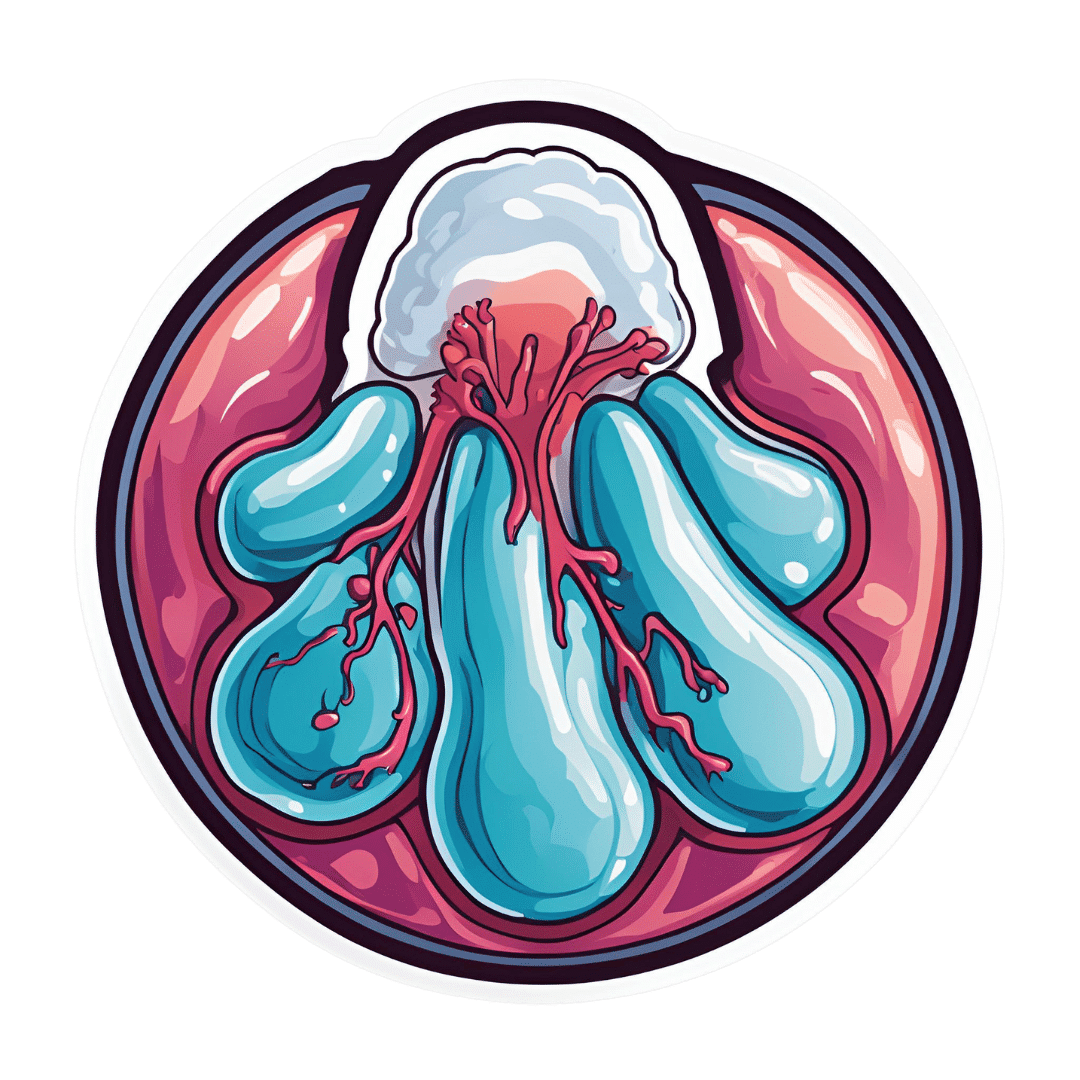
8 Signs Of Hypothyroidism Beyond Tiredness & Weight Gain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to hypothyroidism, most people know to look out for tiredness and weight gain, and possibly menstrual disturbances in those who menstruate. But those symptoms could be caused by very many things, so what more specific signs and symptoms of hypothyroidism should we look out for?
Dr. James O’Donovan shows us in this short video:
The lesser-known signs
Dr. O’Donovan discusses:
- Asteatotic eczema (also called: eczema craquelé): dry, cracked skin with a “crazy paving” appearance, leading to fissures. It’s common on the lower legs, back, torso, and arms, especially in older patients and especially in winter.
- Cold peripheries with pale, dry, coarse skin: cold hands and feet, along with dryness due to decreased sweating; these invariably come together, though the exact link is unclear.
- Yellowish hue to the skin (carotenoderma): yellow-orange discoloration from elevated beta-carotene levels. This can easily be mistaken for jaundice and also occurs in diabetes, liver, and kidney diseases.
- Thin, brittle hair: the hair on one’s head may become dry, coarse, and fall out in handfuls.
- Loss of hair on the outer third of eyebrows: thinning or disappearance of hair in this very specific area.
- Slow-growing, rigid, brittle nails: slowed nail growth due to decreased cell turnover rate. Ridges may form as keratin cells accumulate.
- Myxedema: puffy face, eyelids, legs, and feet caused by tissue swelling from cutaneous deposition.
- Delayed wound healing: is what it sounds like; a slower healing process.
10almonds note: this video, like much of medical literature as well, does focus on what things are like for white people. Black people with hypothyroidism are more likely to see a lightening of hair pigmentation, and, in contrast, hyperpigmentation of the skin, usually in patches. We couldn’t find data for other ethnicities or skintones, but it does seem that most of the signs and symptoms (unrelated to pigmentation) should be the same for most people.
Meanwhile, for more on the above 8 signs, with visuals, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
The Three Rs To Boost Thyroid-Related Energy Levels
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: