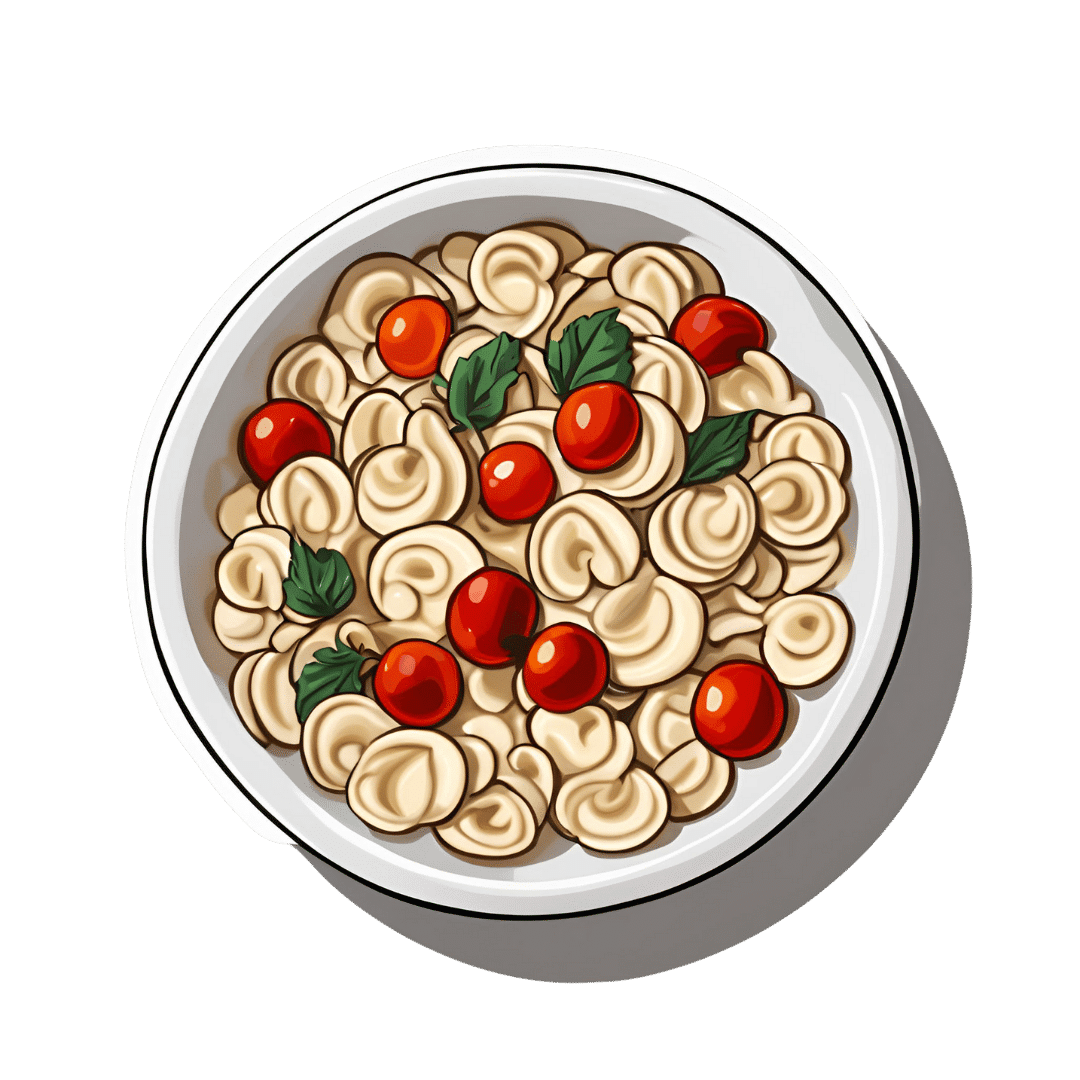
Gut-Healthy Labneh Orecchiette
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Labneh (a sort of yogurt-cheese made from strained yogurt) is a great probiotic, and there’s plenty of resistant starch in this dish too, from how we cook, cool, and reheat the pasta. Add to this the lycopene from the tomatoes, the ergothioneine from the mushrooms, and the healthful properties of the garlic, black pepper, and red chili, and we have a very healthy dish!
You will need
- 10 oz labneh (if you can’t buy it locally, you can make your own by straining Greek yogurt through a muslin cloth, suspended over a bowl to catch the water that drips out, overnight—and yes, plant-based is also fine if you are vegan, and the gut benefits are similar because unlike vegan cheese, vegan yogurt is still fermented)
- 6 oz wholegrain orecchiette (or other pasta, but this shape works well for this sauce)
- ¼ bulb garlic, grated
- Juice of ½ lemon
- Large handful chopped parsley
- Large handful chopped dill
- 9 oz cherry tomatoes, halved
- 9 oz mushrooms (your choice what kind), sliced (unless you went for shiitake or similar, which don’t need it due to already being very thin)
- 2 tsp black pepper, coarse ground
- 1 tsp red chili flakes
- ¼ tsp MSG or ½ tsp low-sodium salt
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Cook the pasta as you normally would. Drain, and rinse with cold water. Set aside.
2) Combine the labneh with the garlic, black pepper, dill, parsley, and lemon juice, in a large bowl. Set aside.
3) Heat a little olive oil in a skillet; add the chili flakes, followed by the mushrooms. Cook until soft and browned, then add the tomatoes and fry for a further 1 minute—we want the tomatoes to be blistered, but not broken down. Stir in the MSG/salt, and take off the heat.
4) Refresh the pasta by passing a kettle of boiling water through it in a colander, then add the hot pasta to the bowl of labneh sauce, stirring to coat thoroughly.
5) Serve, spooning the mushrooms and tomatoes over the labneh pasta.

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Making Friends With Your Gut (You Can Thank Us Later)
- Lycopene’s Benefits For The Gut, Heart, Brain, & More
- “The Longevity Vitamin” (That’s Not A Vitamin)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tastes from our past can spark memories, trigger pain or boost wellbeing. Here’s how to embrace food nostalgia
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Have you ever tried to bring back fond memories by eating or drinking something unique to that time and place?
It could be a Pina Colada that recalls an island holiday? Or a steaming bowl of pho just like the one you had in Vietnam? Perhaps eating a favourite dish reminds you of a lost loved one – like the sticky date pudding Nanna used to make?
If you have, you have tapped into food-evoked nostalgia.
As researchers, we are exploring how eating and drinking certain things from your past may be important for your mood and mental health.
Halfpoint/Shutterstock Bittersweet longing
First named in 1688 by Swiss medical student, Johannes Hoffer, nostalgia is that bittersweet, sentimental longing for the past. It is experienced universally across different cultures and lifespans from childhood into older age.
But nostalgia does not just involve positive or happy memories – we can also experience nostalgia for sad and unhappy moments in our lives.
In the short and long term, nostalgia can positively impact our health by improving mood and wellbeing, fostering social connection and increasing quality of life. It can also trigger feelings of loneliness or meaninglessness.
We can use nostalgia to turn around a negative mood or enhance our sense of self, meaning and positivity.
Research suggests nostalgia alters activity in the brain regions associated with reward processing – the same areas involved when we seek and receive things we like. This could explain the positive feelings it can bring.
Nostalgia can also increase feelings of loneliness and sadness, particularly if the memories highlight dissatisfaction, grieving, loss, or wistful feelings for the past. This is likely due to activation of brain areas such as the amygdala, responsible for processing emotions and the prefrontal cortex that helps us integrate feelings and memories and regulate emotion.
How to get back there
There are several ways we can trigger or tap into nostalgia.
Conversations with family and friends who have shared experiences, unique objects like photos, and smells can transport us back to old times or places. So can a favourite song or old TV show, reunions with former classmates, even social media posts and anniversaries.
What we eat and drink can trigger food-evoked nostalgia. For instance, when we think of something as “comfort food”, there are likely elements of nostalgia at play.
Foods you found comforting as a child can evoke memories of being cared for and nurtured by loved ones. The form of these foods and the stories we tell about them may have been handed down through generations.
Food-evoked nostalgia can be very powerful because it engages multiple senses: taste, smell, texture, sight and sound. The sense of smell is closely linked to the limbic system in the brain responsible for emotion and memory making food-related memories particularly vivid and emotionally charged.
But, food-evoked nostalgia can also give rise to negative memories, such as of being forced to eat a certain vegetable you disliked as a child, or a food eaten during a sad moment like a loved ones funeral. Understanding why these foods evoke negative memories could help us process and overcome some of our adult food aversions. Encountering these foods in a positive light may help us reframe the memory associated with them.
Just like mum used to make. Food might remind you of the special care you received as a child. Galina Kovalenko/Shutterstock What people told us about food and nostalgia
Recently we interviewed eight Australians and asked them about their experiences with food-evoked nostalgia and the influence on their mood. We wanted to find out whether they experienced food-evoked nostalgia and if so, what foods triggered pleasant and unpleasant memories and feelings for them.
They reported they could use foods that were linked to times in their past to manipulate and influence their mood. Common foods they described as particularly nostalgia triggering were homemade meals, foods from school camp, cultural and ethnic foods, childhood favourites, comfort foods, special treats and snacks they were allowed as children, and holiday or celebration foods. One participant commented:
I guess part of this nostalgia is maybe […] The healing qualities that food has in mental wellbeing. I think food heals for us.
Another explained
I feel really happy, and I guess fortunate to have these kinds of foods that I can turn to, and they have these memories, and I love the feeling of nostalgia and reminiscing and things that remind me of good times.
Yorkshire pudding? Don’t mind if I do. Rigsbyphoto/Shutterstock Understanding food-evoked nostalgia is valuable because it provides us with an insight into how our sensory experiences and emotions intertwine with our memories and identity. While we know a lot about how food triggers nostalgic memories, there is still much to learn about the specific brain areas involved and the differences in food-evoked nostalgia in different cultures.
In the future we may be able to use the science behind food-evoked nostalgia to help people experiencing dementia to tap into lost memories or in psychological therapy to help people reframe negative experiences.
So, if you are ever feeling a little down and want to improve your mood, consider turning to one of your favourite comfort foods that remind you of home, your loved ones or a holiday long ago. Transporting yourself back to those times could help turn things around.
Megan Lee, Senior Teaching Fellow, Psychology, Bond University; Doug Angus, Assistant Professor of Psychology, Bond University, and Kate Simpson, Sessional academic, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Healing Spices – by Dr. Bharat Aggarwal & Debora Yost
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is exactly what the subtitle promises it to be, and more. It’s actually herbs and spices, but definitely mostly spices, and includes the kinds found in even the smallest supermarket, to some you might not have heard of, and might need to order online.
We are treated to an explanation of the health-giving properties of each (and any potential contraindications), as well as the culinary properties, many tables of what goes with what and how and why, and even recipes to use them in. For the more adventurous, there’s even advice on how to grow, prepare, and store each of them.
An extra benefit is that everything is cross-linked such that you can look things up by spice or by health condition or by flavor profile, and find what you need and what’ll go with it.
The style is simple and informational, clearly laid-out in encyclopedic form.
Bottom line: this book should be in your kitchen (or related nearby kitchen-book-place).
Click here to check out Healing Spices, and advance your culinary repertoire!
Share This Post
-
Tempeh vs Tofu – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing tempeh to tofu, we picked the tempeh.
Why?
Per 100g, tempeh has about 1.5x as many calories, about 2x as much protein, about 3x as much fiber, and about 4x the carbohydrates.
Which latter sounds like a lot, but really, the amounts here are small—tempeh is under 12% carbohydrates, and most of that is treated by the body as fiber (e.g. it’s a resistant starch).
Both have no sugar, and both have more or less the same (tiny) amount of fat.
Micronutrients, you ask? As they’re both made from soybeans, the micronutrient profiles are similar, but exact amounts will depend on the method used, so by all means check labels if comparing products in store. By and large, there’s usually not much difference, though.
You can see sample stats here:
In summary
Both are great, and/but tempeh is the more nutrient-dense of the two.
Therefore, tempeh is the healthier option, unless you are on a very strictly calorie-controlled diet, in which case, tofu will give you more quantity per calorie.
Enjoy!
Share This Post
Related Posts
-
Apples vs Figs – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing apples to figs, we picked the figs.
Why?
These two fruits are both known for being quite rich in sugar (but also rich in fiber, which offsets it metabolically), and indeed their macros are quite similar. That said, figs have slightly more protein, fiber, and carbs. Both are considered low glycemic index foods. We can consider this category a tie, or perhaps a nominal win for apples, whose glycemic index is the lower of the two. But since figs’ GI is also low, it’s really not a deciding factor.
In terms of vitamins, apples have more of vitamins C and E, while figs have more of vitamins A, B1, B2, B3, B5, B6, B9, and choline, with noteworthy margins of difference. A clear for figs here.
When it comes to minerals, apples are not higher in any minerals, while figs are several times higher in calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. An overwhelming win for figs.
Of course, enjoy either or both, but if you want nutritional density, apples simply cannot compete with figs.
Want to learn more?
You might like to read:
Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Brussels Sprouts vs Spirulina – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing Brussels sprouts to spirulina, we picked the sprouts.
Why?
Pitting these two well-known superfoods against each other, we get the following:
Looking at the macros first, spirulina has a little more protein, while sprouts have more carbs and nearly 10x the fiber. So, we call this a win for sprouts.
In terms of vitamins, sprouts have a lot more of vitamins A, B6, B9, C, E, K, and choline, while spirulina has a little more of vitamins B1, B2, and B3. An easy win for sprouts.
In the category of minerals, sprouts have more calcium, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while spirulina has more copper and iron. Another clear win for sprouts.
Adding up the sections makes the winner very clear: Brussels sprouts enjoy a well-earned victory.
Want to learn more?
You might like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Nanotechnology vs Alcohol Damage!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One Thing That Does Pair Well With Alcohol…
Alcohol is not a healthy thing to consume. That shouldn’t be a controversial statement, but there is a popular belief that it can be good for the heart:
Red Wine & The Heart: Can We Drink To Good Health?
The above is an interesting and well-balanced article that examines the arguments for health benefits (including indirectly, e.g. social aspects).
Ultimately, though, as the World Health Organization puts it:
WHO: No level of alcohol consumption is safe for our health
There is some good news:
We can somewhat reduce the harm done by alcohol by altering our habits slightly:
How To Make Drinking Less Harmful
…and we can also, of course, reduce our alcohol consumption (ideally to zero, but any reduction is an improvement already):
And, saving the best news (in this section, anyway) for last, it is almost always possible to undo the harm done specifically to one’s liver:
Nanotechnology to the rescue?
Remember when we had a main feature about how colloidal gold basically does nothing by itself (and that that’s precisely why gold is used in medicine, when it is used)?
Now it has an extra bit of nothing to do, for our benefit (if we drink alcohol, anyway), as part of a gel that detoxifies alcohol before it can get to our liver:
Gold is one of the “ingredients” in a gel containing a nanotechnology lattice of protein fibrils coated with iron (and the gold is there as an inert catalyst, which is chemistry’s way of saying it doesn’t react in any way but it does cheer the actual reagents on). There’s more chemistry going on than we have room to discuss in our little newsletter, so if you like the full details, you can read about that here:
Single-site iron-anchored amyloid hydrogels as catalytic platforms for alcohol detoxification
The short and oversimplified explanation is that instead of alcohol being absorbed from the gut and transported via the bloodstream to the liver, where it is metabolized (poisoning the liver as it goes, and poisoning the rest of the body too, including the brain), the alcohol is degraded while it is still in the gastrointestinal tract, converted by the gel’s lattice into acetic acid (which is at worst harmless, and actually in moderation a good thing to have).
Even shorter and even more oversimplified: the gel turns the alcohol into vinegar in the stomach and gut, before it can get absorbed into the blood.
But…
Of course there’s a “but”…
There are some limitations:
It doesn’t get it all (tests so far found it only gets about half of the alcohol), and so far it’s only been tested on mice, so it’s not on the market yet—while the researchers are sufficiently confident about it that a patent application has now been made, though, so it’ll probably show up on the market in the near future.
You can read a pop-science article about it (with diagrams!) here:
New gel breaks down alcohol in the body
Want to read more…
…about how to protect your organs (including your brain) from alcohol completely?
We’ve reviewed quite a number of books about quitting alcohol, so it’s hard to narrow it down to a single favorite, but after some deliberation, we’ll finish today with recommending:
Quit Drinking – by Rebecca Dolton ← you can read our review here
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: