Montana Eyes $30M Revamp of Mental Health, Developmental Disability Facilities
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
HELENA, Mont. — As part of a proposed revamping of the state’s behavioral health system, Republican Gov. Greg Gianforte’s administration is looking into moving a facility for people with developmental disabilities, beefing up renovations at the Montana State Hospital, and creating a Helena unit of that psychiatric hospital.
The changes, backers say, would fill gaps in services and help people better prepare for life outside of the locked, secure setting of the two state facilities before they reenter their own communities.
“I think part of the theme is responsibly moving people in and out of the state facilities so that we create capacity and have people in the appropriate places,” state Sen. Dave Fern (D-Whitefish) said of the proposed capital projects during a recent interview.
Fern served on the Behavioral Health System for Future Generations Commission, a panel created by a 2023 law to suggest how to spend $300 million to revamp the system. The law set aside the $300 million for improving state services for people with mental illness, substance abuse disorders, and developmental disabilities.
Gianforte’s proposed budget for the next two years would spend about $100 million of that fund on 10 other recommendations from the commission. The capital projects are separate ideas for using up to $32.5 million of the $75 million earmarked within the $300 million pool of funds for building new infrastructure or remodeling existing buildings.
The state Department of Public Health and Human Services and consultants for the behavioral health commission presented commission members with areas for capital investments in October. In December, the commission authorized state health department director Charlie Brereton to recommend the following projects to Gianforte:
- Move the 12-bed Intensive Behavior Center for people with developmental disabilities out of Boulder, possibly to either Helena or Butte, at an estimated cost of up to $13.3 million.
- Establish a “step-down” facility of about 16 beds, possibly on the campus of Shodair Children’s Hospital in Helena, to serve adults who have been committed to the Montana State Hospital but no longer need the hospital’s intensive psychiatric services.
- Invest $19.2 million to upgrade the Montana State Hospital’s infrastructure and buildings at Warm Springs, on top of nearly $16 million appropriated in 2023 for renovations already underway there in an effort to regain federal certification of the facility.
The state Architecture & Engineering Division is reviewing the health department’s cost estimates and developing a timeline for the projects so the information can be sent to the governor. Gianforte ultimately must approve the projects.
Health department officials have said they plan to take the proposals to legislative committees as needed. “With Commission recommendation and approval from the governor, the Department believes that it has the authority to proceed with capital project expenditures but must secure additional authority from the Legislature to fund operations into future biennia,” said department spokesperson Jon Ebelt.
The department outlined its facility plans to the legislature’s health and human services budget subcommittee on Jan. 22 as part of a larger presentation on the commission’s work and the 10 noncapital proposals in the governor’s budget. Time limits prevented in-depth discussion and public comment on the facility-related ideas.
One change the commission didn’t consider: moving the Montana State Hospital to a more populated area from its rural and relatively remote location near Anaconda, in southwestern Montana, in an attempt to alleviate staffing shortages.
“The administration is committed to continuing to invest in MSH as it exists today,” Brereton told the commission in October, referring to the Montana State Hospital.
The hospital provides treatment to people with mental illness who have been committed to the state’s custody through a civil or criminal proceeding. It’s been beset by problems, including the loss of federal Medicaid and Medicare funding due to decertification by the federal government in April 2022, staffing issues that have led to high use of expensive traveling health care providers, and turnover in leadership.
State Sen. Chris Pope (D-Bozeman) was vice chair of a separate committee that met between the 2023 and 2025 legislative sessions and monitored progress toward a 2023 legislative mandate to transition patients with dementia out of the state hospital. He agreed in a recent interview that improving — not moving — MSH is a top priority for the system right now.
“Right now, we have an institution that is failing and needs to be brought back into the modern age, where it is located right now,” he said after ticking off a list of challenges facing the hospital.
State Sen. John Esp (R-Big Timber) also noted at the October commission meeting that moving the hospital was likely to run into resistance in any community considered for a new facility.
Fern, the Whitefish senator, questioned in October whether similar concerns might exist for moving the Intensive Behavior Center out of Boulder. For more than 130 years, the town 30 miles south of Helena has been home, in one form or another, to a state facility for people with developmental disabilities. But Brereton said he believes relocation could succeed with community and stakeholder involvement.
The 12-bed center in Boulder serves people who have been committed by a court because their behaviors pose an immediate risk of serious harm to themselves or others. It’s the last residential building for people with developmental disabilities on the campus of the former Montana Developmental Center, which the legislature voted in 2015 to close.
Drew Smith, a consultant with the firm Alvarez & Marsal, told the commission in October that moving the facility from the town of 1,300 to a bigger city such as Helena or Butte would provide access to a larger labor pool, possibly allow a more homelike setting for residents, and open more opportunities for residents to interact with the community and develop skills for returning to their own communities.
Ideally, Brereton said, the center would be colocated with a new facility included in the governor’s proposed budget, for crisis stabilization services to people with developmental disabilities who are experiencing significant behavioral health issues.
Meanwhile, the proposed subacute facility with up to 16 beds for state hospital patients would provide a still secure but less structured setting for people who no longer need intensive treatment at Warm Springs but aren’t yet ready to be discharged from the hospital’s care. Brereton told the commission in October the facility would essentially serve as a less restrictive “extension” of the state hospital. He also said the agency would like to contract with a company to staff the subacute facility.
Health department officials don’t expect the new facility to involve any construction costs. Brereton has said the agency believes an existing building on the Shodair campus would be a good spot for it.
The state began leasing the building Nov. 1 for use by about 20 state hospital patients displaced by the current remodeling at Warm Springs — a different purpose than the proposed subacute facility.
Shodair CEO Craig Aasved said Shodair hasn’t committed to having the state permanently use the building as the step-down facility envisioned by the agency and the commission.
But Brereton said the option is attractive to the health department now that the building has been set up and licensed to serve adults.
“It seems like a natural place to start,” he told the commission in December, “and we don’t mind that it’s in our backyard here in Helena.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
‘Emergency’ or Not, Covid Is Still Killing People. Here’s What Doctors Advise to Stay Safe.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
With around 20,000 people dying of covid in the United States since the start of October, and tens of thousands more abroad, the covid pandemic clearly isn’t over. However, the crisis response is, since the World Health Organization and the Biden administration ended their declared health emergencies last year.
Let’s not confuse the terms “pandemic” and “emergency.” As Abraar Karan, an infectious disease physician and researcher at Stanford University, said, “The pandemic is over until you are scrunched in bed, feeling terrible.”
Pandemics are defined by neither time nor severity, but rather by large numbers of ongoing infections worldwide. Emergencies are acute and declared to trigger an urgent response. Ending the official emergency shifted the responsibility for curbing covid from leaders to the public. In the United States, it meant, for example, that the government largely stopped covering the cost of covid tests and vaccines.
But the virus is still infecting people; indeed, it is surging right now.
With changes in the nature of the pandemic and the response, KFF Health News spoke with doctors and researchers about how to best handle covid, influenza, and other respiratory ailments spreading this season.
A holiday wave of sickness has ensued as expected. Covid infections have escalated nationwide in the past few weeks, with analyses of virus traces in wastewater suggesting infection rates as high as last year’s. More than 73,000 people died of covid in the U.S. in 2023, meaning the virus remains deadlier than car accidents and influenza. Still, compared with last year’s seasonal surge, this winter’s wave of covid hospitalizations has been lower and death rates less than half.
“We’re seeing outbreaks in homeless shelters and in nursing homes, but hospitals aren’t overwhelmed like they have been in the past,” said Salvador Sandoval, a doctor and health officer at the Merced County public health department in California. He attributes that welcome fact to vaccination, covid treatments like Paxlovid, and a degree of immunity from prior infections.
While a new coronavirus variant, JN.1, has spread around the world, the current vaccines and covid tests remain effective.
Other seasonal illnesses are surging, too, but rates are consistent with those of previous years. Between 9,400 and 28,000 people died from influenza from Oct. 1 to Jan. 6, estimates the Centers for Disease Control and Prevention, and millions felt so ill from the flu that they sought medical care. Cases of pneumonia — a serious condition marked by inflamed lungs that can be triggered by the flu, covid, or other infections — also predictably rose as winter set in. Researchers are now less concerned about flare-ups of pneumonia in China, Denmark, and France in November and December, because they fit cyclical patterns of the pneumonia-causing bacteria Mycoplasma pneumoniae rather than outbreaks of a dangerous new bug.
Public health researchers recommend following the CDC guidance on getting the latest covid and influenza vaccines to ward off hospitalization and death from the diseases and reduce chances of getting sick. A recent review of studies that included 614,000 people found that those who received two covid vaccines were also less likely to develop long covid; often involving fatigue, cognitive dysfunction, and joint pain, the condition is marked by the development or continuation of symptoms a few months after an infection and has been debilitating for millions of people. Another analysis found that people who had three doses of covid vaccines were much less likely to have long covid than those who were unvaccinated. (A caveat, however, is that those with three doses might have taken additional measures to avoid infections than those who chose to go without.)
It’s not too late for an influenza vaccine, either, said Helen Chu, a doctor and epidemiologist at the University of Washington in Seattle. Influenza continues to rise into the new year, especially in Southern states and California. Last season’s shot appeared to reduce adults’ risk of visits to the emergency room and urgent care by almost half and hospitalization by more than a third. Meanwhile, another seasonal illness with a fresh set of vaccines released last year, respiratory syncytial virus, appears to be waning this month.
Another powerful way to prevent covid, influenza, common colds, and other airborne infections is by wearing an N95 mask. Many researchers say they’ve returned to socializing without one but opt for the masks in crowded, indoor places when wearing one would not be particularly burdensome. Karan, for example, wears his favorite N95 masks on airplanes. And don’t forget good, old-fashioned hand-washing, which helps prevent infections as well.
If you do all that and still feel sick? Researchers say they reach for rapid covid tests. While they’ve never been perfect, they’re often quite helpful in guiding a person’s next steps.
When President Joe Biden declared the end of the public health emergency last year, many federally funded testing sites that sent samples to laboratories shut their doors. As a result, people now mainly turn to home covid tests that signal an infection within 15 minutes and cost around $6 to $8 each at many pharmacies. The trick is to use these tests correctly by taking more than one when there’s reason for concern. They miss early infections more often than tests processed in a lab, because higher levels of the coronavirus are required for detection — and the virus takes time to multiply in the body. For this reason, Karan considers other information. “If I ran into someone who turned out to be sick, and then I get symptoms a few days later,” he said, “the chance is high that I have whatever they had, even if a test is negative.”
A negative result with a rapid test might mean simply that an infection hasn’t progressed enough to be detected, that the test had expired, or that it was conducted wrong. To be sure the culprit behind symptoms like a sore throat isn’t covid, researchers suggest testing again in a day or two. It often takes about three days after symptoms start for a test to register as positive, said Karan, adding that such time estimates are based on averages and that individuals may deviate from the norm.
If a person feels healthy and wants to know their status because they were around someone with covid, Karan recommends testing two to four days after the exposure. To protect others during those uncertain days, the person can wear an N95 mask that blocks the spread of the virus. If tests remain negative five days after an exposure and the person still feels fine, Chu said, they’re unlikely to be infected — and, if they are, viral levels would be so low that they would be unlikely to pass the disease to others.
Positive tests, on the other hand, reliably flag an infection. In this case, people can ask a doctor whether they qualify for the antiviral drug Paxlovid. The pills work best when taken immediately after symptoms begin so that they slash levels of the virus before it damages the body. Some studies suggest the medicine reduces a person’s risk of long covid, too, but the evidence is mixed. Another note on tests: Don’t worry if they continue to turn out positive for longer than symptoms last; the virus may linger even if it’s no longer replicating. After roughly a week since a positive test or symptoms, studies suggest, a person is unlikely to pass the virus to others.
If covid is ruled out, Karan recommends tests for influenza because they can guide doctors on whether to prescribe an antiviral to fight it — or if instead it’s a bacterial infection, in which case antibiotics may be in order. (One new home test diagnoses covid and influenza at the same time.) Whereas antivirals and antibiotics target the source of the ailment, over-the-counter medications may soothe congestion, coughs, fevers, and other symptoms. That said, the FDA recently determined that a main ingredient in versions of Sudafed, NyQuil, and other decongestants, called phenylephrine, is ineffective.
Jobs complicate a personal approach to staying healthy. Emergency-era business closures have ended, and mandates on vaccination and wearing masks have receded across the country. Some managers take precautions to protect their staff. Chu, for example, keeps air-purifying devices around her lab, and she asks researchers to stay home when they feel sick and to test themselves for covid before returning to work after a trip.
However, occupational safety experts note that many employees face risks they cannot control because decisions on if and how to protect against outbreaks, such as through ventilation, testing, and masking, are left to employers. Notably, people with low-wage and part-time jobs — occupations disproportionately held by people of color — are often least able to control their workplace environments.
Jessica Martinez, co-executive director of the National Council for Occupational Safety and Health, said the lack of national occupational standards around airborne disease protection represents a fatal flaw in the Biden administration’s decision to relinquish its control of the pandemic.
“Every workplace needs to have a plan for reducing the threat of infectious disease,” she said. “If you only focus on the individual, you fail workers.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
Put Your Feet Up! (Against A Wall, For 20 Minutes)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Feel free to browse our articles while you do
Here are 10 good reasons to give it a try; there are another 10 in the short (3:18) video:
- Improves blood circulation
- Improves blood pressure
- Relaxes the body as a whole
- Alleviates lower back tension
- Eases headaches and migraines
- Reduces knee pain
- Relieves swelling in feet and ankles
- Improves lymphatic flow
- Stretches the hamstrings (and hip flexors, if you do it wide)
- Helps quiet the mind
As for the rest…
Click Here If The Embedded Video Doesn’t Load Automatically
PS: about that circulation… As a general rule of thumb, anything that slightly confuses the heart (anatomically, not romantically) will tend to have a beneficial effect, in moderation. This goes for being upside-down (as is partly the case here), and also for high-intensity interval training (HIIT):
How To Do HIIT (Without Wrecking Your Body)
Take care!
Share This Post
-
The Knowledge That Harvard Medical School’s Clinical Instructor Dr. Monique Tello Thinks Everyone SHOULD Have About Heart Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
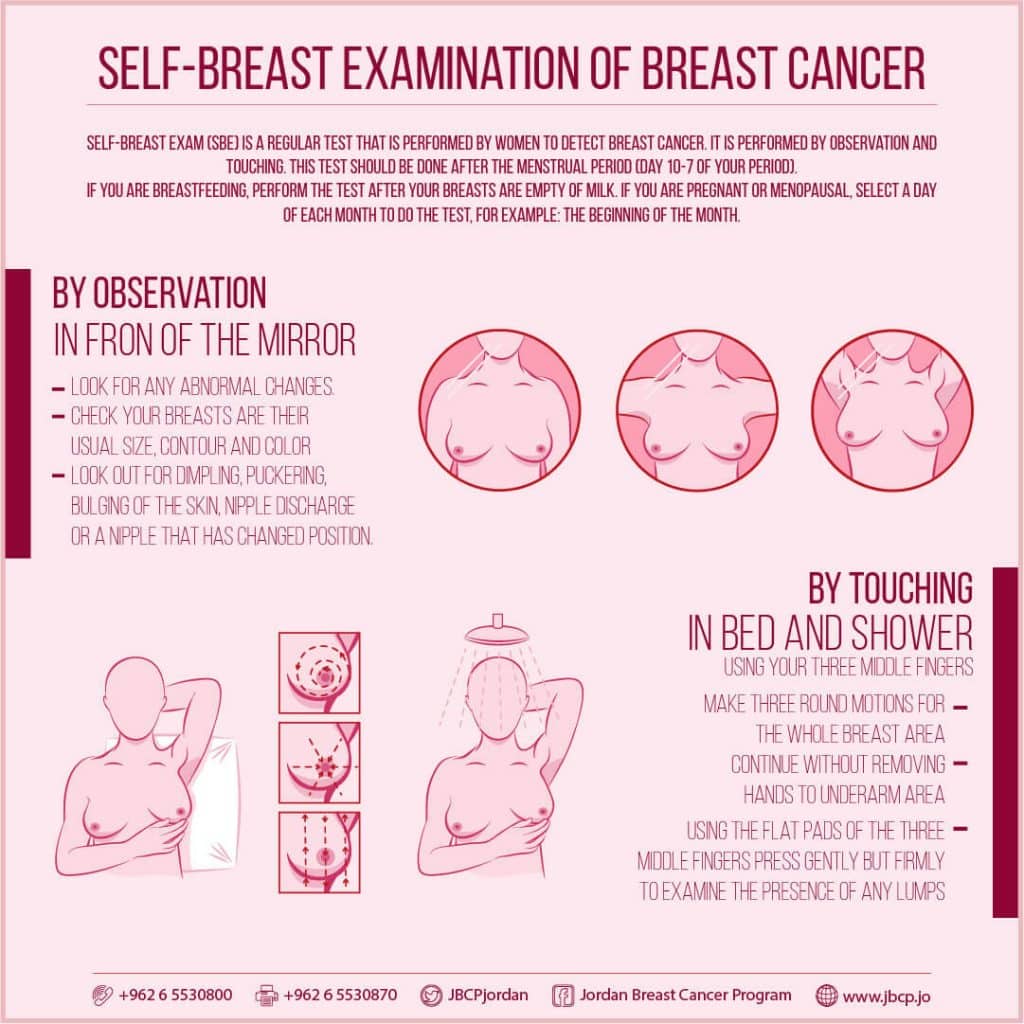
Anyone (who has not had a double mastectomy, anyway) can get breast cancer.
Breast cancer, if diagnosed early (before it spreads), has a 98% survival rate.
That survival rate drops to 31% if diagnosed after it has spread through the body.
(The US CDC’s breast cancer “stat bite” page has more stats and interactive graphs, so click here to see those charts and get the more detailed low-down on mortality/survival rates with various different situations)
We think that the difference between 98% and 31% survival rates is more than enough reason to give ourselves a monthly self-check at the very least! You’ve probably seen how-to diagrams before, but here are instructions for your convenience:
This graphic created by the Jordan Breast Cancer Program (check them out, as they have lots of resources)
If you don’t have the opportunity to take matters into your own hands right now, rather than just promise yourself “I’ll do that later”, take this free 4-minute Breast Health Assessment from Aurora Healthcare. Again, we think the difference early diagnosis can make to your survival chances make these tests well worth it.
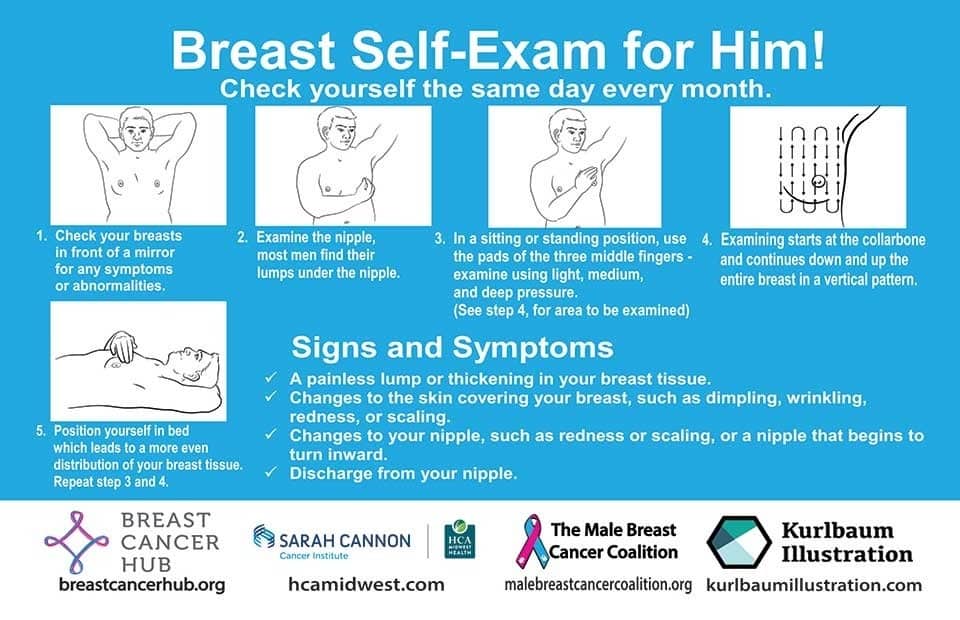
Lest we forget, men can also get breast cancer (the CDC has a page for men too), especially if over 50. But how do you check for breast cancer, when you don’t have breasts in the commonly-understood sense of the word?
So take a moment to do this (yes, really actually do it!), and set a reminder in your calendar to repeat it monthly—there really is no reason not to! Take care of yourself; you’re important.
Pssst! Did you scroll past the diagrams, looking for the online 4-minute test promised by the subtitle? If so, scroll back up; the link is in the middle!
Harvard Medical School’s Clinical Instructor’s Five-Point Plan for Heart Health
Dr. Monique Tello, M.D., M.P.H., is a practicing physician at Massachusetts General Hospital, director of research and academic affairs for the MGH DGM Healthy Lifestyle Program, clinical instructor at Harvard Medical School, and author of the evidence-based lifestyle change guide Healthy Habits for Your Heart.
Here are what she says are the five most important factors to help keep your ticker ticking:
5. Have (at most) a moderate alcohol intake! While there are polyphenols such as resveratrol in red wine that could boost heart health, there’s so little per glass that you may need 100–1000 glasses to get the dosage that provides benefits in mouse studies. If you’re not a mouse, it may not be as beneficial, and Dr. Tello recommends drinking no more than one glass per day of any alcohol. What constitutes a glass? It varies from one kind of drink to another, so here’s a handy guide.
4. Don’t smoke. Best of all to never start. But if you did, quit. Simple as that. There is no healthy amount of smoking. While paradoxically, quitting smoking may of course be stressful to you, the long term gains are considered more than worth it. As with all advice, do consult your own physician for guidance, as individual circumstances may vary, and that may change the best approach for you.
3. Maintain a healthy body weight. While BMI (Body Mass Index) is not a perfect system, it’s a system in popular use, and Dr. Tello recommends keeping a BMI between 18.5 and 24.9.
What’s your BMI? It takes into account your height and weight; here’s a Quick BMI Calculator for your convenience.
2. Keep a healthy level of physical activity—which ideally means at least 30 minutes per day vigorous activity, but obviously if you’re not used to this, take it slowly and build up over time. Even just small lifestyle changes (walking where possible, taking the stairs instead of the elevator where possible, etc) can add up to a big difference.
1. Enjoy a healthy diet. This is the single most important thing, and the best modern scientific consensus holds that the best diet contains plenty of vegetables, fruits and nuts, whole grains, and omega-3 fatty acids, while it avoids processed meats, sugar-sweetened beverages, trans fats (what are trans fats?), and too much sodium.
Share This Post
Related Posts
-
Without Medicare Part B’s Shield, Patient’s Family Owes $81,000 for a Single Air-Ambulance Flight
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Without Medicare Part B’s Shield, Patient’s Family Owes $81,000 for a Single Air-Ambulance Flight
Debra Prichard was a retired factory worker who was careful with her money, including what she spent on medical care, said her daughter, Alicia Wieberg. “She was the kind of person who didn’t go to the doctor for anything.”
That ended last year, when the rural Tennessee resident suffered a devastating stroke and several aneurysms. She twice was rushed from her local hospital to Vanderbilt University Medical Center in Nashville, 79 miles away, where she was treated by brain specialists. She died Oct. 31 at age 70.
One of Prichard’s trips to the Nashville hospital was via helicopter ambulance. Wieberg said she had heard such flights could be pricey, but she didn’t realize how extraordinary the charge would be — or how her mother’s skimping on Medicare coverage could leave the family on the hook.
Then the bill came.
The Patient: Debra Prichard, who had Medicare Part A insurance before she died.
Medical Service: An air-ambulance flight to Vanderbilt University Medical Center.
Service Provider: Med-Trans Corp., a medical transportation service that is part of Global Medical Response, an industry giant backed by private equity investors. The larger company operates in all 50 states and says it has a total of 498 helicopters and airplanes.
Total Bill: $81,739.40, none of which was covered by insurance.
What Gives: Sky-high bills from air-ambulance providers have sparked complaints and federal action in recent years.
For patients with private insurance coverage, the No Surprises Act, which went into effect in 2022, bars air-ambulance companies from billing people more than they would pay if the service were considered “in-network” with their health insurers. For patients with public coverage, such as Medicare or Medicaid, the government sets payment rates at much lower levels than the companies charge.
But Prichard had opted out of the portion of Medicare that covers ambulance services.
That meant when the bill arrived less than two weeks after her death, her estate was expected to pay the full air-ambulance fee of nearly $82,000. The main assets are 12 acres of land and her home in Decherd, Tennessee, where she lived for 48 years and raised two children. The bill for a single helicopter ride could eat up roughly a third of the estate’s value, said Wieberg, who is executor.
The family’s predicament stems from the complicated nature of Medicare coverage.
Prichard was enrolled only in Medicare Part A, which is free to most Americans 65 or older. That section of the federal insurance program covers inpatient care, and it paid most of her hospital bills, her daughter said.
But Prichard declined other Medicare coverage, including Part B, which handles such things as doctor visits, outpatient treatment, and ambulance rides. Her daughter suspects she skipped that coverage to avoid the premiums most recipients pay, which currently are about $175 a month.
Loren Adler, a health economist for the Brookings Institution who studies ambulance bills, estimated the maximum charge that Medicare would have allowed for Prichard’s flight would have been less than $10,000 if she’d signed up for Part B. The patient’s share of that would have been less than $2,000. Her estate might have owed nothing if she’d also purchased supplemental “Medigap” coverage, as many Medicare members do to cover things like coinsurance, he said.
Nicole Michel, a spokesperson for Global Medical Response, the ambulance provider, agreed with Adler’s estimate that Medicare would have limited the charge for the flight to less than $10,000. But she said the federal program’s payment rates don’t cover the cost of providing air-ambulance services.
“Our patient advocacy team is actively engaged with Ms. Wieberg’s attorney to determine if there was any other applicable medical coverage on the date of service that we could bill to,” Michel wrote in an email to KFF Health News. “If not, we are fully committed to working with Ms. Wieberg, as we do with all our patients, to find an equitable solution.”
The Resolution: In mid-February, Wieberg said the company had not offered to reduce the bill.
Wieberg said she and the attorney handling her mother’s estate both contacted the company, seeking a reduction in the bill. She said she also contacted Medicare officials, filled out a form on the No Surprises Act website, and filed a complaint with Tennessee regulators who oversee ambulance services. She said she was notified Feb. 12 that the company filed a legal claim against the estate for the entire amount.
Wieberg said other health care providers, including ground ambulance services and the Vanderbilt hospital, wound up waiving several thousand dollars in unpaid fees for services they provided to Prichard that are normally covered by Medicare Part B.
But as it stands, Prichard’s estate owes about $81,740 to the air-ambulance company.
More from Bill of the Month
- The Colonoscopies Were Free. But the ‘Surgical Trays’ Came With $600 Price Tags. Jan 25, 2024
- When a Quick Telehealth Visit Yields Multiple Surprises Beyond a Big Bill Dec 19, 2023
- Out for Blood? For Routine Lab Work, the Hospital Billed Her $2,400 Nov 21, 2023
The Takeaway: People who are eligible for Medicare are encouraged to sign up for Part B, unless they have private health insurance through an employer or spouse.
“If someone with Medicare finds that they are having difficulty paying the Medicare Part B premiums, there are resources available to help compare Medicare coverage choices and learn about options to help pay for Medicare costs,” Meena Seshamani, director of the federal Center for Medicare, said in an email to KFF Health News.
She noted that every state offers free counseling to help people navigate Medicare.
In Tennessee, that counseling is offered by the State Health Insurance Assistance Program. Its director, Lori Galbreath, told KFF Health News she wishes more seniors would discuss their health coverage options with trained counselors like hers.
“Every Medicare recipient’s experience is different,” she said. “We can look at their different situations and give them an unbiased view of what their next best steps could be.”
Counselors advise that many people with modest incomes enroll in a Medicare Savings Program, which can cover their Part B premiums. In 2023, Tennessee residents could qualify for such assistance if they made less than $1,660 monthly as a single person or $2,239 as a married couple. Many people also could obtain help with other out-of-pocket expenses, such as copays for medical services.
Wieberg, who lives in Missouri, has been preparing the family home for sale.
She said the struggle over her mother’s air-ambulance bill makes her wonder why Medicare is split into pieces, with free coverage for inpatient care under Part A, but premiums for coverage of other crucial services under Part B.
“Anybody past the age of 70 is likely going to need both,” she said. “And so why make it a decision of what you can afford or not afford, or what you think you’re going to use or not use?”
Bill of the Month is a crowdsourced investigation by KFF Health News and NPR that dissects and explains medical bills. Do you have an interesting medical bill you want to share with us? Tell us about it!
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
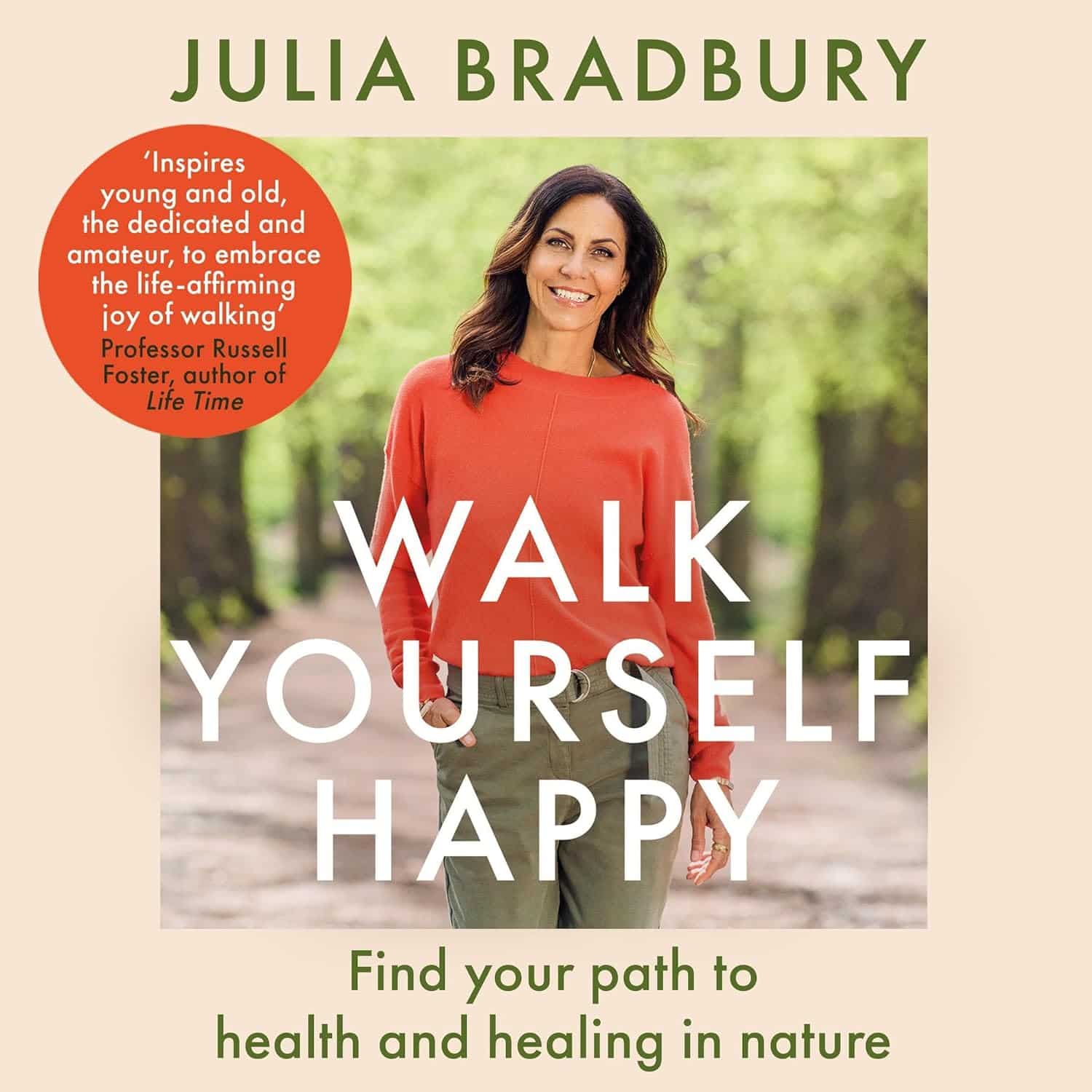
Walk Yourself Happy – by Dr. Julia Bradbury
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Notwithstanding her (honorary) doctorate, Dr. Bradbury is not, in fact, a scientist. But…
- She has a lot of experience walking all around the world, and her walking habit has seen her through all manner of things, from stress and anxiety to cancer and grief and more.
- She does, throughout this book, consult many scientists and other experts (indeed, some we’ve featured here before at 10almonds), so we still get quite a dose of science too.
The writing style of this book is… Compelling. Honestly, the biggest initial barrier to you getting out of the door will be putting this book down first.If you have good self-discipline, you might make it last longer by treating yourself to a chapter per day
Bottom line: you probably don’t need this book to know how to go for a walk, but it will motivate, inspire, and even inform you of how to get the most out of it. Treat yourself!
Click here to check out Walk Yourself Happy, and prepare for a new healthy habit!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Reading At Night: Good Or Bad For Sleep? And Other Questions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Would be interested in your views about “reading yourself to sleep”. I find that current affairs magazines and even modern novels do exactly the opposite. But Dickens – ones like David Copperfield and Great Expectations – I find wonderfully effective. It’s like entering a parallel universe where none of your own concerns matter. Any thoughts on the science that may explain this?!❞
Anecdotally: this writer is (like most writers) a prolific reader, and finds reading some fiction last thing at night is a good way to create a buffer between the affairs of the day and the dreams of night—but I could never fall asleep that way, unless I were truly sleep-deprived. The only danger is if I “one more chapter” my way deep into the night! For what it’s worth, bedtime reading for me means a Kindle self-backlit with low, soft lighting.
Scientifically: this hasn’t been a hugely researched area, but there are studies to work from. But there are two questions at hand (at least) here:
- one is about reading, and
- the other is about reading from electronic devices with or without blue light filters.
Here’s a study that didn’t ask the medium of the book, and concluded that reading a book in bed before going to sleep improved sleep quality, compared to not reading a book in bed:
Here’s a study that concluded that reading on an iPad (with no blue light filter) that found no difference in any metrics except EEG (so, there was no difference on time spent in different sleep states or sleep onset latency), but advised against it anyway because of the EEG readings (which showed slow wave activity being delayed by approximately 30 minutes, which is consistent with melatonin production mechanics):
Here’s another study that didn’t take EEG readings, and/but otherwise confirmed no differences being found:
We’re aware this goes against general “sleep hygiene” advice in two different ways:
- General advice is to avoid electronic devices before bedtime
- General advice is to not do activities besides sleep (and sex) in bed
…but, we’re committed to reporting the science as we find it!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: