The Brain Health Book – by Dr. John Randolph
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author, a clinical neuropsychologist and brain health consultant, brings his professional knowledge and understanding to bear on the questions of what works, what doesn’t, and why?
In practical terms, the focus is mostly on maintaining/improving attention, memory, and executive functions. To that end, he covers what kinds of exercises to do (physical and mental!), and examines what strategies make the most difference—including the usual lifestyle considerations of course, but also more specifically than that, what to prioritize over what when it comes to daily choices.
The style is easy pop-science, with an emphasis on being directly useful to the reader, rather than giving an overabundance of citations for everything as we go along. He does, however, explain the necessary science as we go, making the book educational without being academic.
Bottom line: if you’d like to maintain/improve your brain, this book can certainly help with that, and as a bonus (unless you are already an expert) you’ll learn plenty about the brain as you go.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Alzheimer’s Causative Factors To Avoid
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Best Brains Bar Nun?
This is Dr. David Snowdon. He’s an epidemiologist, and one of the world’s foremost experts on Alzheimer’s disease. He was also, most famously, the lead researcher of what has become known as “The Nun Study”.
We recently reviewed his book about this study:
…which we definitely encourage you to check out, but we’ll do our best to summarize its key points today!
Reassurance up-front: no, you don’t have to become a nun
The Nun Study
In 1991, a large number (678) of nuns were recruited for what was to be (and until now, remains) the largest study of its kind into the impact of a wide variety of factors on aging, and in particular, Alzheimer’s disease.
Why it was so important: because the nuns were all from the same Order, had the same occupation (it’s a teaching Order), with very similar lifestyles, schedules, socioeconomic status, general background, access to healthcare, similar diets, same relationship status (celibate), same sex (female), and many other factors also similar, this meant that most of the confounding variables that confound other studies were already controlled-for here.
Enrollment in the study also required consenting to donating one’s brain for study post-mortem—and of those who have since died, indeed 98% of them have been donated (the other 2%, we presume, may have run into technical administrative issues with the donation process, due to the circumstances of death and/or delays in processing the donation).
How the study was undertaken
We don’t have enough space to describe the entire methodology here, but the gist of it is:
- Genetic testing for relevant genetic factors
- Data gathered about lives so far, including not just medical records but also autobiographies that the nuns wrote when they took their vows (at ages 19–21)
- Extensive ongoing personal interviews about habits, life choices, and attitudes
- Yearly evaluations including memory tests and physical function tests
- Brain donation upon death
What they found
Technically, The Nun Study is still ongoing. Of the original 678 nuns (aged 75–106), three are still alive (based on the latest report, at least).
However, lots of results have already been gained, including…
Genes
A year into the study, in 1992, the “apolipoprotein E” (APOE) gene was established as a likely causative factor in Alzheimer’s disease. This is probably not new to our readers in 2024, but there are interesting things being learned even now, for example:
The Alzheimer’s Gene That Varies By Race & Sex
…but watch out! Because also:
Alzheimer’s Sex Differences May Not Be What They Appear
Words
Based on the autobiographies written by the nuns in their youth upon taking their vows, there were two factors that were later correlated with not getting dementia:
- Longer sentences
- Positive outlook
- “Idea density”
That latter item means the relative linguistic density of ideas and complexity thereof, and the fluency and vivacity with which they were expressed (this was not a wishy-washy assessment; there was a hard-science analysis to determine numbers).
Want to spruce up yours? You might like to check out:
Reading, Better: Reading As A Cognitive Exercise
…for specific, evidence-based ways to tweak your reading to fight cognitive decline.
Food
While the dietary habits of the nuns were fairly homogenous, those who favored eating more and cooked greens, beans, and tomatoes, lived longer and with healthier brains.
See also: Brain Food? The Eyes Have It!
Other aspects of brain health & mental health
The study also found that nuns who avoided stroke and depression, were also less likely to get dementia.
For tending to these, check out:
- Two Things You Can Do To Improve Stroke Survival Chances
- Depression, And The Mental Health First-Aid That You’ll Hopefully Never Need
- Behavioral Activation Against Depression & Anxiety
Community & Faith
Obviously, in this matter the nuns were quite a homogenous group, scoring heavily in community and faith. What’s relevant here is the difference between the nuns, and other epidemiological studies in other groups (invariably not scoring so highly).
Community & faith are considered, separately and together, to be protective factors against dementia.
Faith may be something that “you have it or you don’t” (we’re a health science newsletter, not a theological publication, but for the interested, philosopher John Stuart Mill’s 1859 essay “On Liberty“ makes a good argument for it not being something one can choose, prompting him to argue for religious tolerance, on the grounds that religious coercion is a futile effort precisely because a person cannot choose to dis/believe something)
…but community can definitely be chosen, nurtured, and grown. We’ve written about this a bit before:
You might also like to check out this great book on the topic:
Purpose: Design A Community And Change Your Life – by Gina Bianchini
Want more?
We gave a ground-up primer on avoiding Alzheimer’s and other dementias; check it out:
How To Reduce Your Alzheimer’s Risk
Take care!
Share This Post
-
“The Longevity Vitamin” (That’s Not A Vitamin)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Magic of Mushrooms
“The Longevity Vitamin that’s not a vitamin” is a great tagline for what’s actually an antioxidant amino acid nutraceutical, but in this case, we’re not the ones spearheading its PR, but rather, the Journal of Nutritional Science:
Is ergothioneine a “longevity vitamin” limited in the American diet?
It can be found in all foods, to some extent, but usually in much tinier amounts than would be useful. The reason for this is that it’s synthesized by a variety of microbes (mostly fungi and actinobacteria), and enters the food chain via vegetables that are grown in soil that contain such (which is basically all soil, unless you were to go out of your way to sterilize it, or something really unusually happened).
About those fungi? That includes common popular edible fungi, where it is found quite generously. An 85g (3oz) portion of (most) mushrooms contains about 5mg of ergothioneine, the consumption of which is associated with a 16% reduced all-cause mortality:
However… Most Americans don’t eat that many mushrooms, and those polled averaged 1.1mg/day ergothioneine (in contrast with, for example, Italians’ 4.6mg/day average).
Antioxidant properties
While its antioxidant properties aren’t the most exciting quality, they are worth a mention, on account of their potency:
The biology of ergothioneine, an antioxidant nutraceutical
This is also part of its potential bid to get classified as a vitamin, because…
❝Decreased blood and/or plasma levels of ergothioneine have been observed in some diseases, suggesting that a deficiency could be relevant to the disease onset or progression❞
Source: Ergothioneine: a diet-derived antioxidant with therapeutic potential
Healthy aging
Building on from the above, ergothioneine has been specifically identified as being associated with healthy aging and the prevention of cardiometabolic diseases:
❝An increasing body of evidence suggests ergothioneine may be an important dietary nutrient for the prevention of a variety of inflammatory and cardiometabolic diseases and ergothioneine has alternately been suggested as a vitamin, “longevity vitamin”, and nutraceutical❞
~ Dr. Bernadette Moore et al., citing more references every few words there
Source: Ergothioneine: an underrecognised dietary micronutrient required for healthy ageing?
Good for the heart = good for the brain
As a general rule of thumb, “what’s good for the heart is good for the brain” is almost always true, and it appears to be so in this case, too:
❝Ergothioneine crosses the blood–brain barrier and has been reported to have beneficial effects in the brain. In this study, we discuss the cytoprotective and neuroprotective properties of ergotheioneine, which may be harnessed for combating neurodegeneration and decline during aging.❞
Source: Ergothioneine: A Stress Vitamin with Antiaging, Vascular, and Neuroprotective Roles?
Want to get some?
You can just eat a portion of mushrooms per day! But if you don’t fancy that, it is available as a supplement in convenient 1/day capsule form too.
We don’t sell it, but for your convenience, here is an example product on Amazon
Enjoy!
Share This Post
-
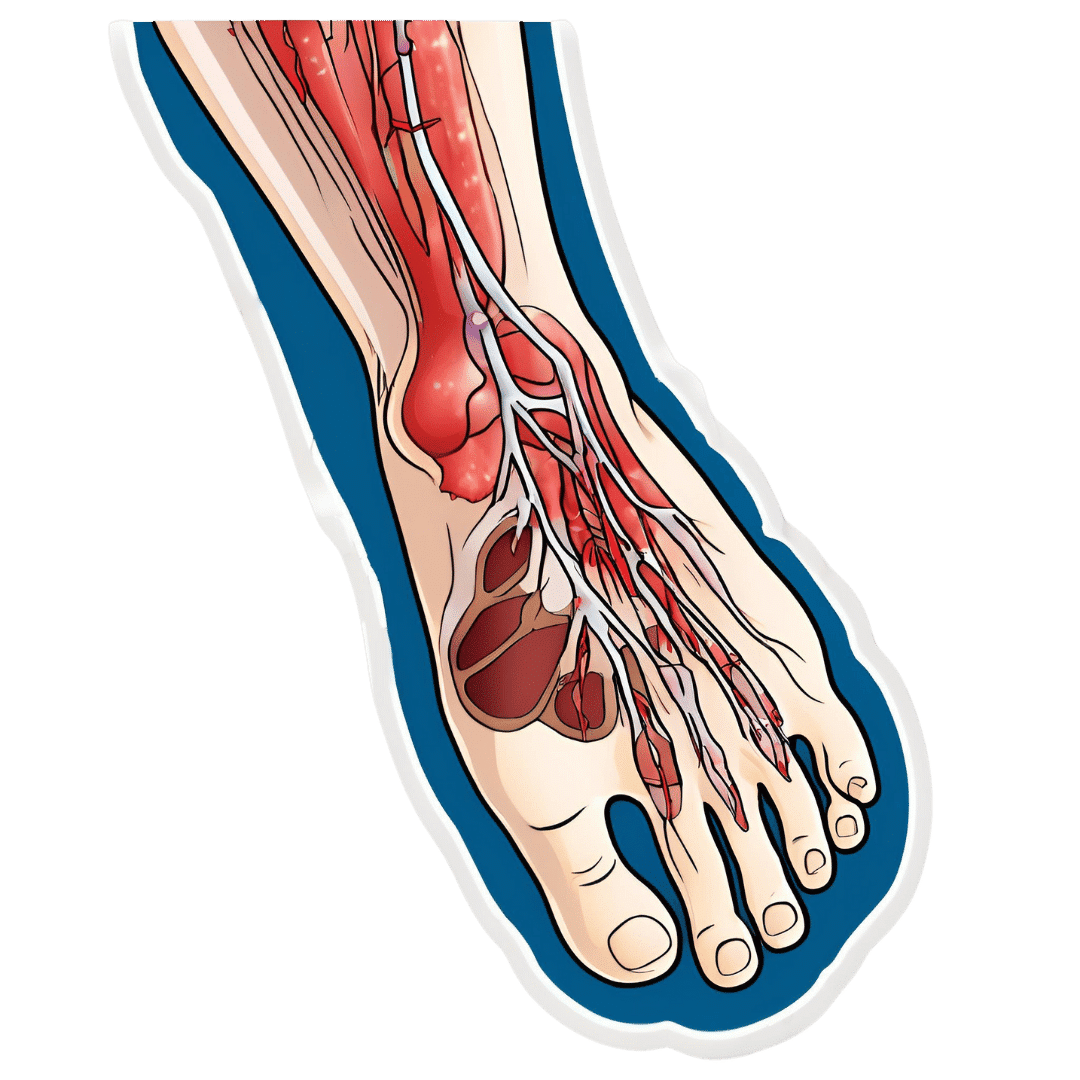
How To Stay A Step Ahead Of Peripheral Artery Disease
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Far less well-known than Coronary Artery Disease, it can still result in loss of life and limb (not in that order). Fortunately, there are ways to be on your guard:
What it is
Peripheral Artery Disease (PAD) is the same thing as Coronary Artery Disease (CAD), just, in the periphery—which by definition means “outside of the heart and brain”, but in practice, it starts with the extremities. And of the extremities, it tends to start with the feet and legs, for the simple reason that if someone’s circulation is sluggish, then because of gravity, that’s where’s going to get blocked first.
In both CAD and PAD, the usual root cause is atherosclerosis, that is to say, the build-up of fatty material inside the arteries, usually commensurate to LDL (“bad”) cholesterol, especially in men (high LDL is still a predictor of cardiovascular disease in women though, just more modestly so, at least pre-menopause or in cases of treated menopause whereby HRT has returned hormones to pre-menopause levels).
See also: Demystifying Cholesterol
And for that about sex differences: His & Hers: The Hidden Complexities of Statins and Cardiovascular Disease (CVD)
Why it is
This one’s straightforward, as it’s the same things as any kind of cardiovascular disease: high blood pressure, high cholesterol, older age, obesity, smoking, drinking, diabetes, and genetic factors (so, a risk factor is: family history of heart disease).
However, while those are the main causes and/or risk factors, it absolutely can still strike other people, so it’s as well to be watch out for…
What to look out for
Many people first notice signs and symptoms that turn out to be PAD when they experience pain or numbness in the foot or feet, and/or a discoloration of the feet (especially toes), and slow wound healing.
At that stage, chances are you will need to go urgently to a specialist, and surgery is a likely necessity. With a little luck, it’ll be a minimally-invasive surgery to unblock an artery; failing that, an amputation will be in order.
At that stage, under 50% will be alive 5 years from diagnosis:
You probably want to avoid those. Good news is, you can, by catching it earlier!
What to look out for before that
The most common test for PAD is one you can do at home, but enlisting a nurse to do it for you will help ensure accurate readings. It’s called the Ankle-Brachial Index (ABI) test, and it involves comparing the blood pressure in your ankle with the blood pressure in your arm, and expressing them as a ratio.
Here’s how to do it (instructions and a video demonstration if you want it):
Do Try This At Home: ABI Test For Clogged Arteries
If you need a blood pressure monitor, by the way, here’s an example product on Amazon.
- A healthy ABI score is between 1.0 and 1.4; anything outside this range may indicate arterial problems.
- Low ABI scores (below 0.8) suggest plaque is likely obstructing blood flow
- High ABI scores (above 1.4) may indicate artery hardening
Do note also that yes, if you have plaque obstructing blood flow and hardened arteries, your scores may cancel out and give you a “healthy” score, despite your arteries being very much not healthy.
For this reason, this test can be used to raise the alarm, but not to give the “all clear”.
There are other tests that clinicians can do for you, but you can’t do at home unless you have an MRI machine, a CT scanner, an x-ray machine, a doppler-and-ultrasound machine, etc. We’ll not go into those in detail here, but ask your doctor about them if you’re concerned.
What to do about it
In the mid-to-late stages of the disease, the options are medication and surgery, respectively, but your doctor will advise about those in that eventuality.
In the early stages of the disease, the first-line recommend treatment is exercise, of which, especially walking:
Lower Extremity Peripheral Artery Disease: Diagnosis and Treatment
Given that this more often happens when someone hasn’t been walking so much, it can be a walk-rest-walk approach at first (a treadmill on a low setting can be very useful for this):
See also: Exercise Comparison Head-to-Head: Treadmill vs Road
Take care!
Share This Post
Related Posts
-
Woman Petitions Health Insurer After Company Approves — Then Rejects — Her Infusions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When KFF Health News published an article in August about the “prior authorization hell” Sally Nix said she went through to secure approval from her insurance company for the expensive monthly infusions she needs, we thought her story had a happy ending.
That’s because, after KFF Health News sent questions to Nix’s insurance company, Blue Cross Blue Shield of Illinois, it retroactively approved $36,000 worth of treatments she thought she owed. Even better, she also learned she would qualify for the infusions moving forward.
Good news all around — except it didn’t last for long. After all, this is the U.S. health care system, where even patients with good insurance aren’t guaranteed affordable care.
To recap: For more than a decade, Nix, of Statesville, North Carolina, has suffered from autoimmune diseases, chronic pain, and fatigue, as well as a condition called trigeminal neuralgia, which is marked by bouts of electric shock-like pain that’s so intense it’s commonly known as the “suicide disease.”
“It is a pain that sends me to my knees,” Nix said in October. “My entire family’s life is controlled by the betrayal of my body. We haven’t lived normally in 10 years.”
Late in 2022, Nix started receiving intravenous immunoglobulin infusions to treat her diseases. She started walking two miles a day with her service dog. She could picture herself celebrating, free from pain, at her daughter’s summer 2024 wedding.
“I was so hopeful,” she said.
But a few months after starting those infusions, she found out that her insurance company wouldn’t cover their cost anymore. That’s when she started “raising Cain about it” on Instagram and Facebook.
You probably know someone like Sally Nix — someone with a chronic or life-threatening illness whose doctor says they need a drug, procedure, or scan, and whose insurance company has replied: No.
Prior authorization was conceived decades ago to rein in health care costs by eliminating duplicative and ineffective treatment. Not only does overtreatment waste billions of dollars every year, but doctors acknowledge it also potentially harms patients.
However, critics worry that prior authorization has now become a way for health insurance companies to save money, sometimes at the expense of patients’ lives. KFF Health News has heard from hundreds of people in the past year relating their prior authorization horror stories.
When we first met Nix, she was battling her insurance company to regain authorization for her infusions. She’d been forced to pause her treatments, unable to afford $13,000 out-of-pocket for each infusion.
Finally, it seemed like months of her hard work had paid off. In July, Nix was told by staff at both her doctor’s office and her hospital that Blue Cross Blue Shield of Illinois would allow her to restart treatment. Her balance was marked “paid” and disappeared from the insurer’s online portal.
But the day after the KFF Health News story was published, Nix said, she learned the message had changed. After restarting treatment, she received a letter from the insurer saying her diagnoses didn’t actually qualify her for the infusions. It felt like health insurance whiplash.
“They’re robbing me of my life,” she said. “They’re robbing me of so much, all because of profit.”
Dave Van de Walle, a spokesperson for Blue Cross Blue Shield of Illinois, said the company would not discuss individual patients’ cases.
“Prior authorization is often a requirement for certain treatments,” Van de Walle said in a written statement, “and BCBSIL administers benefits according to medical policy and the employer’s benefit.”
But Nix is a Southern woman of the “Steel Magnolia” variety. In other words, she’s not going down without a fight.
In September, she called out her insurance company’s tactics in a http://change.org/ campaign that has garnered more than 21,000 signatures. She has also filed complaints against her insurance company with the U.S. Department of Health and Human Services, U.S. Department of Labor, Illinois Department of Insurance, and Illinois attorney general.
Even so, Nix said, she feels defeated.
Not only is she still waiting for prior authorization to restart her immunoglobulin infusions, but her insurance company recently required Nix to secure preapproval for another treatment — routine numbing injections she has received for nearly 10 years to treat the nerve pain caused by trigeminal neuralgia.
“It is reprehensible what they’re doing. But they’re not only doing it to me,” said Nix, who is now reluctantly taking prescription opioids to ease her pain. “They’re doing it to other patients. And it’s got to stop.”
Do you have an experience with prior authorization you’d like to share? Click here to tell your story.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
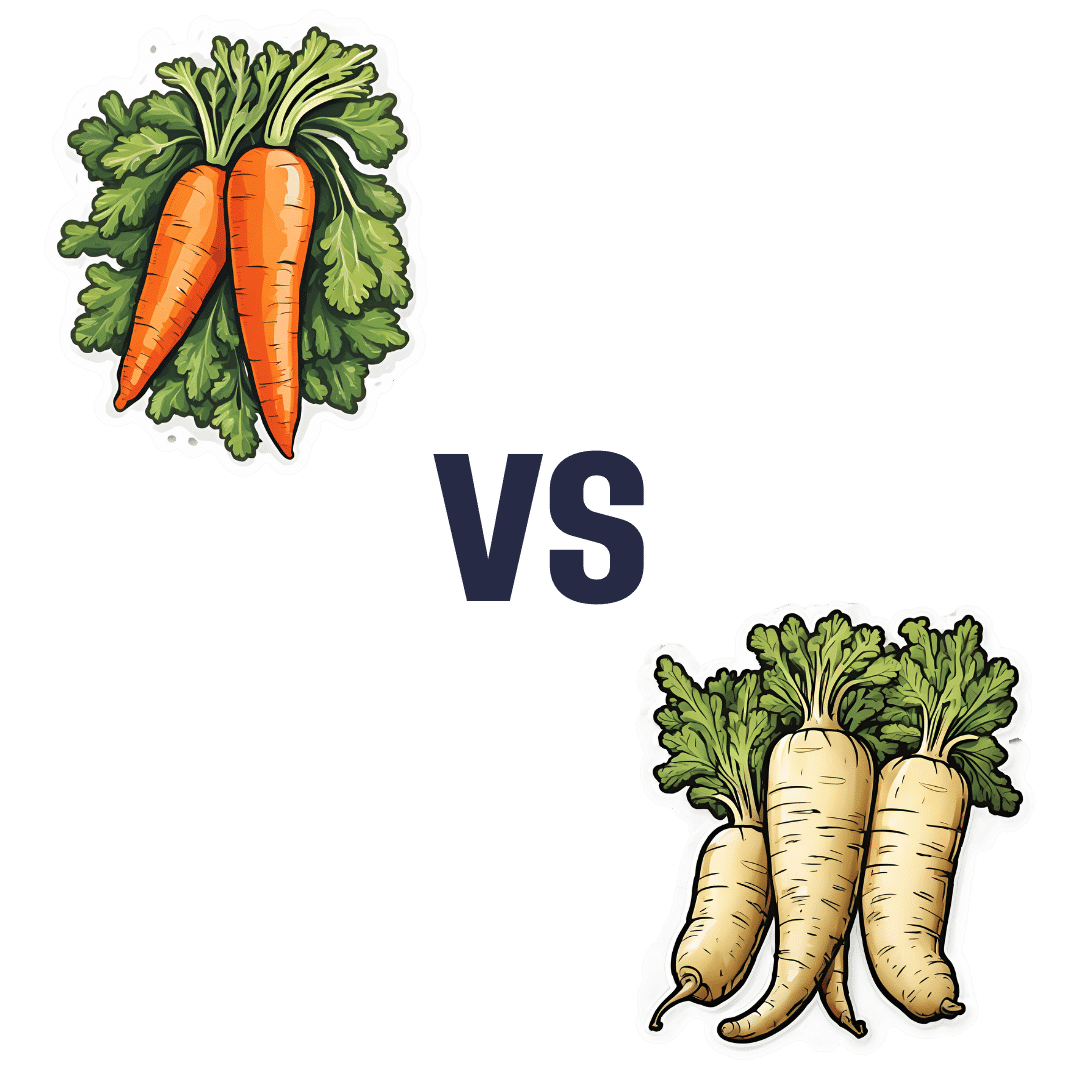
Carrots vs Parsnips – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing carrots to parsnips, we picked the parsnips.
Why?
There are arguments for both! But we say parsnips win on overall nutritional density.
In terms of macros, parsnips vary quite a lot from region to another, but broadly speaking, parsnips have more carbs and fiber, and/but the ratios are such that carrots have the lower glycemic index. We’ll call this one a win for carrots.
When it comes to vitamins, carrots have more of vitamins A, B2, B3, B6, and choline, while parsnips have more of vitamins B1, B5, B9, C, E, and K. A small win for parsnips here.
In the category of minerals, carrots are not higher in any minerals, while parsnips are higher in calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. An overwhelming win for parsnips.
While the overall vitamin and mineral content puts parsnips ahead, it’s still worth noting that carrots have highly bioavailable megadoses of vitamin A.
Another thing to note is that the glycemic index recorded for both is when peeled and boiled, whereas both of these root vegetables can be enjoyed raw if you wish, which has a much lower GI.
In short, enjoy either or both, but parsnips are the more nutritionally dense overall.
Want to learn more?
You might like to read:
Glycemic Index vs Glycemic Load vs Insulin Index
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Forget Ringing the Button for the Nurse. Patients Now Stay Connected by Wearing One.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
HOUSTON — Patients admitted to Houston Methodist Hospital get a monitoring device about the size of a half-dollar affixed to their chest — and an unwitting role in the expanding use of artificial intelligence in health care.
The slender, battery-powered gadget, called a BioButton, records vital signs including heart and breathing rates, then wirelessly sends the readings to nurses sitting in a 24-hour control room elsewhere in the hospital or in their homes. The device’s software uses AI to analyze the voluminous data and detect signs a patient’s condition is deteriorating.
Hospital officials say the BioButton has improved care and reduced the workload of bedside nurses since its rollout last year.
“Because we catch things earlier, patients are doing better, as we don’t have to wait for the bedside team to notice if something is going wrong,” said Sarah Pletcher, system vice president at Houston Methodist.
But some nurses fear the technology could wind up replacing them rather than supporting them — and harming patients. Houston Methodist, one of dozens of U.S. hospitals to employ the device, is the first to use the BioButton to monitor all patients except those in intensive care, Pletcher said.
“The hype around a lot of these devices is they provide care at scale for less labor costs,” said Michelle Mahon, a registered nurse and an assistant director of National Nurses United, the profession’s largest U.S. union. “This is a trend that we find disturbing,” she said.
The rollout of BioButton is among the latest examples of hospitals deploying technology to improve efficiency and address a decades-old nursing shortage. But that transition has raised its own concerns, including about the device’s use of AI; polls show the public is wary of health providers relying on it for patient care.
In December 2022 the FDA cleared the BioButton for use in adult patients who are not in critical care. It is one of many AI tools now used by hospitals for tasks like reading diagnostic imaging results.
In 2023, President Joe Biden directed the Department of Health and Human Services to develop a plan to regulate AI in hospitals, including by collecting reports of patients harmed by its use.
The leader of BioIntelliSense, which developed the BioButton, said its device is a huge advance compared with nurses walking into a room every few hours to measure vital signs. “With AI, you now move from ‘I wonder why this patient crashed’ to ‘I can see this crash coming before it happens and intervene appropriately,’” said James Mault, CEO of the Golden, Colorado-based company.
The BioButton stays on the skin with an adhesive, is waterproof, and has up to a 30-day battery life. The company says the device — which allows providers to quickly notice deteriorating health by recording more than 1,000 measurements a day per patient — has been used on more than 80,000 hospital patients nationwide in the past year.
Hospitals pay BioIntelliSense an annual subscription fee for the devices and software.
Houston Methodist officials would not reveal how much the hospital pays for the technology, though Pletcher said it equates to less than a cup of coffee a day per patient.
For a hospital system that treats thousands of patients at a time — Houston Methodist has 2,653 non-ICU beds at its eight Houston-area hospitals — such an investment could still translate to millions of dollars a year.
Hospital officials say they have not made any changes in nurse staffing and have no plans to because of implementing the BioButton.
Inside the hospital’s control center for virtual monitoring on a recent morning, about 15 nurses and technicians dressed in scrubs sat in front of large monitors showing the health status of hundreds of patients they were assigned to monitor.
A red checkmark next to a patient’s name signaled the AI software had found readings trending outside normal. Staff members could click into a patient’s medical record, showing patients’ vital signs over time and other medical history. These virtual nurses, if you will, could contact nurses on the floor by phone or email, or even dial directly into the patient’s room via video call.
Nutanben Gandhi, a technician who was watching 446 patients on her monitor that morning, said that when she gets an alert, she looks at the patient’s health record to see if the anomaly can be easily explained by something in the patient’s condition or if she needs to contact nurses on the patient’s floor.
Oftentimes an alert can be easily dismissed. But identifying signs of deteriorating health can be tough, said Steve Klahn, Houston Methodist’s clinical director of virtual medicine.
“We are looking for a needle in a haystack,” he said.
Donald Eustes, 65, was admitted to Houston Methodist in March for prostate cancer treatment and has since been treated for a stroke. He is happy to wear the BioButton.
“You never know what can happen here, and having an extra set of eyes looking at you is a good thing,” he said from his hospital bed. After being told the device uses AI, the Montgomery, Texas, man said he has no problem with its helping his clinical team. “This sounds like a good use of artificial intelligence.”
Patients and nurses alike benefit from remote monitoring like the BioButton, said Pletcher of Houston Methodist.
The hospital has placed small cameras and microphones inside all patient rooms enabling nurses outside to communicate with patients and perform tasks such as helping with patient admissions and discharge instructions. Patients can include family members on the remote calls with nurses or a doctor, she said.
Virtual technology frees up on-duty nurses to provide more hands-on help, such as starting an intravenous line, Pletcher said. With the BioButton, nurses can wait to take routine vital signs every eight hours instead of every four, she said.
Pletcher said the device reduces nurses’ stress in monitoring patients and allows some to work more flexible hours because virtual care can be done from home rather than coming to the hospital. Ultimately it helps retain nurses, not drive them away, she said.
Sheeba Roy, a nurse manager at Houston Methodist, said some members of the nursing staff were nervous about relying on the device and not checking patients’ vital signs as often themselves. But testing has shown the device provides accurate information.
“After we implemented it, the staff loves it,” Roy said.
Serena Bumpus, chief executive officer of the Texas Nurses Association, said her concern with any technology is that it can be more burdensome on nurses and take away time with patients.
“We have to be hypervigilant in ensuring that we are not leaning on this to replace the ability of nurses to critically think and assess patients and validate what this device is telling us is true,” Bumpus said.
Houston Methodist this year plans to send the BioButton home with patients so the hospital can better track their progress in the weeks after discharge, measuring the quality of their sleep and checking their gait.
“We are not going to need less nurses in health care, but we have limited resources and we have to use those as thoughtfully as we can,” Pletcher said. “Looking at projected demand and seeing the supply we have coming, we will not have enough to meet demand, so anything we can do to give time back to nurses is a good thing.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: