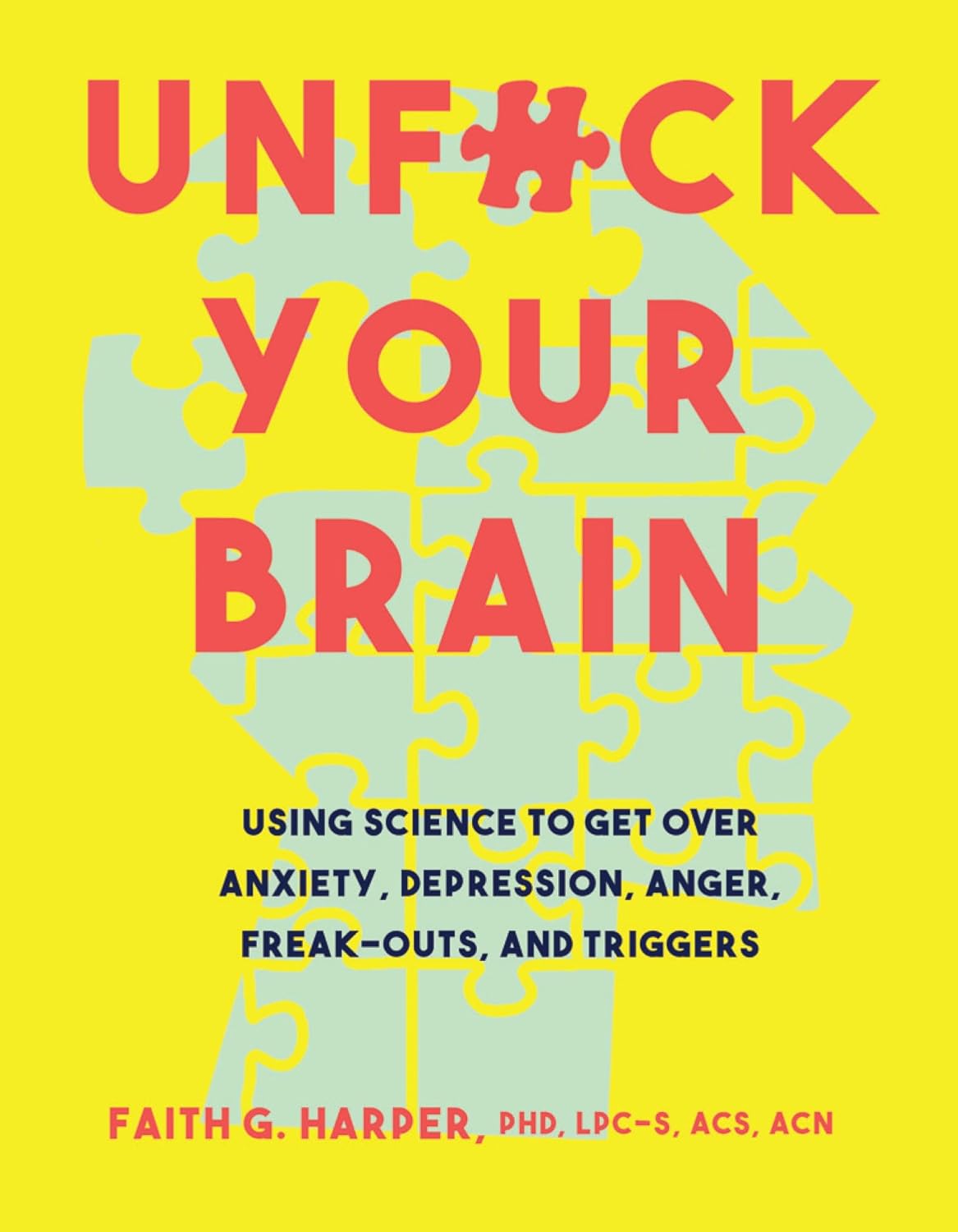
Unfuck Your Brain – by Dr. Faith Harper
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book takes a trauma-informed care approach, which is relatively novel in the mental health field and it’s quickly becoming the industry standard because of its effectiveness.
The basic premise of trauma-informed care is that you had a bad experience (possibly even more than one—what a thought!) and that things that remind you of that will tend to prompt reactivity from you in a way that probably isn’t healthy. By identifying each part of that process, we can then interrupt it, much like we might with CBT (the main difference being that CBT, for all its effectiveness, tends to assume that the things that are bothering you are not true, while TIC acknowledges that they might well be, and that especially historically, they probably were).
A word of warning: if something that triggers a trauma-based reactivity response in you is people swearing, then this book will either cure you by exposure therapy or leave you a nervous wreck, because it’s not just the title; Dr. Harper barely gets through a sentence without swearing. It’s a lot, even by this (European) reviewer’s standards (we’re a lot more relaxed about swearing over here, than people tend to be in America).
On the other hand, something that Dr. Harper excels at is actually explaining stuff very well. So while it sometimes seems like she’s “trying too hard” style-wise in terms of being “not like other therapists”, in her defence she’s nevertheless a very good writer; she knows her stuff, and knows how to communicate it clearly.
Bottom line: if you don’t mind a writer who swears more than 99% of soldiers, then this book is an excellent how-to guide for self-administered trauma-informed care.
Click here to check out Unfuck Your Brain, and indeed unfuck it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Alzheimer’s Sex Differences May Not Be What They Appear
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Alzheimer’s Sex Differences May Not Be What They Appear
Women get Alzheimer’s at nearly twice the rate than men do, and deteriorate more rapidly after onset, too.
So… Why?
There are many potential things to look at, but four stand out for quick analysis:
- Chromosomes: women usually have XX chromosomes, to men’s usual XY. There are outliers to both groups, people with non-standard combinations of chromosomes, but not commonly enough to throw out the stats.
- Hormones: women usually have high estrogen and low testosterone, compared to men. Again there are outliers and this is a huge oversimplification that doesn’t even look at other sex hormones, but broadly speaking (which sounds vague, but is actually what is represented in epidemiological studies), it will be so.
- Anatomy: humans have some obvious sexual dimorphism (again, there are outliers, but again, not enough to throw out the stats); this seems least likely to be relevant (Alzheimer’s is probably not stored in the breasts, for examples), though average body composition (per muscle:fat ratio) could admittedly be a factor.
- Social/lifestyle: once again, #NotAllWomen etc, but broadly speaking, women and men often tend towards different social roles in some ways, and as we know, of course lifestyle can play a part in disease pathogenesis.
As a quick aside before we continue, if you’re curious about those outliers, then a wiki-walk into the fascinating world of intersex conditions, for example, could start here. But by and large, this won’t affect most people.
So… Which parts matter?
Back in 2018, Dr. Maria Teresa Ferretti et al. kicked up some rocks in this regard, looking not just at genes (as much research has focussed on) or amyloid-β (again, well-studied) but also at phenotypes and metabolic and social factors—bearing in mind that all three of those are heavily influenced by hormones. Noting, for example, that (we’ll quote directly here):
- Men and women with Alzheimer disease (AD) exhibit different cognitive and psychiatric symptoms, and women show faster cognitive decline after diagnosis of mild cognitive impairment (MCI) or AD dementia.
- Brain atrophy rates and patterns differ along the AD continuum between the sexes; in MCI, brain atrophy is faster in women than in men.
- The prevalence and effects of cerebrovascular, metabolic and socio-economic risk factors for AD are different between men and women.
See: Sex differences in Alzheimer disease—the gateway to precision medicine
So, have scientists controlled for each of those factors?
Mostly not! But they have found clues, anyway, while noting the limitations of the previous way of conducting studies. For example:
❝Women are more likely to develop Alzheimer’s disease and experience faster cognitive decline compared to their male counterparts. These sex differences should be accounted for when designing medications and conducting clinical trials❞
~ Dr. Feixiong Cheng
Read: Research finds sex differences in immune response and metabolism drive Alzheimer’s disease
Did you spot the clue?
It was “differences in immune response and metabolism”. These things are both influenced by (not outright regulated by, but strongly influenced by) sex hormones.
❝As [hormonal] sex influences both the immune system and metabolic process, our study aimed to identify how all of these individual factors influence one another to contribute to Alzheimer’s disease❞
~ Dr. Justin Lathia
Ignoring for a moment progesterone’s role in metabolism, estrogen is an immunostimulant and testosterone is an immunosuppressant. These thus both also have an effect in inflammation, which yes, includes neuroinflammation.
But wait a minute, shouldn’t that mean that women are more protected, not less?
It should! Except… Alzheimer’s is an age-related disease, and in the age-bracket that generally gets Alzheimer’s (again, there are outliers), menopause has been done and dusted for quite a while.
Which means, and this is critical: post-menopausal women not on HRT are essentially left without the immune boost usually directed by estrogen, while men of the same age will be ticking over with their physiology that (unlike that of the aforementioned women) was already adapted to function with negligible estrogen.
Specifically:
❝The metabolic consequences of estrogen decline during menopause accelerate neuropathology in women❞
~ Dr. Rasha Saleh
Critical idea to take away from all this:
Alzheimer’s research is going to be misleading if it doesn’t take into account sex differences, and not just that, but also specifically age-relevant sex differences—because that can flip the narrative. If we don’t take age into account, we could be left thinking estrogen is to blame, when in fact, it appears to be the opposite.
In the meantime, if you’re a woman of a certain age, you might talk with a doctor about whether HRT could be beneficial for you, if you haven’t already:
❝Women at genetic risk for AD (carrying at least one APOE e4 allele) seem to be particularly benefiting from MHT❞
(MHT = Menopausal Hormone Therapy; also commonly called HRT, which is the umbrella term for Hormone Replacement Therapies in general)
~ Dr. Herman Depypere
Source study: Menopause hormone therapy significantly alters pathophysiological biomarkers of Alzheimer’s disease
Pop-sci press release version: HRT could ward off Alzheimer’s among at-risk women
Take care!
Share This Post
-
The Secret to Mental Health – by George Pransky
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book (and its author) have a sizeable popular following, so it definitely can be said that it has been well-received by many people. The premise in this book is that there is fundamentally nothing wrong with anybody’s brain, and rather everything can be broken down into:
- Mind (the energy and intelligence that animates all life)
- Consciousness (the capacity to be aware of one’s life and experiences)
- Thought (the ability to think, allowing individuals to create their personal experience of reality)
The author explains, over the course of 145 pages, that where anyone with any perceived mental health issue is going wrong is by either lacking self-awareness (Consciousness) or erring by creating an undesirable personal experience of reality (Thought).
In terms of the science of this, frequent references are made to “there is evidence that shows”, “new discoveries about mental health suggest…”, etc, but this claimed evidence is never actually presented, just alluded to. Where many books would have a bibliography, this one has simply a collection of what the author has titled “interesting case studies, conversations, papers, and discussions” (there are no actual case studies or papers; it is just a collection of anecdotes).
The style is… Honestly, in this reviewer’s opinion, barely readable. But, apparently lots of people love it, so your mileage may vary.
We don’t usually delve too far into claimed credentials, but because of the interesting writing style and the bold claims without evidence, we were curious as to where this PhD came from, and apparently it came from a now-shut-down diploma mill that was described by the court as “a complete scam”.
Bottom line: we can’t recommend this one, but we read it so that you don’t have to, and we hope that publishing this review will help reassure you that when we do recommend a book, we mean it!
Share This Post
-
Afterwork – by Joel Malick and Alex Lippert
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Regular 10almonds readers may remember that one of the key unifying factors of Blue Zones supercentenarians is the importance of having purpose, sometimes called ikigai (borrowing the Japanese term, as a nod to the Okinawan Blue Zone).
The authors are financial advisors by profession, but don’t let that fool you; this book is not about retirement financial planning, but rather, simply addressing a problem that was often presented to them while helping people plan their retirements:
A lot of people find themselves adrift without purpose at several points in life. Often, these are: 1) early twenties, 2) some point in the midlife, and/or 3) retirement. This book addresses the third of those life points.
The authors advise cultivating 10 key disciplines; we’ll not keep them a mystery; they are:
- Purpose
- Calendar
- Movement
- Journaling
- Faith
- Connection
- Learning
- Awareness
- Generosity
- Awe
…which each get a chapter in this book.
A note on the chapter about faith: the authors are Christians, and that does influence their perspective here, but if Christianity’s not your thing, then don’t worry: the rest also stands on its own feet without that.
The general “flavor” of the book overall is in essence, embracing a new period of enjoying what is in effect the strongest, most potentially impactful version of you you’ve ever been, as well as avoiding the traps of retirement “sugar rush” and “retirement drift”, to define, well, a more purposeful life—with what’s most meaningful to you.
The style of the book is self-help in layout, with occasional diagrams, flowcharts, and the like; sometimes we see well-sourced stats, but there’s no hard science here. In short, a simple and practical book.
Bottom line: if your retirement isn’t looking like what you imagined it to be, and/or you think it could be more fulfilling, then this book can help you find, claim, and live your ikigai.
Click here to check out Afterwork, and indeed live a future that’s worthy of dreams!
Share This Post
Related Posts
-
New California Laws Target Medical Debt, AI Care Decisions, Detention Centers
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
SACRAMENTO, Calif. — As the nation braces for potential policy shifts under President-elect Donald Trump’s “Make America Healthy Again” mantra, the nation’s most populous state and largest health care market is preparing for a few changes of its own.
With supermajorities in both houses, Democrats in the California Legislature passed — and Democratic Gov. Gavin Newsom signed — laws taking effect this year that will erase medical debt from credit reports, allow public health officials to inspect immigrant detention centers, and require health insurance companies to cover fertility services such as in vitro fertilization.
Still, industry experts say it was a relatively quiet year for health policy in the Golden State, with more attention on a divisive presidential election and with several state legislators seeking to avoid controversial issues as they ran for Congress in competitive swing districts.
Newsom shot down some of legislators’ most ambitious health care policies, including proposals that would have regulated pharmaceutical industry middlemen and given the state more power to stop private equity deals in health care.
Health policy experts say advocates and legislators are now focused on how to defend progressive California policies such as sweeping abortion access in the state and health coverage for immigrants living in the U.S. without authorization.
“I think everyone’s just thinking about how we’re going to enter 2025,” said Rachel Linn Gish, a spokesperson with the consumer health advocacy group Health Access California. “We’re figuring out what is vulnerable, what we are exposed to on the federal side, and what do budget changes mean for our work. That’s kind of putting a cloud over everything.”
Here are some of the biggest new health care laws Californians should know about:
Medical debt
California becomes the eighth state in which medical debt will no longer affect patients’ credit reports or credit scores. SB 1061 bars health care providers and debt collectors from reporting unpaid medical bills to credit bureaus, a practice that supporters of the law say penalizes people for seeking critical care and can make it harder for patients to get a job, buy a car, or secure a mortgage.
Critics including the California Association of Collectors called the measure from Sen. Monique Limón (D-Santa Barbara) a “tremendous overreach” and successfully lobbied for amendments that limited the scope of the bill, including an exemption for any medical debt incurred on credit cards.
The Biden administration has finalized federal rules that would stop unpaid medical bills from affecting patients’ credit scores, but the fate of those changes remains unclear as Trump takes office.
Psychiatric hospital stays for violent offenders
Violent offenders with severe mental illness can now be held longer after a judge orders them released from a state mental hospital.
State officials and local law enforcement will now have 30 days to coordinate housing, medication, and behavioral health treatment for those parolees, giving them far more time than the five-day deadline previously in effect.
The bill drew overwhelming bipartisan support after a high-profile case in San Francisco in which a 61-year-old man was charged in the repeated stabbing of a bakery employee just days after his release from a state mental hospital. The bill’s author, Assembly member Matt Haney (D-San Francisco), called the previous five-day timeline “dangerously short.”
Cosmetics and ‘forever chemicals’
California was the first state to ban PFAS chemicals, also known as “forever chemicals,” in all cosmetics sold and manufactured within its borders. The synthetic compounds, found in everyday products including rain jackets, food packaging, lipstick, and shaving cream, have been linked to cancer, birth defects, and diminished immune function and have been increasingly detected in drinking water.
Industry representatives have argued that use of PFAS — perfluoroalkyl and polyfluoroalkyl substances — is critical in some products and that some can be safely used at certain levels.
Immigration detention facilities
After covid-19 outbreaks, contaminated water, and moldy food became the subjects of detainee complaints and lawsuits, state legislators gave local county health officials the authority to enter and inspect privately run immigrant detention centers. SB 1132, from Sen. María Elena Durazo (D-Los Angeles), gives public health officials the ability to evaluate whether privately run facilities are complying with state and local public health regulations regarding proper ventilation, basic mental and physical health care, and food safety.
Although the federal government regulates immigration, six federal detention centers in California are operated by the GEO Group. One of the country’s largest private prison contractors, GEO has faced a litany of complaints related to health and safety. Unlike public prisons and jails, which are inspected annually, these facilities would be inspected only as deemed necessary.
The contractor filed suit in October to stop implementation of the law, saying it unconstitutionally oversteps the federal government’s authority to regulate immigration detention centers. A hearing in the case is set for March 3, said Bethany Lesser, a spokesperson for California Attorney General Rob Bonta. The law took effect Jan. 1.
Doctors vs. insurance companies using AI
As major insurance companies increasingly use artificial intelligence as a tool to analyze patient claims and authorize some treatment, trade groups representing doctors are concerned that AI algorithms are driving an increase in denials for necessary care. Legislators unanimously agreed.
SB 1120 states that decisions about whether a treatment is medically necessary can be made only by licensed, qualified physicians or other health care providers who review a patient’s medical history and other records.
Sick leave and protected time off
Two new laws expand the circumstances under which California workers may use sick days and other leave. SB 1105 entitles farmworkers who work outdoors to take paid sick leave to avoid heat, smoke, or flooding when local or state officials declare an emergency.
AB 2499 expands the list of reasons employees may take paid sick days or use protected unpaid leave to include assisting a family member who is experiencing domestic violence or other violent crimes.
Prescription labels for the visually impaired
Starting this year, pharmacies will be required to provide drug labels and use instructions in Braille, large print, or audio for blind patients.
Advocates of the move said state law, which already required translated instructions in five languages for non-English speakers, has overlooked blind patients, making it difficult for them to monitor prescriptions and take the correct dosage.
Maternal mental health screenings
Health insurers will be required to bolster maternal mental health programs by mandating additional screenings to better detect perinatal depression, which affects 1 in 5 people who give birth in California, according to state data. Pregnant people will now undergo screenings at least once during pregnancy and then six weeks postpartum, with further screenings as providers deem necessary.
Penalties for threatening health care workers (abortion clinics)
With abortion care at the center of national policy fights, California is cracking down on those who threaten, post personal information about, or otherwise target providers or patients at clinics that perform abortions. Penalties for such behavior will increase under AB 2099, and offenders can face felony charges, up to three years in jail, and $50,000 in fines for repeat or violent offenses. Previously, state law classified many of those offenses as misdemeanors.
Insurance coverage for IVF
Starting in July, state-regulated health plans covering 50 employees or more would be required to cover fertility services under SB 729, passed and signed last year. Advocates have long fought for this benefit, which they say is essential care for many families who have trouble getting pregnant and would ensure LGBTQ+ couples aren’t required to pay more out-of-pocket costs than straight couples when starting a family.
In a signing statement, Newsom asked legislators to delay implementation of the law until 2026 as state officials consider whether to add infertility treatments to the list of benefits that insurance plans are required to cover.
It’s unclear whether legislators intend to address that this session, but a spokesperson for the governor said that Newsom “clearly stated his position on the need for an extension” and that he “will continue to work with the legislature” on the matter.
Plans under CalPERS, the California Public Employees’ Retirement System, would have to comply by July 2027.
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Do You Know These 10 Common Ovarian Cancer Symptoms?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s better to know in advance:
Things you may need to know
The symptoms listed in the video are:
- Abdominal bloating: persistent bloating due to fluid buildup, often mistaken for overeating or weight gain.
- Pelvic or abdominal pain: continuous pain in the lower abdomen or pelvis, unrelated to menstruation.
- Difficulty eating or feeling full quickly: loss of appetite or feeling full after eating only a small amount.
- Urgent or frequent urination: increased need to urinate due to tumor pressure on the bladder.
- Unexplained weight loss: sudden weight loss without changes in diet or exercise (this goes for cancer in general, of course).
- Fatigue: extreme tiredness that doesn’t improve with rest, possibly linked to anemia.
- Back pain: persistent lower back pain due to tumor pressure or fluid buildup.
- Changes in bowel habits: unexplained constipation, diarrhea, or a feeling of incomplete bowel movements.
- Menstrual changes: irregular, heavier, lighter, or missed periods in premenopausal women.
- Pain during intercourse: discomfort or deep pelvic pain during or after vaginal sex—often overlooked!
Of course, some of those things can be caused by many things, but it’s worth getting it checked out, especially if you have a cluster of them together. Even if it’s not ovarian cancer (and hopefully it won’t be), having multiple things from this list certainly means that “something wrong is not right” in any case.
For those who remember better from videos than what you read, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Dating apps could have negative effects on body image and mental health, our research shows
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Around 350 million people globally use dating apps, and they amass an estimated annual revenue of more than US$5 billion. In Australia, 49% of adults report using at least one online dating app or website, with a further 27% having done so in the past.
But while dating apps have helped many people find romantic partners, they’re not all good news.
In a recent review, my colleagues and I found using dating apps may be linked to poorer body image, mental health and wellbeing.
Dikushin Dmitry/Shutterstock We collated the evidence
Our study was a systematic review, where we collated the results of 45 studies that looked at dating app use and how this was linked to body image, mental health or wellbeing.
Body image refers to the perceptions or feelings a person has towards their own appearance, often relating to body size, shape and attractiveness.
Most of the studies we included were published in 2020 onwards. The majority were carried out in Western countries (such as the United States, the United Kingdom and Australia). Just under half of studies included participants of all genders. Interestingly, 44% of studies observed men exclusively, while only 7% included just women.
Of the 45 studies, 29 looked at the impact of dating apps on mental health and wellbeing and 22 considered the impact on body image (some looked at both). Some studies examined differences between users and non-users of dating apps, while others looked at whether intensity of dating app use (how often they’re used, how many apps are used, and so on) makes a difference.
More than 85% of studies (19 of 22) looking at body image found significant negative relationships between dating app use and body image. Just under half of studies (14 of 29) observed negative relationships with mental health and wellbeing.
The studies noted links with problems including body dissatisfaction, disordered eating, depression, anxiety and low self-esteem.
Dating apps are becoming increasingly common. But could their use harm mental health? Rachata Teyparsit/Shutterstock It’s important to note our research has a few limitations. For example, almost all studies included in the review were cross-sectional – studies that analyse data at a particular point in time.
This means researchers were unable to discern whether dating apps actually cause body image, mental health and wellbeing concerns over time, or whether there is simply a correlation. They can’t rule out that in some cases the relationship may go the other way, meaning poor mental health or body image increases a person’s likelihood of using dating apps.
Also, the studies included in the review were mostly conducted in Western regions with predominantly white participants, limiting our ability to generalise the findings to all populations.
Why are dating apps linked to poor body image and mental health?
Despite these limitations, there are plausible reasons to expect there may be a link between dating apps and poorer body image, mental health and wellbeing.
Like a lot of social media, dating apps are overwhelmingly image-centric, meaning they have an emphasis on pictures or videos. Dating app users are initially exposed primarily to photos when browsing, with information such as interests or hobbies accessible only after manually clicking through to profiles.
Because of this, users often evaluate profiles based primarily on the photos attached. Even when a user does click through to another person’s profile, whether or not they “like” someone may still often be determined primarily on the basis of physical appearance.
This emphasis on visual content on dating apps can, in turn, cause users to view their appearance as more important than who they are as a person. This process is called self-objectification.
People who experience self-objectification are more likely to scrutinise their appearance, potentially leading to body dissatisfaction, body shame, or other issues pertaining to body image.
Dating apps are overwhelmingly image-centric. Studio Romantic/Shutterstock There could be several reasons why mental health and wellbeing may be impacted by dating apps, many of which may centre around rejection.
Rejection can come in many forms on dating apps. It can be implied, such as having a lack of matches, or it can be explicit, such as discrimination or abuse. Users who encounter rejection frequently on dating apps may be more likely to experience poorer self-esteem, depressive symptoms or anxiety.
And if rejection is perceived to be based on appearance, this could lead again to body image concerns.
What’s more, the convenience and game-like nature of dating apps may lead people who could benefit from taking a break to keep swiping.
What can app developers do? What can you do?
Developers of dating apps should be seeking ways to protect users against these possible harms. This could, for example, include reducing the prominence of photos on user profiles, and increasing the moderation of discrimination and abuse on their platforms.
The Australian government has developed a code of conduct – to be enforced from April 1 this year – to help moderate and reduce discrimination and abuse on online dating platforms. This is a positive step.
Despite the possible negatives, research has also found dating apps can help build confidence and help users meet new people.
If you use dating apps, my colleagues and I recommend choosing profile images you feel display your personality or interests, or photos with friends, rather than semi-clothed images and selfies. Engage in positive conversations with other users, and block and report anyone who is abusive or discriminatory.
It’s also sensible to take breaks from the apps, particularly if you’re feeling overwhelmed or dejected.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14. The Butterfly Foundation provides support for eating disorders and body image issues, and can be reached on 1800 334 673.
Zac Bowman, PhD Candidate, College of Education, Psychology & Social Work, Flinders University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: