Kiwi vs Grapefruit – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing kiwi to grapefruit, we picked the kiwi.
Why?
In terms of macros, kiwi has nearly 2x the protein, slightly more carbs, and 2x the fiber; both fruits are low glycemic index foods, however.
When it comes to vitamins, kiwi has more of vitamins B3, B6, B7, B9, C, E, K, and choline, while grapefruit has more of vitamins A, B1, B2, and B5. An easy win for kiwi.
In the category of minerals, kiwi is higher in calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while grapefruit is not higher in any minerals. So, no surprises for guessing which wins this category.
One thing that grapefruit is a rich source of: furanocoumarin, which can inhibit cytochrome P-450 3A4 isoenzyme and P-glycoptrotein transporters in the intestine and liver—slowing down their drug metabolism capabilities, thus effectively increasing the bioavailability of many drugs manifold.
This may sound superficially like a good thing (improving bioavailability of things we want), but in practice it means that in the case of many drugs, if you take them with (or near in time to) grapefruit or grapefruit juice, then congratulations, you just took an overdose. This happens with a lot of meds for blood pressure, cholesterol (including statins), calcium channel-blockers, anti-depressants, benzo-family drugs, beta-blockers, and more. Oh, and Viagra, too. Which latter might sound funny, but remember, Viagra’s mechanism of action is blood pressure modulation, and that is not something you want to mess around with unduly. So, do check with your pharmacist to know if you’re on any meds that would be affected by grapefruit or grapefruit juice!
All in all, adding up the categories makes for an overwhelming total win for kiwis.
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer ← kiwi is top of the list!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Undo The Sun’s Damage To Your Skin
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s often said that our skin is our largest organ. Our brain or liver are the largest solid organs by mass (which one comes out on top will vary from person to person), our gut is the longest, and our lungs are the largest by surface area. But our skin is large, noticeable, and has a big impact on the rest of our health.
The sun is one of the main damaging factors for our skin; assorted toxins are also a major threat for many people, and once the skin barrier gets broken, it’s a field-day for bacteria.
So, what can we do about it?
Tretinoin: the skin’s rejuvenator
Tretinoin is also called retinoic acid, not to be mistaken for retinol, although they are both retinoids. Tretinoin is much stronger.
As for what it’s stronger at:
It’s usually prescribed for the treatment of sun-damage, acne, and wrinkles. Paradoxically, it works by inflaming the skin (and then making it better, and having done so, keeping it better).
In few words: it encourages your skin to speed up its life cycle, which means that cells die and are replaced sooner, which means the average age of skin cells will be considerably younger at any given time.
This is the same principle as we see at work when it comes to cellular apoptosis and autophagy in general, and specifically the same idea as we discussed when talking about senolytics, compounds that kill aging cells:
Fisetin: The Anti-Aging Assassin
About that paradoxical inflammation…
❝The topical use of tretinoin as an antiacne agent began almost a half century ago. Since that time it has been successfully used to treat comedonal and inflammatory acne.
Over the intervening years, the beneficial effects of tretinoin have grown from an understanding of its potent cornedolytie-related properties to an evolving appreciation of its antiinflammatory actions.
…
The topical use of clindamycin and tretinoin as a combination treatment modality that includes antibacterial, comedolytic, and antiinflammatoiy properties has proven to be a very effective therapy for treating the various stages of acne
…
It is now becoming increasingly clear that there may be good reasons for these observations.❞
~ Drs. Schmidt & Gans, lightly edited here for brevity
Read in full: Tretinoin: A Review of Its Anti-inflammatory Properties in the Treatment of Acne
Against damage by the sun
The older we get, the more likely sun damage is a problem than acne. And in the case of tretinoin,
❝In several well-controlled clinical trials, the proportion of patients showing improvement was significantly higher with 0.01 or 0.05% tretinoin cream than with placebo for criteria such as global assessment, fine and coarse wrinkling, pigmentation and roughness.
Improvements in the overall severity of photodamage were also significantly greater with tretinoin than with placebo.
…
Several placebo-controlled clinical studies have demonstrated that topical tretinoin has significant efficacy in the treatment of photodamaged skin. Improvements in subjective global assessment scores were recorded in:
49–100% of patients using once-daily 0.01% tretinoin,
68–100% of patients using 0.05% tretinoin, and
0–44% of patients using placebo.❞
~ Drs. Wagstaff & Noble
…which is quite compelling.
Read in full: Tretinoin: A Review of its Pharmacological Properties and Clinical Efficacy in the Topical Treatment of Photodamaged Skin
This is very well-established by now; here’s an old paper from when the mechanism of action was unknown (here in the current day, 17 mechanisms of action have been identified; beyond the scope of this article as we only have so much room, but it’s nice to see science building on science):
❝Tretinoin cream has been used extensively to reverse the changes of photoaging. It is the first topical therapy to undergo controlled clinical testing and proved to be efficacious. These results have been substantiated with photography, histopathologie examination, and skin surface replicas.
…
Tretinoin cream has an excellent safety record; a local cutaneous hypervitaminosis A reaction is the only common problem.❞
~ Dr. Goldfarb et al.
Read in full: Topical tretinoin therapy: Its use in photoaged skin
Is it safe?
For most people, when used as directed*, yes. However, it’s likely to irritate your skin at first, and that’s normal. If this persists more than a few weeks, or seems unduly severe, then you might want to stop and talk to your doctor again.
*See also: Scarring following inappropriate use of 0.05% tretinoin gel
(in the case of a young woman who used it 4x daily instead of 1x daily)
Want to try some?
Tretinoin is prescription-only, so speak with your doctor/pharmacist about that. Alternatively, retinal (not retinol) is the strongest natural alternative that works on the same principles; here’s an example product on Amazon 😎
Take care!
Share This Post
-
Foods Linked To Urinary Incontinence In Middle-Age (& Foods That Avert It)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Incontinence is an inconvenience associated with aging, especially for women. Indeed, as the study we’re going to talk about today noted:
❝Estrogen deficiency during menopause, aging, reproductive history, and factors increasing intra-abdominal pressure may lead to structural and functional failure in the pelvic floor.❞
However, that was just the “background”, before they got the study going, because…
❝Lifestyle choices, such as eating behavior, may contribute to pelvic floor disorders. The objective of the study was to investigate associations of eating behavior with symptoms of pelvic floor disorders, that is, stress urinary incontinence, urgency urinary incontinence, fecal incontinence, and constipation or defecation difficulties among middle-aged women.❞
~ Ibid.
How the study went
The researchers examined 1,098 Finnish women aged 47–55. It was a cross-sectional observational study, so no intervention was made, just: gathering data and analysing it. They examined:
- Eating behavior (i.e. what one’s diet is like; their questionnaire was quite comprehensive and the simplified conclusion doesn’t do that justice)
- Food consumption frequency (i.e. temporal patterns of eating)
- Demographic variables (e.g. age, education, etc)
- Gynecological variables (e.g. menopause status, hysterectomy, etc)
- Physical activity variables (e.g. light, moderate, heavy, previous history of no exercise, regular, competitive sport, etc)
With those things taken into account, the researchers crunched the numbers to assess the associations of dietary factors with pelvic floor disorders.
What they found
Adjusting for possible confounding variables…
- those with disordered eating patterns (e.g. overeating, restrictive eating, swinging between the two behaviors) were 50% higher chance of developing urinary incontinence than the norm
- those who more frequently consumed ready-made foods got 50% higher chance of developing urinary incontinence than the norm
- those who ate fruits daily enjoyed a 20% lower chance of urinary incontinence than the norm
So, in practical terms:
- practice mindful eating
- avoid ready-made foods
- enjoy fruit
You can read the paper in full here (it obviously goes into a lot more detail, and also covers other things beyond the scope of this article, such as fecal incontinence or, conversely, constipation—needless to say, the same advice stands in any case):
As for why this works the way it does: the study focused on the association and only hypothesized the question of “how”, but they did write a bit about that too, and it is almost certainly mostly a matter of gut health vs inflammation.
We really only have room for that kind of one-line summary here, but do read the paper if you’re interested, as it also talks about other dietary factors that had an impact, with the above-listed items being the topmost impactful factors, but for example (to take just one snippet of many possible ones):
❝In particular, saturated fatty acids (SFA) and cholesterol increased the risk for symptoms❞
~ Ibid. ← so do read it, for many more snippets like this!
What else does and doesn’t work
We covered a little while back the question of whether it is strengthening to hold one’s pee, or better to go whenever one feels the urge, and the answer is clear:
Meanwhile, supplements on the other hand are a mixed bag; there are some that probably help, and others, not so much:
What’s in the supplements that claim to help you cut down on bathroom breaks? And do they work?
Want to do more?
Check out these previous articles of ours:
Pelvic Floor Exercises (Not Kegels!) To Prevent Urinary Incontinence
and
Keeping Your Kidneys Happy: It’s About More Than Just Hydration! ← important at all ages, but especially relevant after 60
Take care!
Share This Post
-
The Purple Parsnip’s Bioactive Brain Benefits (& more)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This Root Might Be A Guardian Angel
Sometimes we go searching for supplements to research; sometimes supplements present themselves for examination! In this case, our attention was grabbed by a headline:
Angelica gigas extract emerges as a potential treatment for vascular disease
Angelica who?
Angelica gigas, also called the purple parsnip (amongst other names), is a flowering plant native to Korea. It has assorted medicinal properties, and in this case, it was its heart-healthy benefits that were making news:
❝Ultimately, this study presents clearly evidence that Angelica gigas extract is a promising natural product-based functional food/herbal medicine candidate for preventing or regulating hyperlipidemic cardiovascular complications❞
But it has a lot more to offer…
The root has various bioactive metabolites, but the compounds that most studies are most interested in are decursin and decursinol, for their neuroprotective and cognitive enhancement effects:
❝[C]rude extracts and isolated components from the root of A. gigas exhibited neuroprotective and cognitive enhancement effects.
Neuronal damage or death is the most important factor for many neurodegenerative diseases.
In addition, recent studies have clearly demonstrated the possible mechanisms behind the neuroprotective action of extracts/compounds from the root of A. gigas.❞
That middle paragraph there? That’s one of the main pathogenic processes of Alzheimer’s, Parkinson’s, Huntington’s, and Multiple Sclerosis.
Angelica gigas attenuates (reduces the force of) that process:
❝The published reports revealed that the extracts and isolated components from the root of A. gigas showed neuroprotective and cognitive enhancement properties through various mechanisms such as anti-apoptosis, antioxidative actions, inhibiting mRNA and protein expressions of inflammatory mediators and regulating a number of signaling pathways.
In conclusion, the A. gigas root can serve as an effective neuroprotective agent by modulating various pathophysiological processes❞
Read more: Neuroprotective and Cognitive Enhancement Potentials of Angelica gigas Nakai Root: A Review
Beyond neuroprotection & cognitive enhancement
…and also beyond its protection against vascular disease, which is what got our attention…
Angelica gigas also has antioxidant properties, anti-cancer properties, and general immune-boosting properties.
We’ve only so much room, so: those links above will take you to example studies for those things, but there are plenty more where they came from, so we’re quite confident in this one.
Of course, what has antioxidant properties is usually anti-inflammatory, anti-cancer, and anti-aging, because these things are reliant on many of the same processes as each other, with a lot of overlap.
Where can we get it?
We don’t sell it, but here’s an example product on Amazon, for your convenience
Enjoy!
Share This Post
Related Posts
-
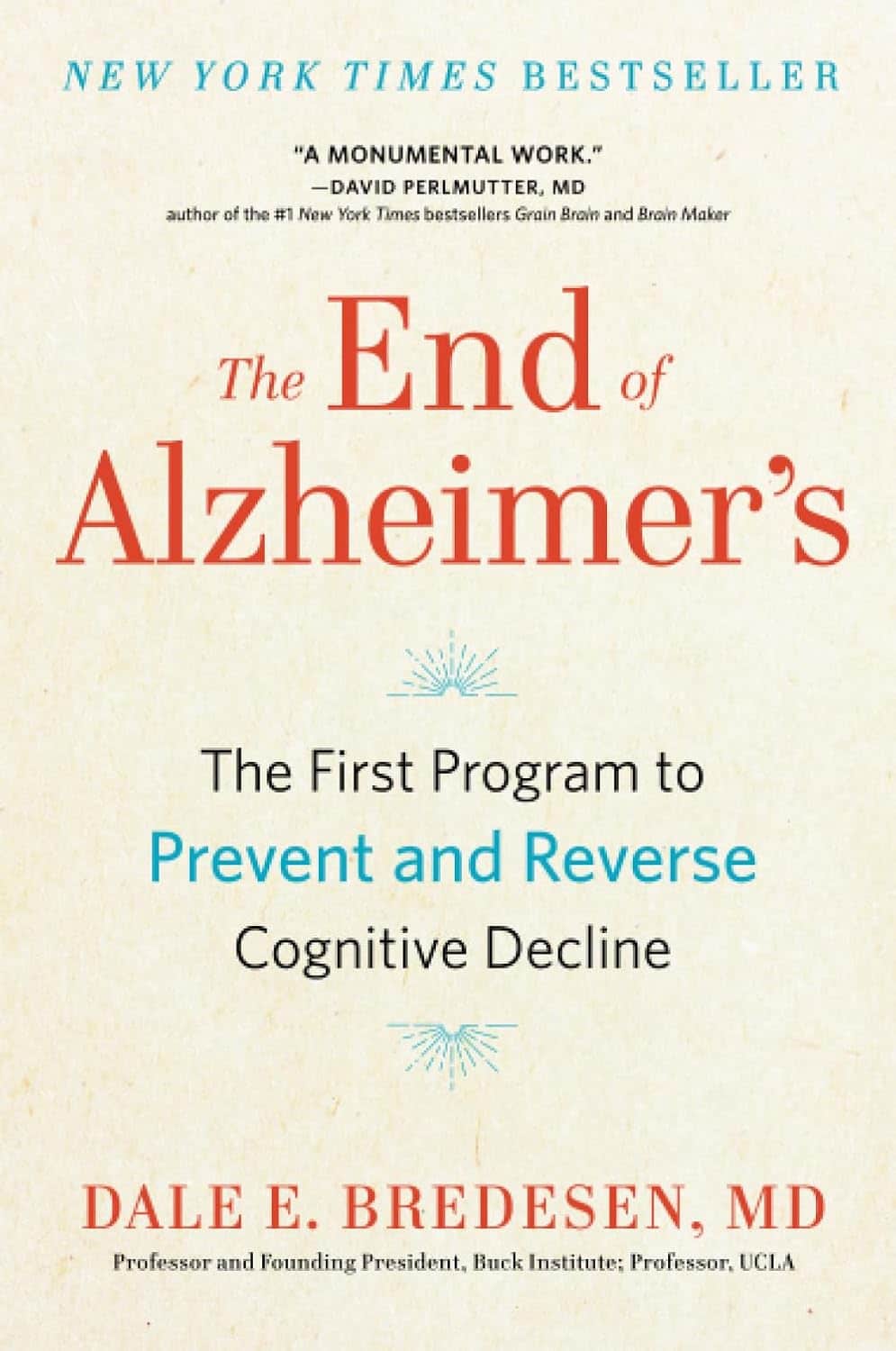
The End of Alzheimer’s – by Dr. Dale Bredesen
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This one didn’t use the “The New Science Of…” subtitle that many books do, and this one actually is a “new science of”!
Which is exciting, and/but comes with the caveat that the overall protocol itself is still undergoing testing, but the results so far are promising. The constituent parts of the protocol are for the most already well-established, but have not previously been put together in this way.
Dr. Bredesen argues that Alzheimer’s Disease is not one condition but three (medical consensus agrees at least that it is a collection of conditions, but different schools of thought slice them differently), and outlines 36 metabolic factors that are implicated, and the good news is, most of them are within our control.
Since there’s a lot to put together, he also offers many workarounds and “crutches”, making for very practical advice.
The style of the book is on the hard end of pop-science, that is to say while the feel and tone is very pop-sciencey, there are nevertheless a lot of words that you might know but your spellchecker probably wouldn’t. He does explain everything along the way, but this does mean that if you’re not already well-versed, you can’t just dip in to a later point without reading the earlier parts.
Bottom line: even if you only implement half the advice in this book, you’ll be doing your long-term cognitive health a huge favor.
Click here to check out The End of Alzheimer’s, and keep cognitive decline at bay!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Rest For The Restless (Legs)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Any tips for dealing with restless legs syndrome?❞
As a neurological disorder (Willis-Ekbom Disease, as it is also called
by almost nobody outside of academia), there’s a lot that’s not known about its pathology, but we do know that looking after one’s nerves can help a lot.This means:
- Avoid alcohol, as this is bad for everything, including nerves
- See also: How To Reduce Or Quit Alcohol
- Don’t smoke, as this is bad for everything, including nerves
- Do exercise those restless legs! It may sound funny, but in seriousness, movement promotes nerve health
- See also: Walking… Better.
- Take care of your blood sugars, because diabetic neuropathy can also cause this
- See also: 10 Ways To Balance Blood Sugars
- Massage your legs, and enjoy a hot bath/shower
You can also take into account the measures recommended for dealing with peripheral neuropathy, e.g:
Peripheral Neuropathy: How To Avoid It, Manage It, Treat It
There are also medication options for RLS; most of them are dopamine agonists, so if you want to try something yourself before going the pharmaceutical route, then things that improve your dopamine levels will probably be a worth checking out. In the category of supplements, you might enjoy:
NALT: The Dopamine Precursor And More
Take care! And… Want something answered here? Send us your questions!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- Avoid alcohol, as this is bad for everything, including nerves
-
Can You Be Fat AND Fit?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The short answer is “yes“.
And as for what that means for your heart and/or all-cause mortality risk: it’s just as good as being fit at a smaller size, and furthermore, it’s better than being less fit at a smaller size.
Here’s the longer answer:
The science
A research team did a systematic review looking at multiple large cohort studies examining the associations between:
- Cardiorespiratory fitness and cardiovascular disease risk
- Cardiorespiratory fitness and all-cause mortality
- BMI and cardiovascular disease risk
- BMI and all-cause mortality
However, they also took this further, and tabulated the data such that they could also establish the cardiovascular disease mortality risk and all-cause mortality risk of:
- Unfit people with “normal” BMI
- Unfit people with “overweight” BMI
- Unfit people with “obese” BMI
- Fit people with “normal” BMI
- Fit people with “overweight” BMI
- Fit people with “obese” BMI
Before we move on, let’s note for the record that BMI is a woeful system in any case, for enough reasons to fill a whole article:
Now, with that in mind, let’s get to the results:
What they found
For cardiovascular disease mortality risk of unfit people specifically, compared to fit people of “normal” BMI:
- Unfit people with “normal” BMI: 2.04x higher risk.
- Unfit people with “overweight” BMI: 2.58x higher risk.
- Unfit people with “obese” BMI: 3.35x higher risk
So here we can see that if you are unfit, then being heavier will indeed increase your CVD mortality risk.
For all-cause mortality risk of unfit people specifically, compared to fit people of “normal” BMI:
- Unfit people with “normal” BMI: 1.92x higher risk.
- Unfit people with “overweight” BMI: 1.82x higher risk.
- Unfit people with “obese” BMI: 2.04x higher risk
This time we see that if you are unfit, then being heavier or lighter than “overweight” will increase your all-cause mortality risk.
So, what about if you are fit? Then being heavier or lighter made no significant difference to either CVD mortality risk or all-cause mortality risk.
Fit individuals, regardless of weight category (normal, overweight, or obese), had significantly lower mortality risks compared to unfit individuals in any weight category.
Note: not just “compared to unfit individuals in their weight category”, but compared to unfit individuals in any weight category.
In other words, if you are obese and have good cardiorespiratory fitness, you will (on average) live longer than an unfit person with “normal” BMI.
You can find the paper itself here, if you want to examine the data and/or method:
Cardiorespiratory fitness, body mass index and mortality: a systematic review and meta-analysis
Ok, so how do I improve the kind of fitness that they measured?
They based their cardiorespiratory fitness on VO2 Max, which scientific consensus holds to be a good measure of how efficiently your body can use oxygen—thus depending on your heart and lungs being healthy.
If you use a fitness tracker that tracks your exercise and your heart rate, it will estimate your VO2 Max for you—to truly measure the VO2 Max itself directly, you’ll need a lot more equipment; basically, access to a lab that tests this. But the estimates are fairly accurate, and so good enough for most personal purposes that aren’t hard-science research.
Next, you’ll want to do this:
53 Studies Later: The Best Way to Improve VO2 Max
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: