How To Be 7.5x More Likely To Develop Chronic Fatigue Syndrome
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what is it?
Many more people have chronic fatigue, which is the symptom of being exhausted all the time, than have chronic fatigue syndrome (CFS) which is the illness of myalgic encephalomyelitis (ME).
This is because fatigue can be a symptom of many, many other conditions, and can be heavily influenced by lifestyle factors too.
A lot of the advice for dealing with chronic fatigue is often the same in both cases, but some will be different, because for example:
- If your fatigue is from some other condition, that condition probably impacts what lifestyle factors you are (and are not) able to change, too
- If your fatigue is from lifestyle factors, that hopefully means you can change those and enjoy less fatigue…
- But if it’s not from lifestyle factors, as in ME/CFS, then advice to “exercise more” etc is not going to help so much.
There are ways to know the difference though:
Check out: Do You Have Chronic Fatigue Syndrome?
The chronic disease pipeline
While it had been strongly suspected that COVID infection could lead to CFS, with long COVID having chronic fatigue as one of its characteristic symptoms, a research team led by Dr. Suzanne Vernon has now established the nature of the relationship.
It was a large (n=13,224) longitudinal observational cohort study of people with no pre-existing ME/CFS, grouped according to their COVID infection status:
- acute infected, enrolled within 30 days of infection or enrolled as uninfected who became infected (n=4,515)
- post-acute infected, enrolled greater than 30 days after infection (n=7,270)
- uninfected (n=1,439).
(to be clear, that last means “never infected”, or else they would be in group 2)
Note: people who had COVID and were hospitalized for it were excluded from the study, so this risk is the risk represented by even just more “moderate” infections.
What they found:
❝The proportion of all RECOVER-Adult participants that met criteria for ME/CFS following SARS-CoV-2 infection was 4.5% (531 of 11,785) compared to 0.6% (9 of 1439) in uninfected participants.❞
There are then different numbers if we look per 100 person-years, as the study also did—in which case, we get a re-modelled increase in risk of 5x instead of 7.5x, but a) that’s still not good b) the “here-and-now” figures of 4.5% vs 0.6% are also relevant.
Read in full: Incidence and Prevalence of Post-COVID-19 Myalgic Encephalomyelitis: A Report from the Observational RECOVER-Adult Study
The killer nobody wants to talk about anymore
Of course, as we all know the pandemic is over, because politicians declared it so, which is very reassuring.
Nevertheless, COVID is currently the still 4th leading cause of death in the US, placing it higher than stroke, Alzheimer’s, diabetes, and others.
See also: Emergency or Not, Covid Is Still Killing People. Here’s What Doctors Advise to Stay Safe
So, while it’s very good to take care of our hearts, brains, blood sugars, and so forth, let’s at the very least continue to keep on top of our vaccinations, avoid enclosed crowded spaces where possible, etc.
And for extra boosts to one’s chances: Why Some People Get Sick More (And How To Not Be One Of Them)
What if I do get (or already have) long COVID and/or ME/CFS?
Well, that is definitely going to suck, but there are still some things that can be done.
Here’s a big one: How To Eat To Beat Chronic Fatigue ← this will not, of course, cure you, but it’s a way of getting maximum nutrition for minimum effort, given that for someone with chronic fatigue, effort is a very finite resource that must be used sparingly
Finally, here are some further resources:
Support For Long COVID & Chronic Fatigue
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Think Again – by Adam Grant
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Warning: this book may cause some feelings of self-doubt! Ride them out and see where they go, though.
It was Socrates who famously (allegedly) said “ἓν οἶδα ὅτι οὐδὲν οἶδα”—”I know that I know nothing”.
Adam Grant wants us to take this philosophy and apply it usefully to modern life. How?
The main premise is that rethinking our plans, answers and decisions is a good thing… Not a weakness. In contrast, he says, a fixed mindset closes us to opportunities—and better alternatives.
He wants us to be sure that we don’t fall into the trap of the Dunning-Kruger Effect (overestimating our abilities because of being unaware of how little we know), but he also wants us to rethink whole strategies, too. For example:
Grant’s approach to interpersonal conflict is very remniscent of another book we might review sometime, “Aikido in Everyday Life“. The idea here is to not give in to our knee-jerk responses to simply retaliate in kind, but rather to sidestep, pivot, redirect. This is, admittedly, the kind of “rethinking” that one usually has to rethink in advance—it’s too late in the moment! Hence the value of a book.
Nor is the book unduly subjective. “Wishy-washiness” has a bad rep, but Grant gives us plenty in the way of data and examples of how we can, for example, avoid losses by not doubling down on a mistake.
What, then, of strongly-held core principles? Rethinking doesn’t mean we must change our mind—it simply means being open to the possibility in contexts where such makes sense.
Grant borrows, in effect, from:
❝Do the best you can until you know better. Then when you know better… do better!❞
So, not so much undercutting the principles we hold dear, and instead rather making sure they stand on firm foundations.
All in all, a thought-provokingly inspiring read!
Share This Post
-
How To Heal Psoriasis Naturally
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Nutritionist Julia Davies explains the gut-skin connection (& how to use it to your advantage) in this video:
Inside out
Psoriasis is a chronic autoimmune skin condition, in which the skin renewal process accelerates from 28 days (normal) to 3–5 days, leading to red, scaly patches. It most commonly affects the outer joints (especially elbows & knees) but can appear anywhere, including the scalp and torso.
Autoimmune diseases are often linked to gut barrier integrity issues, as leaky gut syndrome allows toxins/food particles to penetrate the gut lining, triggering an immune response, which means inflammation.
Standard treatments often include topical or systemic immunosuppressants, such as steroids. Such medications suppress the immune response (and thus the symptoms) but they don’t address root causes.
What to do about it, from the root
As you might imagine, part of the key is a non-inflammatory (or ideally, anti-inflammatory) diet. This means starting by removing likely triggers; gluten sensitivity is common so that’s near the top of the list.
At the very top of the list though is sugar*, which is not only pro-inflammatory but also feeds candida in the gut, which is a major driver of leaky gut, as the fungus puts its roots through your intestines (that’s as bad as it sounds).
*as usual, sugar that comes with adequate fiber, such as whole fruit, is fine. Fruit juice, however, is not.
It is likely to see early improvements within 6 weeks, and significant improvement (such as being mostly symptom-free) can take 6–8 months, so don’t give up if it’s day 3 and you’re not cured yet. This is a marathon not a sprint, and you’ll need to maintain things or the psoriasis may return.
In the meantime, it is recommended to do all you reasonably can to help your gut to repair itself, which means a good amount of fiber, and occasional probiotics. Also, focusing on whole, nutrient-dense foods will of course reduce inflammation and improve energy—which can be a big deal, as psoriasis is often associated with fatigue, both because inflammation itself is exhausting (the body is very active, on a cellular level), and because a poor diet is not invigorating.
Outside of diet, stress is often a trigger for flare-ups, so try to manage that too, of course.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Of Brains & Breakouts: The Brain-Skin Doctor
Take care!
Share This Post
-
How Much Can Hypnotherapy Really Do?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sit Back, Relax, And…
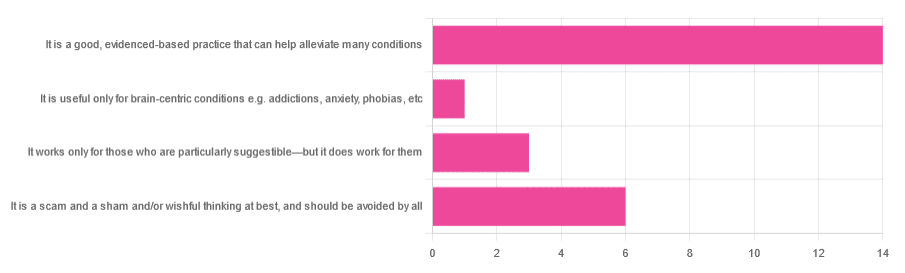
In Tuesday’s newsletter, we asked you for your opinions of hypnotherapy, and got the above-depicted, below-described, set of responses:
- About 58% said “It is a good, evidenced-based practice that can help alleviate many conditions”
- Exactly 25% said “It is a scam and sham and/or wishful thinking at best, and should be avoided by all”
- About 13% said “It works only for those who are particularly suggestible—but it does work for them”
- One (1) person said “It is useful only for brain-centric conditions e.g. addictions, anxiety, phobias, etc”
So what does the science say?
Hypnotherapy is all in the patient’s head: True or False?
True! But guess which part of your body controls much of the rest of it.
So while hypnotherapy may be “all in the head”, its effects are not.
Since placebo effect, nocebo effect, and psychosomatic effect in general are well-documented, it’s quite safe to say at the very least that hypnotherapy thus “may be useful”.
Which prompts the question…
Hypnotherapy is just placebo: True or False?
False, probably. At the very least, if it’s placebo, it’s an unusually effective placebo.
And yes, even though testing against placebo is considered a good method of doing randomized controlled trials, some placebos are definitely better than others. If a placebo starts giving results much better than other placebos, is it still a placebo? Possibly a philosophical question whose answer may be rooted in semantics, but happily we do have a more useful answer…
Here’s an interesting paper which: a) begins its abstract with the strong, unequivocal statement “Hypnosis has proven clinical utility”, and b) goes on to examine the changes in neural activity during hypnosis:
Brain Activity and Functional Connectivity Associated with Hypnosis
It works only for the very suggestible: True or False?
False, broadly. As with any medical and/or therapeutic procedure, a patient’s expectations can affect the treatment outcome.
And, especially worthy of note, a patient’s level of engagement will vastly affect it treatment that has patient involvement. So for example, if a doctor prescribes a patient pills, which the patient does not think will work, so the patient takes them intermittently, because they’re slow to get the prescription refilled, etc, then surprise, the pills won’t get as good results (since they’re often not being taken).
How this plays out in hypnotherapy: because hypnotherapy is a guided process, part of its efficacy relies on the patient following instructions. If the hypnotherapist guides the patient’s mind, and internally the patient is just going “nope nope nope, what a lot of rubbish” then of course it will not work, just like if you ask for directions in the street and then ignore them, you won’t get to where you want to be.
For those who didn’t click on the above link by the way, you might want to go back and have a look at it, because it included groups of individuals with “high/low hypnotizability” per several ways of scoring such.
It works only for brain-centric things, e.g. addictions, anxieties, phobias, etc: True or False?
False—but it is better at those. Here for example is the UK’s Royal College of Psychiatrists’ information page, and if you go to “What conditions can hypnotherapy help to treat”, you’ll see two broad categories; the first is almost entirely brain-stuff; the second is more varied, and includes pain relief of various kinds, burn care, cancer treatment side effects, and even menopause symptoms. Finally, warts and other various skin conditions get their own (positive) mention, per “this is possible through the positive effects hypnosis has on the immune system”:
RCPsych | Hypnosis And Hypnotherapy
Wondering how much psychosomatic effect can do?
You might like this previous article; it’s not about hypnotherapy, but it is about the difference the mind can make on physical markers of aging:
Aging, Counterclockwise: When Age Is A Flexible Number
Take care!
Share This Post
Related Posts
-
The Little-Known Truth…
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Myth-Buster, Myth-Buster, Bust Us A Myth (or three!)
Let’s can this myth for good
People think of “canned foods” as meaning “processed foods” and therefore bad. But the reality is it’s all dependent on what’s in the can (check the ingredients!). And as for nutrients?
Many canned fruits and vegetables contain more nutrients than fresh ones! This is because the way they’ve been stored preserves them better. For example:
- Canned tomatoes contain more bioavailable lycopene than fresh
- Canned spinach contains more bioavailable carotene than fresh
- Canned corn contains more bioavailable lutein than fresh
- The list goes on, but you get the idea!
Don’t Want To Take Our Word For It? Read The Scientific Paper Here!
Gaslight, Gymkeep, Girl-loss?
Many women and girls avoid doing weight-training as part of their exercise—or use only the smallest weights—to avoid “bulking up” and “looking like a man”.
Many men, meanwhile, wish it were that easy to bulk up!
The reality is that nobody, unless you have very rare genes, packs on a lot of muscle by accident. Even with the genes for it, it won’t happen unless you’re also eating for it!
Resistance-based strength training (such as lifting weights), is a great way for most people to look after an important part of their long-term health: bone density!
You can’t have strong muscles on weak bones, so strengthening the muscles cues the body to strengthen the bones. In short, your strength-training at age 45 or 55 (or earlier) could be what helps you avoid a broken hip at 65 or 75.
We’re Not Kidding, It Really Is That Important (Read The Study Here)!
Something doesn’t smell right about this
There’s been a big backlash against anti-perspirants and deodorants. The popular argument is that the aluminium in them causes cancer.
This led to many people buying “deodo-rocks”, crystal rocks that can be run under water and then rubbed on the armpits to deodorize “naturally”. But, those crystal rocks are actually alum crystals (guess what they contain…).
The belief that deodorants cause cancer came from studies done by applying deodorant to cells (like the canine kidney cells in this study) in petri dishes. So, assuming you don’t cut out your kidney and then spray it directly with the deodorant, the jury is still out!
A more recent systematic review sorted out quite clearly the ways in which aluminium was, or was not, harmful, and said:
❝Neither is there clear evidence to show use of Al-containing underarm antiperspirants or cosmetics increases the risk of Alzheimer’s Disease or breast cancer. Metallic Al, its oxides, and common Al salts have not been shown to be either genotoxic or carcinogenic.❞
Critical Reviews in Toxicology
…but also says that you should avoid eating aluminium while pregnant or breastfeeding. We hope you can resist the urge.
See The Summary For Yourself Here!
(actually the whole article is there, but we know you value condensed knowledge, so: the abstract at the top will probably tell you all you want to know!)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Eat To Beat Hyperthyroidism!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Would love to see more on eating vegan. I am allergic to soy in any form which seems to be in everything❞
There is a lot of it about, isn’t there? Happily, these days, a lot of meat and dairy alternatives are also made from other sources, for example pea protein is getting used a lot more nowadays in meat substitutes, and there are many kinds of alternatives to dairy (e.g. nut milks, oat milk, hemp milk, and—which is a branding nightmare but very healthy—pea milk).
You might like these previous main features of ours:
- Do We Need Animal Products To Be Healthy?
- The Whys and Hows of Cutting Down Meat Consumption
- Plant-Based Milks—What’s Best?
Also, if doing a whole foods plant-based diet, lentils (especially brown lentils) can be used as a great substitute for minced beef/lamb in recipes that call for such.
Boil the lentils (a liter of water to a cup of lentils is great; use a rice cooker if you have one!) along with the seasonings you will use (herbs appropriate to your dish, and then: black pepper is always good; you shouldn’t need to add salt; a teaspoon of low-sodium yeast extract is great though, or to really get the best nutritional benefits, nooch).
When it is done, you shouldn’t have excess water now, so just use as is, or if you want a slightly fatty kick, fry briefly in a little extra virgin olive oil, before using it however you were planning to use it.
Enjoy!
❝What foods should I eat for hyperthyroidism? My doctor tells me what foods to avoid, but not what to eat❞
Great question! We’ll have to do a main feature on hyperthyroidism one of these days, as so far we’ve only done features on hypothyroidism:
As for hyperthyroidism…
Depending on your medications, your doctor might recommend a low iodine diet. If so, then you might want to check out:
American Thyroid Association | Low Iodine Diet Plan
…for recommendations.
But in a way, that’s still a manner of “what to avoid” (iodine) and then the foods to eat to avoid that.
You may be wondering: is there any food that actively helps against hyperthyroidism, as opposed to merely does not cause problems?
And the answer is: yes!
Cruciferous vegetables (e.g. cabbage, sprouts, broccoli, cauliflower, etc) contain goitrin, which in immoderate quantities can cause problems for people with hypothyroidism because it can reduce thyroid hormone synthesis. If you have hyperthyroidism, however, this can work in your favor.
Read more: The role of micronutrients in thyroid dysfunction
The above paper focuses on children, but it was the paper we found that explains it most clearly while showing good science. However, the same holds true for adults:
Notwithstanding that the title comes from the angle of examining hypothyroidism, the mechanism of action makes clear its beneficence in the case of hyperthyroidism.
Selenium is also a great nutrient in the case of autoimmune hyperthyroidism, because it is needed to metabolize thyroid hormone (if you don’t metabolize it, it’ll just build up):
Selenium and Thyroid Disease: From Pathophysiology to Treatment
The absolute top best dietary source of selenium is Brazil nuts, to the point that people without hyperthyroidism have to take care to not eat more than a few per day (because too much selenium could then cause problems):
NIH | Selenium Fact Sheet for Health Professionals
(this contains information on the recommended amount, the upper limit amount, how much is in Brazil nuts and other foods, and what happens if you get too much or too little)
Note: after Brazil nuts (which are about 5 times more rich in selenium than the next highest source), the other “good” sources of selenium—mostly various kinds of fish—are also “good” source of iodine, so you might want to skip those.
Want more ideas?
You might like this from LivHealth:
Hyperthyroidism Diet: 9 Foods To Ease Symptoms
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Lupus Solution – by Dr. Tiffany Caplan & Dr. Brent Caplan
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Lupus is not fun, and this book sets out to make it easier.
Starting off by explaining the basics of autoimmunity and how lupus works, the authors go on the address the triggers of lupus and how to avoid them—which if you’ve been suffering from lupus for a while, you probably know this part already, but it’s as well to give them a look over just in case you missed something.
The real value of the book though comes in the 8 chapters of the section “Tools & Therapies” which are mostly lifestyle adjustments though there are additionally some pharmaceutical approaches that can also help, and they are explained too. And no, it’s not just “reduce inflammation” (but yes, also that); rather, a whole array of things are examined that often aren’t thought of as related to lupus, but in fact can have a big impact.
The style is to-the-point and informational, and formatted for ease of reading. It doesn’t convey more hard science than necessary, but it does have a fair bibliography at the back.
It’s a short book, weighing in at 182 pages. If you want something more comprehensive, check out our review of The Lupus Encyclopedia, which is 848 pages of information-dense text and diagrams.
Bottom line: if you have lupus and would like fewer symptoms, this book can help you with that quite a bit without getting so technical as the aforementioned encyclopedia.
Click here to check out The Lupus Solution, and live more comfortably!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: