Neurologists Debunk 11 Brain Myths
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Neuroscientists Dr. Santoshi Billakota and Dr. Brad Kamitaki debunk 11 myths about the brain. How many did you know?
From the top
Without further ado, the myths are…
- “We only use 10% of our brains”: False! We use most parts of our brain at different times, depending on the activity. PET/MRI scans show widespread usage.
- “The bigger the brain, the smarter the creature”: False! While there’s often a correlation, intelligence depends on brain complexity and development of specific regions, not overall size. For this reason get, for example, some corvids that are more intelligent than some dogs.
- “IQ tests are an accurate measure of intelligence”: False! IQ tests measure limited aspects of intelligence and are influenced by external factors like test conditions and education.
- “Video games rot your brain”: False! Video games can improve problem-solving, strategy, and team-building skills when played in moderation.
- “Memory gets worse as you age”: Partly false. While episodic memory may decline, semantic and procedural memory often improve with age.
- “Left-brained people are logical, and right-brained people are creative”: False! Both hemispheres work together, and personality or skills are influenced by environment and experiences, not brain hemispheres.
- “You can’t prevent a stroke”: False! Strokes can often be prevented by managing risk factors like blood pressure, cholesterol, and lifestyle choices.
- “Eating fish makes you smarter”: False! Eating fish, especially those rich in omega-3s, can support brain health but won’t increase intelligence.
- “You can always trust your senses”: False! Senses can be deceptive and influenced by emotions, memories, or neurological conditions.
- “Different sexes have different brains”: False! Structurally, brains are the same regardless of chromosomal sex; differences arise from environmental (including hormonal) and experiential factors—and even there, there’s more than enough overlap that we are far from categorizable as sexually dimorphic.
- “If you have a seizure, you have epilepsy”: False! A seizure can occur from various causes, but epilepsy is defined by recurrent unprovoked seizures and requires specific diagnosis and treatment.
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
The Dopamine Myth ← a bonus 12th myth!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Grapefruit vs Lemon – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing grapefruit to lemon, we picked the lemon.
Why?
Grapefruit has its merits, but in the battle of the citrus fruits, lemons come out on top nutritionally:
In terms of macros, grapefruit has more carbs while lemons have more fiber. So, while both have a low glycemic index, lemon is still the winner by the numbers.
Looking at the vitamins, here we say grapefruit’s strengths: grapefruit has more of vitamins A, B2, B3, and choline, while lemon has more of vitamins B6 and C. So, a 4:2 win for grapefruit here.
In the category of minerals, lemons retake the lead: grapefruit has more zinc, while lemon has more calcium, copper, iron, manganese, and selenium.
One final consideration that’s not shown in the nutritional values, is that grapefruit contains high levels of furanocoumarin, which can inhibit cytochrome P-450 3A4 isoenzyme and P-glycoptrotein transporters in the intestine and liver—slowing down their drug metabolism capabilities, thus effectively increasing the bioavailability of many drugs manifold.
This may sound superficially like a good thing (improving bioavailability of things we want), but in practice it means that in the case of many drugs, if you take them with (or near in time to) grapefruit or grapefruit juice, then congratulations, you just took an overdose. This happens with a lot of meds for blood pressure, cholesterol (including statins), calcium channel-blockers, anti-depressants, benzo-family drugs, beta-blockers, and more. Oh, and Viagra, too. Which latter might sound funny, but remember, Viagra’s mechanism of action is blood pressure modulation, and that is not something you want to mess around with unduly. So, do check with your pharmacist to know if you’re on any meds that would be affected by grapefruit or grapefruit juice!
PS: the same substance is quite available in pummelos and sour oranges (but not meaningfully in sweet oranges); you can see a chart here showing the relative furanocoumarin contents of many citrus fruits, or lack thereof as the case may be, as it is for lemons and most limes)
Adding up the sections gives us a clear win for lemons, but by all means enjoy either or both; just watch out for that furanocoumarin content of grapefruit if you’re on any meds affected by such (again, do check with your pharmacist, as our list was far from exhaustive—and yes, this question is one that a pharmacist will answer more easily and accurately than a doctor will).
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer ← citrus fruits in general make the list; they inhibit tumor growth and kill cancer cells; regular consumption is also associated with a lower cancer risk 🙂
Enjoy!
Share This Post
-
This salt alternative could help reduce blood pressure. So why are so few people using it?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One in three Australian adults has high blood pressure (hypertension). Excess salt (sodium) increases the risk of high blood pressure so everyone with hypertension is advised to reduce salt in their diet.
But despite decades of strong recommendations we have failed to get Australians to cut their intake. It’s hard for people to change the way they cook, season their food differently, pick low-salt foods off the supermarket shelves and accept a less salty taste.
Now there is a simple and effective solution: potassium-enriched salt. It can be used just like regular salt and most people don’t notice any important difference in taste.
Switching to potassium-enriched salt is feasible in a way that cutting salt intake is not. Our new research concludes clinical guidelines for hypertension should give patients clear recommendations to switch.
What is potassium-enriched salt?
Potassium-enriched salts replace some of the sodium chloride that makes up regular salt with potassium chloride. They’re also called low-sodium salt, potassium salt, heart salt, mineral salt, or sodium-reduced salt.
Potassium chloride looks the same as sodium chloride and tastes very similar.
Potassium-enriched salt works to lower blood pressure not only because it reduces sodium intake but also because it increases potassium intake. Insufficient potassium, which mostly comes from fruit and vegetables, is another big cause of high blood pressure.
What is the evidence?
We have strong evidence from a randomised trial of 20,995 people that switching to potassium-enriched salt lowers blood pressure and reduces the risks of stroke, heart attacks and early death. The participants had a history of stroke or were 60 years of age or older and had high blood pressure.
An overview of 21 other studies suggests much of the world’s population could benefit from potassium-enriched salt.
The World Health Organisation’s 2023 global report on hypertension highlighted potassium-enriched salt as an “affordable strategy” to reduce blood pressure and prevent cardiovascular events such as strokes.
What should clinical guidelines say?
We teamed up with researchers from the United States, Australia, Japan, South Africa and India to review 32 clinical guidelines for managing high blood pressure across the world. Our findings are published today in the American Heart Association’s journal, Hypertension.
We found current guidelines don’t give clear and consistent advice on using potassium-enriched salt.
While many guidelines recommend increasing dietary potassium intake, and all refer to reducing sodium intake, only two guidelines – the Chinese and European – recommend using potassium-enriched salt.
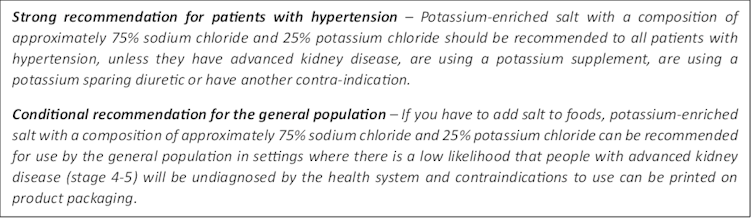
To help guidelines reflect the latest evidence, we suggested specific wording which could be adopted in Australia and around the world:
Recommended wording for guidance about the use of potassium-enriched salt in clinical management guidelines. Why do so few people use it?
Most people are unaware of how much salt they eat or the health issues it can cause. Few people know a simple switch to potassium-enriched salt can help lower blood pressure and reduce the risk of a stroke and heart disease.
Limited availability is another challenge. Several Australian retailers stock potassium-enriched salt but there is usually only one brand available, and it is often on the bottom shelf or in a special food aisle.
Potassium-enriched salts also cost more than regular salt, though it’s still low cost compared to most other foods, and not as expensive as many fancy salts now available.
It looks and tastes like normal salt.
Jimmy Dean/UnsplashA 2021 review found potassium-enriched salts were marketed in only 47 countries and those were mostly high-income countries. Prices ranged from the same as regular salt to almost 15 times greater.
Even though generally more expensive, potassium-enriched salt has the potential to be highly cost effective for disease prevention.
Preventing harm
A frequently raised concern about using potassium-enriched salt is the risk of high blood potassium levels (hyperkalemia) in the approximately 2% of the population with serious kidney disease.
People with serious kidney disease are already advised to avoid regular salt and to avoid foods high in potassium.
No harm from potassium-enriched salt has been recorded in any trial done to date, but all studies were done in a clinical setting with specific guidance for people with kidney disease.
Our current priority is to get people being managed for hypertension to use potassium-enriched salt because health-care providers can advise against its use in people at risk of hyperkalemia.
In some countries, potassium-enriched salt is recommended to the entire community because the potential benefits are so large. A modelling study showed almost half a million strokes and heart attacks would be averted every year in China if the population switched to potassium-enriched salt.
What will happen next?
In 2022, the health minister launched the National Hypertension Taskforce, which aims to improve blood pressure control rates from 32% to 70% by 2030 in Australia.
Potassium-enriched salt can play a key role in achieving this. We are working with the taskforce to update Australian hypertension management guidelines, and to promote the new guidelines to health professionals.
In parallel, we need potassium-enriched salt to be more accessible. We are engaging stakeholders to increase the availability of these products nationwide.
The world has already changed its salt supply once: from regular salt to iodised salt. Iodisation efforts began in the 1920s and took the best part of 100 years to achieve traction. Salt iodisation is a key public health achievement of the last century preventing goitre (a condition where your thyroid gland grows larger) and enhancing educational outcomes for millions of the poorest children in the world, as iodine is essential for normal growth and brain development.
The next switch to iodised and potassium-enriched salt offers at least the same potential for global health gains. But we need to make it happen in a fraction of the time.
Xiaoyue Xu (Luna), Scientia Lecturer, UNSW Sydney; Alta Schutte, SHARP Professor of Cardiovascular Medicine, UNSW Sydney, and Bruce Neal, Executive Director, George Institute Australia, George Institute for Global Health
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Build Strong Feet: Exercises To Strengthen Your Foot & Ankle
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot depends on the health of our feet, especially when it comes to their strength and stability. But they often get quite neglected, when it comes to maintenance. Here’s how to help your feet keep the rest of your body in good condition:
On a good footing
The foot-specific exercises recommended here include:
- Active toe flexion/extension: curl and extend your toes
- Active toe adduction/abduction: use a towel for feedback this time as you spread your toes
- “Short foot” exercise: create an arch by bringing the base of your big toe towards your heel
- Resisted big toe flexion: use resistance bands; flex your big toe while controlling the others.
- Standing big toe flexion (isometric): press your big toe against an inclined surface as forcefully as you can
- Foot bridge exercise: hold your position with the front part of your feet on an elevated surface, to strengthen the arch.
- Heel raises: which can be progressed from basic to more advanced variations, increasing difficulty
- Ankle movements: dorsiflexion, inversion, etc, to increase mobility
It’s important to also look after your general lower body strength and stability, including (for example) single-leg deadlifts, step-downs, and lunges
Balance and proprioceptive exercises are good too, such as a static or dynamic one-leg balances, progressing to doing them with your eyes closed and/or on unstable surfaces (be careful, of course, and progress to this only when confident).
For more on all of these, an explanation of the anatomy, some other exercises too, and visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Steps For Keeping Your Feet A Healthy Foundation
Take care!
Share This Post
Related Posts
-
How to keep your teeth young
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How to keep your teeth young
The association between aging and teeth is so well-established that it’s entered popular idiom, “too long in the tooth”, and when it comes to visual representations, false teeth are well-associated with old age.
And yet, avoiding such outcomes does not get anywhere near so much attention as, say, avoiding wrinkles or hair loss.
At 10almonds, we’ve covered general dental health before, in a three-part series:
- Toothpastes & Mouthwashes: Which Help And Which Harm?
- Flossing, Better (And Easier!)
- Less Common Oral Hygiene Options
Today, we’re going to be looking specifically at keeping our teeth young. What if you have lost your teeth already? Well, gum health remains important, and it’s foundational for everyone, so…
Look after your gums first and last
Hollywood’s most “perfect” whites would be nothing without the gums holding them in place. So, set aside the cosmetic whitening products that often harm gums (anything containing bleach / hydrogen peroxide, is generally a bad idea), andinstead focus on your gums.
As for avoiding gum disease (periodontitis)?
❝In conclusion, periodontitis might enhance the association of biological aging with all-cause mortality in middle-aged and older adults.
Hence, maintaining and enhancing periodontal health is expected to become an intervention to slow aging and extend life span.❞
Source: Does Periodontitis Affect the Association of Biological Aging with Mortality?
Ways to look after gum health include the obvious “floss” and “brush often” and “use fluoride toothpaste”, along with other options we covered in our “Less Common Oral Hygiene Options” article above.
Also important: don’t smoke. It is bad for everything, and this is no exception.
We expect we probably don’t have many subscribers who smoke, but if you do, please consider making quitting a priority.
See also: Smoking, Gum Disease, and Tooth Loss
Consider supplementing with collagen
Everyone’s all about the calcium and vitamin D for bones (and teeth), but a large part of the mass of both is actually collagen. And unlike calcium, which most people not living in a food desert get plenty of, or vitamin D, which is one of the most popular supplements around, collagen is something that gets depleted as we get older. We’ve written about its importance for bones:
We Are Such Stuff As Fish Are Made Of—Collagen’s benefits are more than skin deep
And as for its role in combatting gum disease and tooth loss:
Nanoscale Dynamics of Streptococcal Adhesion to AGE-Modified Collagen
By the way, that “AGE” there isn’t about chronological age; it’s about advanced glycation end-products. Those are also something you can and should avoid:
A different kind of “spit and polish”
We imagine you have the “polishing” part in hand; that’s tooth-brushing, of course. But spit?
Saliva is hugely important for our oral health, but it’s not something most of us think about a lot. For example, you might not have known (or might have known but not thought much about) that many common medications affect our saliva, including many blood pressure medications and antidepressants:
Impact of ageing and drug consumption on oral health
Because there are so many possibilities, this is the kind of thing to check with your pharmacist or doctor about. But as a rule, if you take a medication whose side-effects include “dry mouth”, this might be you.
Here’s a really useful (academic) article that covers what drugs cause this, how to diagnose it, and what can be done about it:
Hyposalivation in Elderly Patients
If something’s difficult, find a way to make it easier
Sometimes, as we get older, some things that used to be easy, aren’t. We can lose strength, coordination, manual dexterity, memory, attention, and more. Obviously, we try not to, and do what we can to keep ourselves in good health.
But, if you do have some disability that makes for example brushing and/or flossing difficult to do consistently and/or well, consider talking to your doctor to see if there are assistive devices that can help, or some other kind of support that could allow you to do what you need to.
There’s never any shame in getting help if we need it.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Galveston Diet Cookbook for Beginners – by Martha McGrew
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We recently reviewed “The Galveston Diet”, and here’s a cookbook (by a nutritionist) to support that.
For the most part, it’s essentially keto-leaning, with an emphasis on protein and fats, but without quite the carb-cut that keto tends to have. It’s also quite plant-centric, but it’s not by default vegan or even vegetarian; you will find meat and fish in here. As you might expect from an anti-inflammatory cookbook, it’s light on the dairy too, though fermented dairy products such as yogurt do feature as well.
The recipes are quite simple and easy to follow, with suggestions of alternative ingredients along the way, making for extra variety as well as convenience.
If you are going to buy this book, you might want to take a look at the buying options, to ensure you get a full-color version, as recent reprints have photos in black and white, whereas older runs have color throughout.
Bottom line: if you’d like to cook the Galveston Diet way, this is as good a way to start as any.
Click here to check out the Galveston Diet Cookbook for Beginners, and get cooking!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What causes the itch in mozzie bites? And why do some people get such a bad reaction?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Are you one of these people who loathes spending time outdoors at dusk as the weather warms and mosquitoes start biting?
Female mosquitoes need blood to develop their eggs. Even though they take a tiny amount of our blood, they can leave us with itchy red lumps that can last days. And sometimes something worse.
So why does our body react and itch after being bitten by a mosquito? And why are some people more affected than others?
Arthur Poulin/Unsplash What happens when a mosquito bites?
Mosquitoes are attracted to warm blooded animals, including us. They’re attracted to the carbon dioxide we exhale, our body temperatures and, most importantly, the smell of our skin.
The chemical cocktail of odours from bacteria and sweat on our skin sends out a signal to hungry mosquitoes.
Some people’s skin smells more appealing to mosquitoes, and they’re more likely to be bitten than others.
Once the mosquito has made its way to your skin, things get a little gross.
The mosquito pierces your skin with their “proboscis”, their feeding mouth part. But the proboscis isn’t a single, straight, needle-like tube. There are multiple tubes, some designed for sucking and some for spitting.
Once their mouth parts have been inserted into your skin, the mosquito will inject some saliva. This contains a mix of chemicals that gets the blood flowing better.
There has even been a suggestion that future medicines could be inspired by the anti-blood clotting properties of mosquito saliva.
A common pest mosquito around the world, Culex quinquefasciatus. Cameron Webb (NSW Health Pathology), CC BY It’s not the stabbing of our skin by the mosquito’s mouth parts that hurts, it’s the mozzie spit our bodies don’t like.
Are some people allergic to mosquito spit?
Once a mosquito has injected their saliva into our skin, a variety of reactions can follow. For the lucky few, nothing much happens at all.
For most people, and irrespective of the type of mosquito biting, there is some kind of reaction. Typically there is redness and swelling of the skin that appears within a few hours, but often more quickly, after just a few minutes.
Occasionally, the reaction can cause pain or discomfort. Then comes the itchiness.
Some people do suffer severe reactions to mosquito bites. It’s a condition often referred to as “skeeter syndrome” and is an allergic reaction caused by the protein in the mosquito’s saliva. This can cause large areas of swelling, blistering and fever.
The chemistry of mosquito spit hasn’t really been well studied. But it has been shown that, for those who do suffer allergic reactions to their bites, the reactions may differ depending on the type of mosquito biting.
We all probably get more tolerant of mosquito bites as we get older. Young children are certainly more likely to suffer more following mosquito bites. But as we get older, the reactions are less severe and may pass quickly without too much notice.
How best to treat the bites?
Research into treating bites has yet to provide a single easy solution.
There are many myths and home remedies about what works. But there is little scientific evidence supporting their use.
The best way to treat mosquito bites is by applying a cold pack to reduce swelling and to keep the skin clean to avoid any secondary infections. Antiseptic creams and lotions may also help.
There is some evidence that heat may alleviate some of the discomfort.
It’s particularly tough to keep young children from scratching at the bite and breaking the skin. This can form a nasty scab that may end up being worse than the bite itself.
Applying an anti-itch cream may help. If the reactions are severe, antihistamine medications may be required.
To save the scratching, stop the bites
Of course, it’s better not to be bitten by mosquitoes in the first place. Topical insect repellents are a safe, effective and affordable way to reduce mosquito bites.
Covering up with loose fitted long sleeved shirts, long pants and covered shoes also provides a physical barrier.
Mosquito coils and other devices can also assist, but should not be entirely relied on to stop bites.
There’s another important reason to avoid mosquito bites: millions of people around the world suffer from mosquito-borne diseases. More than half a million people die from malaria each year.
In Australia, Ross River virus infects more than 5,000 people every year. And in recent years, there have been cases of serious illnesses caused by Japanese encephalitis and Murray Valley encephalitis viruses.
Cameron Webb, Clinical Associate Professor and Principal Hospital Scientist, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: