Top 8 Habits Of The Top 1% Healthiest Over-50s
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Will Harlow, over-50s specialist physio, compiled some stats from over a thousand over-50s clients:
Checklist
The findings:
- Consistency: the healthiest individuals practised some kind(s) of health habit daily. Consistency was emphasized as more important than perfection.
- Resistance training: 75% of the sample engaged in resistance training for better mobility, strength, and mental health. Not all used gyms; some used household objects like bags of books or resistance bands.
- Walking: everyone walked at least 6,000 steps per day, often briskly. Walking speed, not just step count, made a significant difference
- Purpose: most participants (bearing in mind that 80% of the total sample were retired) engaged in purposeful activities like volunteering, joining groups, or writing. Having a sense of purpose correlated with longer and healthier lives.
- Flexible dieting: participants paid attention to their eating without strictly following specific diets. Portion size discipline and consistency (eating well 90% of the time) were key.
- Mobility: they worked on joint stiffness with regular mobility and stretching routines. And, importantly, they do not accept stiffness as inevitable.
- Social engagement: they maintained at-least-weekly social contact (e.g. clubs, family meetups, outings). Social isolation, in contrast, was linked to severe health risks like dementia and early death.
- Positivity: participants maintained a positive attitude despite hardships, focussing on the things they could control. Broader scientific consensus supports the premise that a positive outlook improves health and longevity.
10almonds note: we’re curious as to how causality was established in some of these, since (for example) it could easily be that someone who is in better health will more readily walk more quickly, meaning that a higher walking speed was not necessarily such a causative factor in good health, but rather a result thereof. Of course, there may also be a degree of two-way causality, but still, we like good science and there seem to be some leaps of logic here that have otherwise gone unacknowledged.
This does not take away from the fact that those eight things are most certainly good things to be doing for one’s health, all the same.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Life After Death? (Your Life; A Loved One’s Death)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Show Must Go On
We’ve previously written about the topics of death and dying. It’s not cheery, but it is important to tackle.
Sooner is better than later, in the case of:
Preparations For Managing Your Own Mortality
And for those who are left behind, of course it is hardest of all:
What Grief Does To Your Body (And How To Manage It)
But what about what comes next? For those who are left behind, that is.
Life goes on
In cases when the death is that of a close loved one, the early days after death can seem like a surreal blur. How can the world go ticking on as normal when [loved one] is dead?
But incontrovertibly, it does, so we can only ask again: how?
And, we get to choose that, to a degree. The above-linked article about grief gives a “101” rundown, but it’s (by necessity, for space) a scant preparation for one of the biggest challenges in life that most of us will ever face.
For many people, processing grief involves a kind of “saying goodbye”. For others, it doesn’t, as in the following cases of grieving the loss of one’s child—something no parent should ever have to face, but it happens:
Dr. Ken Druck | The Love That Never Dies
(with warning, the above article is a little heavy)
In short: for those who choose not to “say goodbye” in the case of the death of a loved one, it’s more often not a case of cold neglect, but rather the opposite—a holding on. Not in the “denial” sense of holding on, but rather in the sense of “I am not letting go of this feeling of love, no matter how much it might hurt to hold onto; it’s all I have”.
What about widows, and love after death?
Note: we’ll use the feminine “widow” here as a) it’s the most common and b) most scientific literature focuses on widows, but there is no reason why most of the same things won’t also apply to widowers.
We say “most”, as society does tend to treat widows and widowers differently, having different expectations about a respectful mourning period, one’s comportment during same, and so on.
As an aside: most scientific literature also assumes heterosexuality, which is again statistically reasonable, and for the mostpart the main difference is any extra challenges presented by non-recognition of marriages, and/or homophobic in-laws. But otherwise, grief is grief, and as the saying goes, love is love.
One last specificity before we get into the meat of this: we are generally assuming marriages to be monogamous here. Polyamorous arrangements will likely sidestep most of these issues completely, but again, they’re not the norm.
Firstly, there’s a big difference between remarrying (or similar) after being widowed, and remarrying (or similar) after a divorce, and that largely lies in the difference of how they begin. A divorce is (however stressful it may often be) more often seen as a transition into a new period of freedom, whereas bereavement is almost always felt as a terrible loss.
The science, by the way, shows the stats for this; people are less likely to remarry, and slower to remarry if they do, in instances of bereavement rather than divorce, for example:
Timing of Remarriage Among Divorced and Widowed Parents
Love after death: the options
For widows, then, there seem to be multiple options:
- Hold on to the feelings for one’s deceased partner; never remarry
- Grieve, move on, find new love, relegating the old to history
- Try to balance the two (this is tricky but can be done*)
*Why is balancing the two tricky, and how can it be done?
It’s tricky because ultimately there are three people’s wishes at hand:
- The deceased (“they would want me to be happy” vs “I feel I would be betraying them”—which two feelings can also absolutely come together, by the way)
- Yourself (whether you actually want to get a new partner, or just remain single—this is your 100% your choice either way, and your decision should be made consciously)
- The new love (how comfortable are they with your continued feelings for your late love, really?)
And obviously only two of the above can be polled for opinions, and the latter one might say what they think we want to hear, only to secretly and/or later resent it.
One piece of solid advice for the happily married: talk with your partner now about how you each would feel about the other potentially remarrying in the event of your death. Do they have your pre-emptive blessing to do whatever, do you ask a respectable mourning period first (how long?), would the thought just plain make you jealous? Be honest, and bid your partner be honest too.
One piece of solid advice for everyone: make sure you, and your partner(s), as applicable, have a good emotional safety net, if you can. Close friends or family members that you genuinely completely trust to be there through thick and thin, to hold your/their hand through the emotional wreck that will likely follow.
Because, while depression and social loneliness are expected and looked out for, it’s emotional loneliness that actually hits the hardest, for most people:
Longitudinal Examination of Emotional Functioning in Older Adults After Spousal Bereavement
…which means that having even just one close friend or family member with whom one can be at one’s absolute worst, express emotions without censure, not have to put on the socially expected appearance of emotional stability… Having that one person (ideally more, but having at least one is critical) can make a huge difference.
But what if a person has nobody?
That’s definitely a hard place to be, but here’s a good starting point:
How To Beat Loneliness & Isolation
Take care!
Share This Post
-
Yes, you still need to use sunscreen, despite what you’ve heard on TikTok
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Summer is nearly here. But rather than getting out the sunscreen, some TikTokers are urging followers to chuck it out and go sunscreen-free.
They claim it’s healthier to forgo sunscreen to get the full benefits of sunshine.
Here’s the science really says.
Karolina Grabowska/Pexels How does sunscreen work?
Because of Australia’s extreme UV environment, most people with pale to olive skin or other risk factors for skin cancer need to protect themselves. Applying sunscreen is a key method of protecting areas not easily covered by clothes.
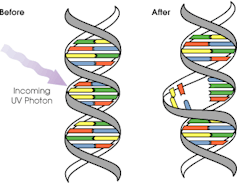
Sunscreen works by absorbing or scattering UV rays before they can enter your skin and damage DNA or supportive structures such as collagen.
When UV particles hit DNA, the excess energy can damage our DNA. This damage can be repaired, but if the cell divides before the mistake is fixed, it causes a mutation that can lead to skin cancers.
The energy from a particle of UV (a photon) causes DNA strands to break apart and reconnect incorrectly. This causes a bump in the DNA strand that makes it difficult to copy accurately and can introduce mutations. NASA/David Herring The most common skin cancers are basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). Melanoma is less common, but is the most likely to spread around the body; this process is called metastasis.
Two in three Australians will have at least one skin cancer in their lifetime, and they make up 80% of all cancers in Australia.
Around 99% of skin cancers in Australia are caused by excessive exposure to UV radiation.
Excessive exposure to UV radiation also affects the appearance of your skin. UVA rays are able to penetrate deep into the skin, where they break down supportive structures such as elastin and collagen.
This causes signs of premature ageing, such as deep wrinkling, brown or white blotches, and broken capillaries.
Sunscreen can help prevent skin cancers
Used consistently, sunscreen reduces your risk of skin cancer and slows skin ageing.
In a Queensland study, participants either used sunscreen daily for almost five years, or continued their usual use.
At the end of five years, the daily-use group had reduced their risk of squamous cell carcinoma by 40% compared to the other group.
Ten years later, the daily use group had reduced their risk of invasive melanoma by 73%
Does sunscreen block the health-promoting properties of sunlight?
The answer is a bit more complicated, and involves personalised risk versus benefit trade-offs.
First, the good news: there are many health benefits of spending time in the sun that don’t rely on exposure to UV radiation and aren’t affected by sunscreen use.
Sunscreen only filters UV rays, not all light. Ron Lach/Pexels Sunscreen only filters UV rays, not visible light or infrared light (which we feel as heat). And importantly, some of the benefits of sunlight are obtained via the eyes.
Visible light improves mood and regulates circadian rhythm (which influences your sleep-wake cycle), and probably reduces myopia (short-sightedness) in children.
Infrared light is being investigated as a treatment for several skin, neurological, psychiatric and autoimmune disorders.
So what is the benefit of exposing skin to UV radiation?
Exposing the skin to the sun produces vitamin D, which is critical for healthy bones and muscles.
Vitamin D deficiency is surprisingly common among Australians, peaking in Victoria at 49% in winter and being lowest in Queensland at 6% in summer.
Luckily, people who are careful about sun protection can avoid vitamin D deficiency by taking a supplement.
Exposing the skin to UV radiation might have benefits independent of vitamin D production, but these are not proven. It might reduce the risk of autoimmune diseases such as multiple sclerosis or cause release of a chemical that could reduce blood pressure. However, there is not enough detail about these benefits to know whether sunscreen would be a problem.
What does this mean for you?
There are some benefits of exposing the skin to UV radiation that might be blunted by sunscreen. Whether it’s worth foregoing those benefits to avoid skin cancer depends on how susceptible you are to skin cancer.
If you have pale skin or other factors that increase you risk of skin cancer, you should aim to apply sunscreen daily on all days when the UV index is forecast to reach 3.
If you have darker skin that rarely or never burns, you can go without daily sunscreen – although you will still need protection during extended times outdoors.
For now, the balance of evidence suggests it’s better for people who are susceptible to skin cancer to continue with sun protection practices, with vitamin D supplementation if needed.
Katie Lee, PhD Candidate, Dermatology Research Centre, The University of Queensland and Rachel Neale, Principal research fellow, QIMR Berghofer Medical Research Institute
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
What is reformer pilates? And is it worth the cost?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Reformer pilates is steadily growing in popularity, with new studios opening regularly in major cities all over the world.
But what exactly is reformer pilates? And how does it compare with regular pilates and other types of exercise?
Classes aren’t cheap so let’s look at the potential benefits and drawbacks to help you decide if it’s right for you.
Ahmet Kurt/Unsplash Pilates with special equipment
Pilates is a mode of exercise that focuses on core stability and flexibility, while also addressing muscular strength and endurance, balance and general fitness. At first glance, it might look a bit like yoga, with some more traditional weight training components thrown in.
Reformer pilates uses a piece of equipment called a “reformer”. This looks like a narrow bed that slides along a carriage, has straps to hold onto, and has adjustable springs that add resistance to movement. You perform pilates on the reformer to target specific muscle groups and movement patterns.
The reformer was first designed to help people recover from injuries. However, it has now become common for general fitness and even sports performance.
Unlike normal pilates, also known as “mat pilates”, which only uses your body weight, the reformer adds resistance, meaning you can change the difficulty according to your current level of fitness.
This not only provides a way to overload your muscles, but can make the exercise session more aerobically demanding, which has been proposed to improve cardiovascular fitness.
Mat pilates uses your body weight. Kampus Productions/Pexels What are the benefits of reformer pilates?
Despite being around for decades, there is surprisingly little research looking at the benefits of reformer pilates. However, what we have seen so far suggests it has a similar effect to other modes of exercise.
Reformer pilates has been shown to help with weight loss, cause some small increases in muscle mass, and enhance cognitive function. All of these benefits are commonly seen when combining weight training and cardio into the same routine.
Similarly, among older adults, it has been shown to improve strength, enhance flexibility and may even reduce the risk of falling.
From a rehabilitation perspective, there is some evidence indicating reformer pilates can improve shoulder health and function, reduce lower back pain and increase flexibility.
Finally, there is some evidence suggesting a single session of reformer pilates can improve two key markers of cardiovascular health, being flow-mediated dilation and pulse wave velocity, while also improving cholesterol and insulin levels. This suggests reformer pilates could lead to long-term improvements in heart and metabolic health, although more research is needed to confirm this.
Reformer pilates was first designed to help people recover from injuries. Kampus Productions/Pexels However, there are some key things to consider when discussing these benefits. Most of this research is quite exploratory and comes from a very small number of studies. So we do not know whether these findings will apply to everyone.
Very few studies compared reformer pilates to other types of exercise. Therefore, while it can improve most aspects of health and function, it’s unlikely reformer pilates provides the optimal mode of exercise for each individual component of physical fitness.
Traditional weight training, for example, will likely cause larger improvements in strength than reformer pilates. Similarly, stretching will probably make you more flexible. And running or cycling will make you fitter.
However, if you want a type of exercise that gives you broad overall health benefits, it could be a good option.
What are the downsides of reformer pilates
Reformer pilates is not for everyone.
First and foremost, classes can be expensive compared to other fitness options. You need to be doing at least two to three sessions per week of any type of exercise to maximise the benefits. So even if you can find a class for A$20 or $30, paying for two or three classes a week (or buying a weekly or monthly subscription) is a significant outlay.
Second, it’s not as accessible as other exercise. Even if you can afford it, not every town or suburb has a reformer pilates studio.
Cost and access are major barriers. Or you might get better results with specific modes of exercises. Karolina Grabowska/Pexels Third, the effectiveness of your workout is likely to be impacted by how competent your instructor is. There are a host of different pilates qualifications you can get in Australia, and some take much less time than others. With this in mind, it might be best to look for accredited pilates instructors, although this will further reduce the number of options you have available.
Finally, there is a learning curve. While you will get better over time, the exercise will likely be less effective during those first few weeks (or months) when you are getting used to the machine and the movements.
Is it right for you?
Reformer pilates can be a great addition to your fitness routine, especially if you’re looking for a low-impact way to build strength and flexibility.
But if you have more specific goals, you might need a more specific mode of exercise. For example, if you need to get stronger to improve your ability to manage your daily life, then strength training is probably your best bet. Likewise, if your goal is to run a marathon, you will get more specific benefits from running.
The cost and availability of reformer pilates make it less accessible for some people. With this in mind, if you are after similar benefits at a lower price point, mat pilates might be a better option. Not only does it have evidence suggesting it can improve strength and fitness, but it is something you can do at home if you find a good resource (YouTube could be a good starting point here).
Hunter Bennett, Lecturer in Exercise Science, University of South Australia; Jacinta Brinsley, Exercise Physiologist and Postdoctoral Researcher in the Alliance for Research in Nutrition, Exercise and Activity, University of South Australia, and Lewis Ingram, Lecturer in Physiotherapy, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
How To Stay A Step Ahead Of Peripheral Artery Disease
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Far less well-known than Coronary Artery Disease, it can still result in loss of life and limb (not in that order). Fortunately, there are ways to be on your guard:
What it is
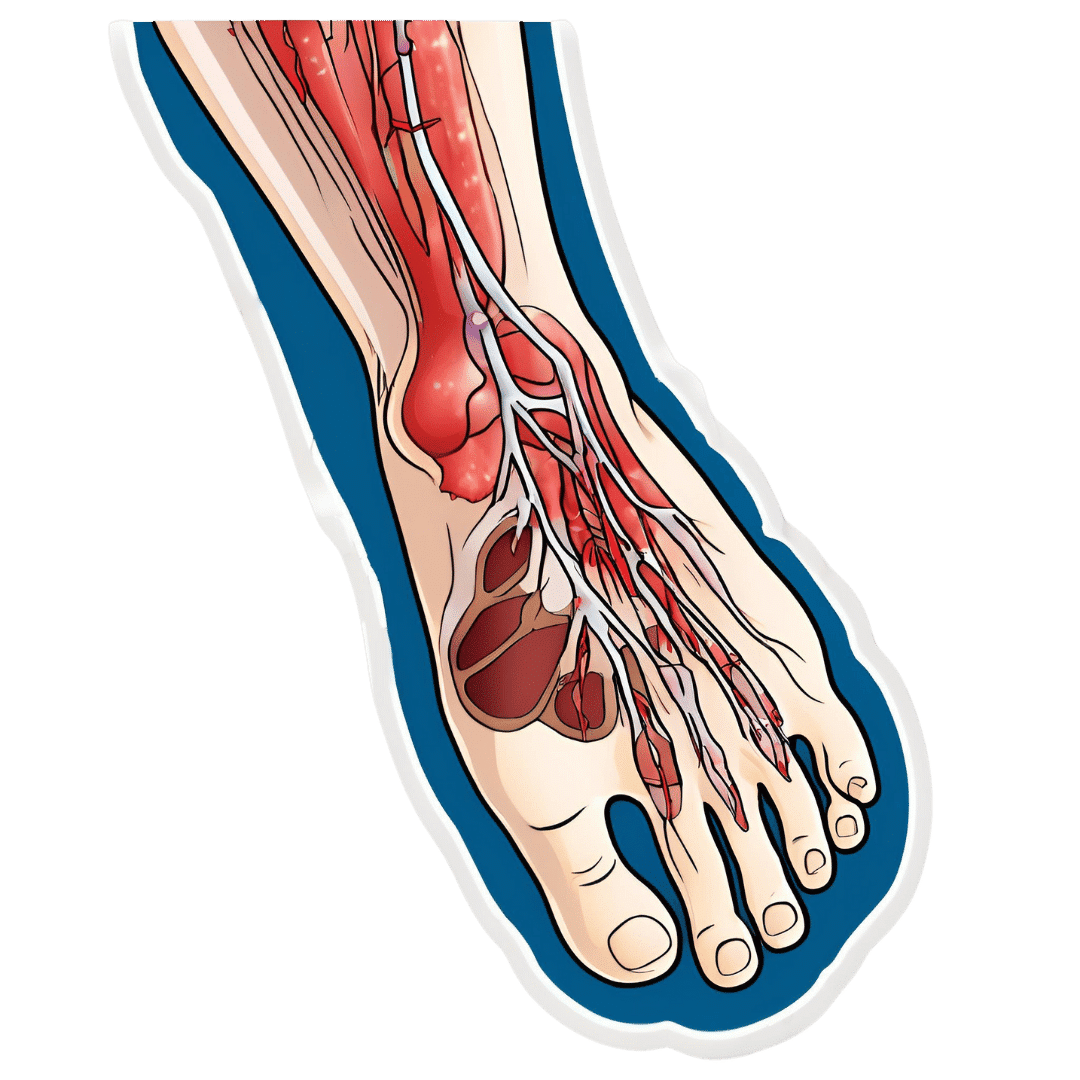
Peripheral Artery Disease (PAD) is the same thing as Coronary Artery Disease (CAD), just, in the periphery—which by definition means “outside of the heart and brain”, but in practice, it starts with the extremities. And of the extremities, it tends to start with the feet and legs, for the simple reason that if someone’s circulation is sluggish, then because of gravity, that’s where’s going to get blocked first.
In both CAD and PAD, the usual root cause is atherosclerosis, that is to say, the build-up of fatty material inside the arteries, usually commensurate to LDL (“bad”) cholesterol, especially in men (high LDL is still a predictor of cardiovascular disease in women though, just more modestly so, at least pre-menopause or in cases of treated menopause whereby HRT has returned hormones to pre-menopause levels).
See also: Demystifying Cholesterol
And for that about sex differences: His & Hers: The Hidden Complexities of Statins and Cardiovascular Disease (CVD)
Why it is
This one’s straightforward, as it’s the same things as any kind of cardiovascular disease: high blood pressure, high cholesterol, older age, obesity, smoking, drinking, diabetes, and genetic factors (so, a risk factor is: family history of heart disease).
However, while those are the main causes and/or risk factors, it absolutely can still strike other people, so it’s as well to be watch out for…
What to look out for
Many people first notice signs and symptoms that turn out to be PAD when they experience pain or numbness in the foot or feet, and/or a discoloration of the feet (especially toes), and slow wound healing.
At that stage, chances are you will need to go urgently to a specialist, and surgery is a likely necessity. With a little luck, it’ll be a minimally-invasive surgery to unblock an artery; failing that, an amputation will be in order.
At that stage, under 50% will be alive 5 years from diagnosis:
You probably want to avoid those. Good news is, you can, by catching it earlier!
What to look out for before that
The most common test for PAD is one you can do at home, but enlisting a nurse to do it for you will help ensure accurate readings. It’s called the Ankle-Brachial Index (ABI) test, and it involves comparing the blood pressure in your ankle with the blood pressure in your arm, and expressing them as a ratio.
Here’s how to do it (instructions and a video demonstration if you want it):
Do Try This At Home: ABI Test For Clogged Arteries
If you need a blood pressure monitor, by the way, here’s an example product on Amazon.
- A healthy ABI score is between 1.0 and 1.4; anything outside this range may indicate arterial problems.
- Low ABI scores (below 0.8) suggest plaque is likely obstructing blood flow
- High ABI scores (above 1.4) may indicate artery hardening
Do note also that yes, if you have plaque obstructing blood flow and hardened arteries, your scores may cancel out and give you a “healthy” score, despite your arteries being very much not healthy.
For this reason, this test can be used to raise the alarm, but not to give the “all clear”.
There are other tests that clinicians can do for you, but you can’t do at home unless you have an MRI machine, a CT scanner, an x-ray machine, a doppler-and-ultrasound machine, etc. We’ll not go into those in detail here, but ask your doctor about them if you’re concerned.
What to do about it
In the mid-to-late stages of the disease, the options are medication and surgery, respectively, but your doctor will advise about those in that eventuality.
In the early stages of the disease, the first-line recommend treatment is exercise, of which, especially walking:
Lower Extremity Peripheral Artery Disease: Diagnosis and Treatment
Given that this more often happens when someone hasn’t been walking so much, it can be a walk-rest-walk approach at first (a treadmill on a low setting can be very useful for this):
See also: Exercise Comparison Head-to-Head: Treadmill vs Road
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Artichoke vs Broccoli – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing artichoke to broccoli, we picked the artichoke.
Why?
Both have their strengths, and it was close! But…
In terms of macros, artichoke has about 2x the fiber (which is lots, because broccoli is already good for this) and more protein, for only slightly more carbs, making it the nutrient dense choice in all respects, and especially in the case of fiber.
In the category of vitamins, artichoke has more of vitamins B3, B9, and choline, while broccoli has more of vitamins A, B2, B5, B6, C, E, and K, thus winning this round.
When it comes to minerals, artichoke has more copper, iron, magnesium, manganese, phosphorus, potassium, and zinc, while broccoli has more calcium and selenium, handing artichoke the win again here.
Looking at polyphenols, both have an abundance; artichoke has more by total mass (in terms of mg/100g) and is especially rich in luteolin and phenolic acids, but broccoli has some that artichoke doesn’t have (such as quercetin and kaempferol). We could reasonably call this a tie or a win for artichoke on strength of numbers; either way, it doesn’t change the end result:
Adding up the sections makes for an overall win for artichoke, but of course, by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
What’s Your Plant Diversity Score?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Make Your Doctor’s Appointment Do More For You
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Doctor: “So, how are you today?”
Patient: “Can’t complain; how about you?”Hopefully your medical appointments don’t start quite like that, but there can be an element of being “along for the ride” when it comes to consultations. They ask questions, we answer, they prescribe something, we thank them.
In principle, the doctor should be able to handle that; ask the right questions, determine the problem, and not need too much from you. After all, they have been trained to deal with an unconscious patient, so the fact you can communicate at all is a bonus.
However, leaving it all to them isn’t really playing the field.
Before the appointment
Research your issue, as best you understand it. Some doctors will be very averse to you telling them about having done this (taking it as an affront to their expertise), but here’s the thing:
You don’t have to tell them.
You just have to understand as much as possible, so that you will be as “up to speed” as possible in the conversation, and not be quickly out of your depth.
Have an agenda, based on the above. Literally, have a little set of bullet-points to remind you what you came in to discuss, so that nothing escapes you in the moment. This should also include:
- If you have additional reasons for a particular concern (e.g. family history of a certain problem), make them known
- If you plan to request any specific tests or treatments, be able to clearly state your reasons for the specific tests or treatments
- If you plan to write off any specific tests or treatments as something to which you will not consent, have your reasons ready—in a way that makes it clear it’s something more than “don’t want it”, for example, “I’ve already decided that this treatment would make a sufficient hit to my quality of life, as to make it not worthwhile for me personally” (or whatever the reason may be for you). It needs to be something they can write on their notes instead of simply “patient refused treatment”.
Compile a record of your symptoms (as appropriate), and any previous tests/treatments (as appropriate), in chronological order. If you take all this with you, perhaps in a nice folder, you will enjoy the following advantages:
- not forgetting anything
- ability to answer questions accurately
- give the (correct) impression you take your health seriously, which means they are more likely to do so also—especially because they will now know that if they fob you off and/or mess something up, you’ll be taking a record of that to your next appointment.
Plan your outfit. No, you don’t have to dress for the red carpet, but you want to satisfy two main conditions:
- Accessibility for examination (for example, if you are going in with a knee pain, maybe don’t wear the tight jeans today; if they’re going to take blood, be either sleeveless or have sleeves that are easily moved out of the way, etc)
- General presentability (it’s a sad fact that doctors are not immune to biases, and will treat people better if they respect them more)
During the appointment
Be friendly; doctors (like most people) will respond much better to that than to grumpiness—even if you have good reason for grumpiness and even if the doctor has been trained to help grumpy patients.
Be confident: when we say “be friendly”, that doesn’t mean to necessarily be so agreeable as to not advocate for yourself. In particular:
- If they explain something and it isn’t clear to you, ask them to clarify
- If you disagree with them about a value judgement, say so. By “a value judgement” here we mean things in the realm of subjectivity. If the doctor says you are prediabetic, then you won’t get much mileage out of arguing otherwise; the numbers have the final say on that one. But if the doctor says “the side effects of the treatment you’re requesting will make it not worthwhile for you” and you have understood the side effects and you still disagree, then your opinion counts for more than theirs—it is your decision to make.
- If they dismiss a concern, ask them to put in writing that they dismissed your concern of X, despite you providing evidence that Y, and it being well-known that Z. Often, rather than doing that, they’ll just fold and actually address your concern instead.
Writer’s example in that last category: I recently made a request for a bone density scan. I expect my bone density is great, because I do all the right things, however, as both of my parents suffered from osteoporosis and assorted resultant crushed bones and the terrible consequences thereof, I a) have reasonable grounds for extra concern, and b) I believe that even if my bone density is fine now, it’s good to establish a baseline so I can know, in 5, 10, 20 years etc, whether there has been any deterioration. Now, happily the doctor I saw agreed with my assessment at first presentation and so I got the referral, but had she not been, I would have said “Could you please put in writing that I asked for a bone density scan, and you refused, on the grounds that [details about what happened with my parents], and that osteoporosis is known to have a strong genetic component is not, in your opinion, any reason to worry?”
Be honest, and/but err on the side of overstating your symptoms rather than understating. For example, if it is about a chronic condition and the doctor asks “are you able to do xyz”, take the question as meaning “are you able to do xyz on your worst days?”. You can clarify that if you like in your answer, but you need to include the information that xyz is something that your condition can and sometimes does impede you from doing.
Leave your embarrassment at the door. To the doctor (unless they are a very unprofessional one), you really are just one more patient with symptoms they have (unless your condition is very rare) seen a thousand times before. If your symptom is embarrassing, it will not faze them and you definitely should not hold back from mentioning it, for example. This goes extra in the case of discussions around sexual health, by the way, in which field the details you’d perhaps rather not share with anybody, are the details they need to adequately treat you.
After the appointment
Follow up on anything that doesn’t happen as promised (e.g. referrals, things ordered, etc), to make sure nothing got lost in a bureacratic error.
Get a second opinion if you’re not satisfied with the first one. Doctors are fallible, and as a matter of professional pride, it’s likely the second doctor will be glad to find something the first doctor missed.
See also: Make Your Negativity Work For You
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: