Kiwi vs Lime – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing kiwi to lime, we picked the kiwi.
Why?
Looking at the macros first, kiwi has more protein, more carbs, and more fiber. As with most fruits, the fiber is the number we’re most interested in for health purposes; in this case, kiwi is just slightly ahead of lime on all three of those.
In terms of vitamins, kiwi has more of vitamins A, B2, B3, B6, B9, C, E, K, and choline, while lime has a tiny bit more vitamin B5. As in, the vitamin that’s in pretty much anything and is practically impossible to be deficient in unless you are literally starving to death. You may be thinking: aren’t limes a famously good source of vitamin C? And yes, yes they are. But kiwis have >3x more. In other big differences, kiwis also have >6x more vitamin E and >67 times more vitamin K.
When it comes to minerals, kiwi has more calcium, copper, magnesium, manganese, phosphorus, potassium, and zinc, while lime has more iron and selenium. Another easy win for kiwis.
In short: enjoy both; both are good. But kiwis are the more nutritionally dense option by almost every way of measuring it.
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer ← kiwi is top of the list; it promotes cancer cell death while sparing healthy cells
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Many Benefits Of Taking PQQ
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’re going to start this one by quoting directly from the journal “Current Research in Food Science”, because it provides a very convenient list of benefits for us to look at:
- PQQ is a potent antioxidant that supports redox balance and mitochondrial function, vital for energy and health.
- PQQ contributes to lipid metabolism regulation, indicating potential benefits for energy management.
- PQQ supplementation is linked to weight control, improved insulin sensitivity, and may help prevent metabolic disorders.
- PQQ may attenuate inflammation, bolster cognitive and cardiovascular health, and potentially assist in cancer therapies.
Future research should investigate PQQ dosages, long-term outcomes, and its potential for metabolic and cognitive health. The translation of PQQ research into clinical practice could offer new strategies for managing metabolic disorders, enhancing cognitive health, and potentially extending lifespan.
What is it?
It’s a redox-active (and thus antioxidant) quinone molecule, and essential vitamin co-factor, that not only helps mitochondria to do their thing, but also supports the creation of new mitochondria.
For more detail, you can read all about that here: Pyrroloquinoline Quinone, a Redox-Active o-Quinone, Stimulates Mitochondrial Biogenesis by Activating the SIRT1/PGC-1α Signaling Pathway
It’s first and foremost made by bacteria, and/but it’s present in many foods, including kiwi fruit, spinach, celery, soybeans, human breast milk, and mouse breast milk.
You may be wondering why “mouse breast milk” makes the list. The causal reason is simply that research scientists do a lot of work with mice, and so it was discovered. If you would argue it is not a food because it is breast milk from another species, then ask yourself if you would have said the same if it came from a cow or goat—only social convention makes it different!
For any vegans reading: ok, you get a free pass on this one :p
This information sourced from: Pyrroloquinoline Quinone: Its Profile, Effects on the Liver and Implications for Health and Disease Prevention
On which note…
Against non-alcoholic fatty liver disease
From the above-linked study:
❝Antioxidant supplementation can reverse hepatic steatosis, suggesting dietary antioxidants might have potential as therapeutics for nonalcoholic fatty liver disease (NAFLD) or nonalcoholic steatohepatitis (NASH).
An extraordinarily potent dietary antioxidant is pyrroloquinoline quinone (PQQ). PQQ is a ubiquitous, natural, and essential bacterial cofactor found in soil, plants, and interstellar dust. The major source of PQQ in mammals is dietary; it is common in leafy vegetables, fruits, and legumes, especially soy, and is found in high concentrations in human and mouse breast milk.
This chapter reviews chemical and biological properties enabling PQQ’s pleiotropic actions, which include modulating multiple signaling pathways directly (NF-κB, JNK, JAK-STAT) and indirectly (Wnt, Notch, Hedgehog, Akt) to improve liver pathophysiology. The role of PQQ in the microbiome is discussed, as PQQ-secreting probiotics ameliorate oxidative stress–induced injury systemwide. A limited number of human trials are summarized, showing safety and efficacy of PQQ❞
…which is all certainly good to see.
Source: Ibid.
Against obesity
And especially, against metabolic obesity, in other words, against the accumulation of visceral and hepatic fat, which are much much worse for the health than subcutaneous fat (that’s the fat you can physically squish and squeeze from the outside with your hands):
❝In addition to inhibiting lipogenesis, PQQ can increase mitochondria number and function, leading to improved lipid metabolism. Besides diet-induced obesity, PQQ ameliorates programing obesity of the offspring through maternal supplementation and alters gut microbiota, which reduces obesity risk.
In obesity progression, PQQ mitigates mitochondrial dysfunction and obesity-associated inflammation, resulting in the amelioration of the progression of obesity co-morbidities, including non-alcoholic fatty liver disease, chronic kidney disease, and Type 2 diabetes.
Overall, PQQ has great potential as an anti-obesity and preventive agent for obesity-related complications.❞
Read in full: Pyrroloquinoline-quinone to reduce fat accumulation and ameliorate obesity progression
Against aging
This one’s particularly interesting, because…
❝PQQ’s modulation of lactate acid and perhaps other dehydrogenases enhance NAD+-dependent sirtuin activity, along with the sirtuin targets, such as PGC-1α, NRF-1, NRF-2 and TFAM; thus, mediating mitochondrial functions. Taken together, current observations suggest vitamin-like PQQ has strong potential as a potent therapeutic nutraceutical❞
If you’re not sure about what NAD+ is, you can read about it here: NAD+ Against Aging
And if you’re not sure what sirtuins do, you can read about those here: Dr. Greger’s Anti-Aging Eight ← it’s at the bottom!
Want to try some?
As mentioned, it can be found in certain foods, but to guarantee getting enough, and/or if you’d simply like it in supplement form, here’s an example product on Amazon 😎
Enjoy!
Share This Post
-
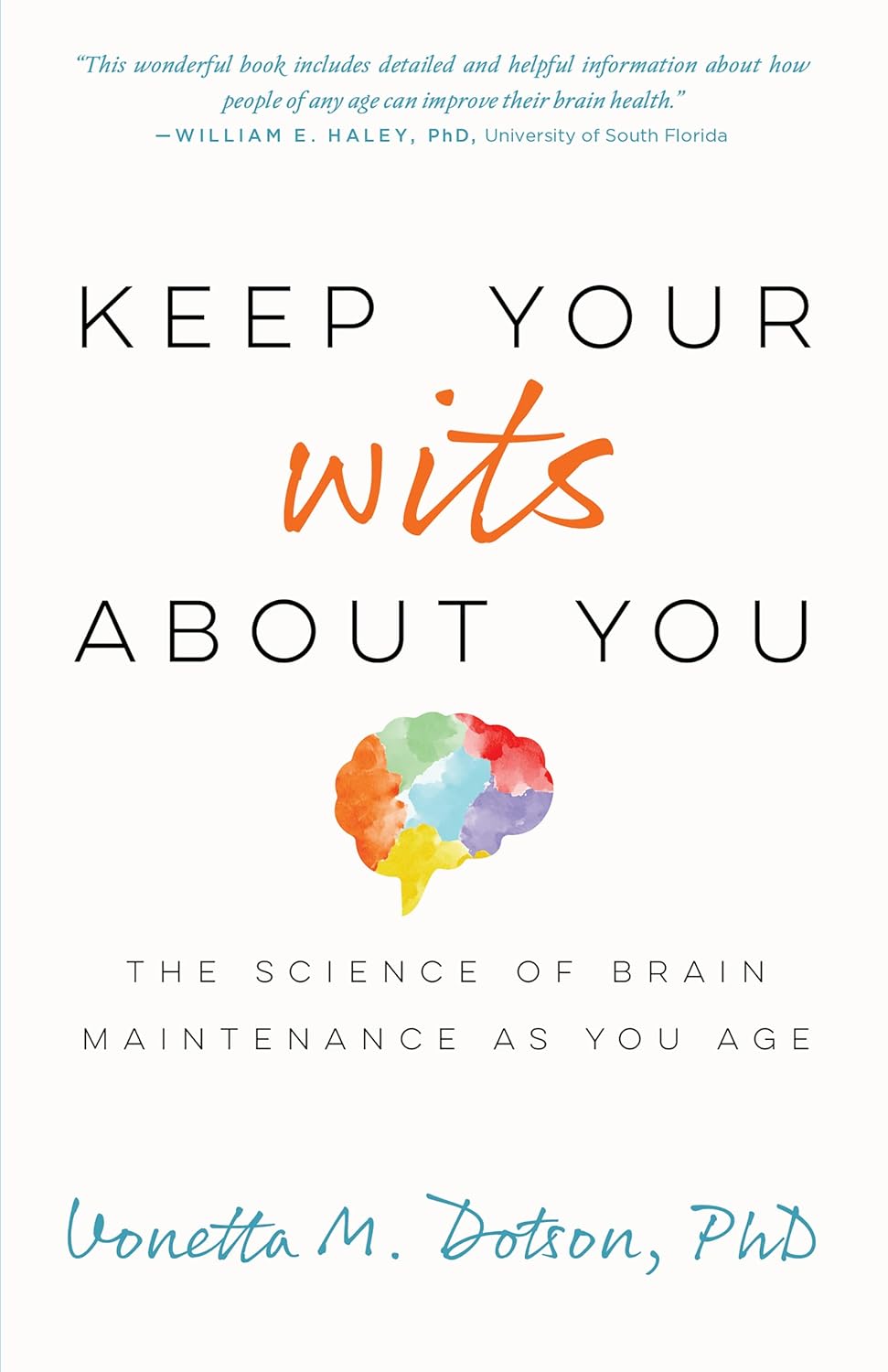
Keep Your Wits About You – by Dr. Vonetta Dotson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Dotson sets out to provide the reader with the tools to maintain good brain health at any age, though she does assume the reader to be in midlife or older.
She talks us through the most important kinds of physical activity, mental activity, and social activity, as well as a good grounding in brain-healthy nutrition, and how to beat the often catch-22 situation of poor sleep.
If you are the sort of person who likes refreshers on what you have just read, you’ll enjoy that the final two chapters repeat the information from chapters 2–6. If not, then well, if you skip the final 2 chapters the book will be 25% shorter without loss of content.
The style is enthusiastic; when it comes to her passion for the brain, Dr. Dotson both tells and shows, in abundance. While some authors may take care to break down the information in a way that can be understood from skimming alone, Dr. Dotson assumes that the reader’s interest will match hers, and thus will not mind a lot of lengthy prose with in-line citations. So, provided that’s the way you like to read, it’ll suit you too.
Bottom line: if you are looking for a book on maintaining optimal brain health that covers the basics without adding advice that is out of the norm, then this is a fine option for that!
Click here to check out Keep Your Wits About You, and keep your wits about you!
Share This Post
-
How Ibogaine Can Beat Buprenorphine For Beating Addictions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Questions?❞
It seems that this week, everyone was so satisfied with our information, that we received no questions! (If you sent one and we somehow missed it, please accept our apologies and do bring our attention to it)
However, we did receive some expert feedback that we wanted to share because it’s so informative:
❝I work at a detox rehab in Mexico, where we can use methods not legal in the United States. Therefore, while much of the linked articles had useful information, I’m in the “trenches” every day, and there’s some information I’d like to share that you may wish to share, with additional information:
- Buprenorphine is widely used and ineffective for addiction because it’s synthetic and has many adverse side effects. For heavy drug users it isn’t enough and they still hit the streets for more opioid, resulting in fentanyl deaths. Depending on length of usage and dose, it can take WEEKS to get off of, and it’s extremely difficult.
- Ibogaine is the medicine we use to detox people off opiates, alcohol, meth as well as my own specialty, bulimia. It’s psychoactive and it temporarily “resets” the brain to a pre-addictive state. Supplemented by behavior and lifestyle changes, as well as addressing the traumas that led to the addiction is extremely effective.
Our results are about 50%, meaning the client is free of the substance or behavior 1 year later. Ibogaine isn’t a “magic pill” or cure, it’s an opening tool that makes the difficult work of reclaiming one’s life easier.
Ibogaine is not something that should be done outside a medical setting. It requires an EKG to ensure the heart is healthy and doesn’t have prolonged QT intervals; also blood testing to ensure organs are functioning (especially the liver) and mineral levels such as magnetic and potassium are where they should be. It is important that this treatment be conducted by experienced doctors or practitioners, and monitoring vital signs constantly is imperative.
I’m taking time to compose this information because it needs to be shared that there is an option available most people have not heard about.❞
~ 10almonds reader (slightly edited for formatting and privacy)
Thank you for that! Definitely valuable information for people to know, and (if applicable for oneself or perhaps a loved one) ask about when it comes to local options.
We see it’s also being studied for its potential against other neurological conditions, too:
❝The combination of ibogaine and antidepressants produces a synergistic effect in reducing symptoms of psychiatric disorders such as bipolar disorder, depression, schizophrenia, paranoia, anxiety, panic disorder, mania, post-traumatic stress disorder (PTSD), and obsessive–compulsive disorder. Though ibogaine and the antidepressant act in different pathways, together they provide highly efficient therapeutic responses compared to when each of the active agents is used alone.❞
Read more: Ibogaine and Their Analogs as Therapeutics for Neurological and Psychiatric Disorders
For those who missed it, today’s information about ibogaine was in response to our article:
Let’s Get Letting Go (Of These Three Things)
…which in turn referenced our previous main feature:
Which Addiction-Quitting Methods Work Best?
Take care!
Share This Post
Related Posts
-
Best Salt for Neti Pots?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
❓ Q&A With 10almonds Subscribers!
Q: What kind of salt is best for neti pots?
A: Non-iodised salt is usually recommended, but really, any human-safe salt is fine. By this we mean for example:
- Sodium chloride (like most kitchen salts),
- Potassium chloride (as found in “reduced sodium” kitchen salts), or
- Magnesium sulfate (also known as epsom salts).
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Best Mobility Exercises For Each Joint
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Stiff joints and tight muscles limit movement, performance, and daily activities. They also increase the risk of injury, and increase recovery time if the injury happens. So, it’s pretty important to take care of that!
Here’s how
Key to joint health involves understanding mobility, flexibility, and stability:
- Mobility: active joint movement through a range of motion.
- Flexibility: muscle lengthening passively through a range of motion.
- Stability: body’s ability to return to position after disturbance.
Different body parts have different needs when it comes to prioritizing mobility, flexibility, and stability exercises. So, with that in mind, here’s what to do for your…
- Wrists: flexibility and stability (e.g., wrist circles, loaded flexions/extensions).
- Elbows: Stability is key; exercises like wrist and shoulder movements benefit elbows indirectly.
- Shoulders: mobility and stability; exercises include prone arm circles, passive hangs, active prone raises, easy bridges, and stick-supported movements.
- Spine: mobility and stability; recommended exercises include cat-cow and quadruped reach.
- Hips: mobility and flexibility through deep squat hip rotations; beginners can use hands for support.
- Knees: stability; exercises include elevated pistols, Bulgarian split squats, lunges, and single-leg balancing.
- Ankles: flexibility and stability; exercises include lunges, prying goblet squats, and deep squats with support if necessary.
For more on all of these, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Building & Maintaining Mobility
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tempeh vs Tofu – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing tempeh to tofu, we picked the tempeh.
Why?
Per 100g, tempeh has about 1.5x as many calories, about 2x as much protein, about 3x as much fiber, and about 4x the carbohydrates.
Which latter sounds like a lot, but really, the amounts here are small—tempeh is under 12% carbohydrates, and most of that is treated by the body as fiber (e.g. it’s a resistant starch).
Both have no sugar, and both have more or less the same (tiny) amount of fat.
Micronutrients, you ask? As they’re both made from soybeans, the micronutrient profiles are similar, but exact amounts will depend on the method used, so by all means check labels if comparing products in store. By and large, there’s usually not much difference, though.
You can see sample stats here:
In summary
Both are great, and/but tempeh is the more nutrient-dense of the two.
Therefore, tempeh is the healthier option, unless you are on a very strictly calorie-controlled diet, in which case, tofu will give you more quantity per calorie.
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: