Is Unnoticed Environmental Mold Harming Your Health?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Environmental mold can be a lot more than just the famously toxic black mold that sometimes makes the headlines, and many kinds you might not notice, but it can colonizes your sinuses and gut just the same:
Breaking the mold
Around 25% of homes in North America are estimated to have mold, though the actual number is likely to be higher, affecting both older and new homes. For that matter, mold can grow in unexpected areas, like inside air conditioning units, even in dry regions.
If mold just sat where it is minding its own business, it might not be so bad, but instead they release their spores, which are de facto airborne mycotoxins, which can colonize places like the sinuses or gut, causing significant health issues.
Not everyone in the same household is affected the same way by mold due to genetic differences and varying pre-existing health conditions. But as a general rule of thumb, mold inflames the brain, nerves, gut, and skin, and can negatively impact the vagal nerve, which is linked to the gut-brain connection. Mycotoxins also damage mitochondria, leading to symptoms like fatigue, brain fog, and cognitive issues. To complicate matters further, mold illness can mimic other conditions like anxiety, chronic fatigue, fibromyalgia, IBS, and more, making it difficult to diagnose.
Testing is possible, though they all have limitations, e.g:
- Home testing: testing the home for mold spores and mycotoxins is crucial for effective treatment; professional mold remediation companies are a good idea (to do a thorough job of cleaning, without also breathing in half the mold while cleaning it).
- Mold allergy testing: mold allergy testing (IgE testing or skin tests) is often used, but it doesn’t diagnose mold-related illnesses linked to severe symptoms like fatigue or neurodegeneration.
- Serum antibody testing: tests for immune reactions (IgG) to mycotoxins may not always show positive results if the immune system is weakened by long-term exposure.
- Urine mycotoxin testing: urine tests can detect mycotoxins in the body, though are likely to be more expensive, being probably not covered by public health in Canada or insurance in the US.
- Organic acid testing: this urine test can indicate mold colonization in areas like the sinuses or gut. Again, cost/availability may vary, though.
For more information on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Regrow Receding Gums
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One of the problems with the human form is that our teeth evolved to last us for the whole of our life, with plenty of room to spare before our eventual death at the ripe old age of about 35 on average. Dr. Ellie Phillips advises those of us who might be a bit older than that, on how we can avoid becoming “too long in the tooth”—in other words, how to keep our gums, and thus our teeth, in place and healthy.
Getting to the root of the problem
The single biggest cause of gum recession is an acidic environment in the mouth, which harms teeth and gums alike. This acidic environment is produced not merely by consuming acid foods or drinks, but also (and much more often, and more problematically) by sugary foods and drinks, which are not necessarily themselves acidic, but they feed bacteria that release acids as a by-product of their metabolism. If we consume an acidic food or drink, it’s there for a moment, but if we then salivate and/or take a drink of water, it’s pretty much gone in a few seconds. But those bacteria when we feed them sugar? They are there to stay unless we do something more about them than just drink some water.
Other contributing factors to gum recession include teeth grinding, and (ironically) certain oral care products, especially many artificial teeth whiteners.
In case you were wondering: no, brushing will not* generally cause or even worsen gum recession, but flossing can exacerbate it if it’s already underway.
*unless, of course, you are using one of the whiteners we mentioned above
What to do about it: Dr. Phillips recommends:
- use a moderately firm toothbrush to massage gums and promote blood flow
- avoid acidic oral products and homemade remedies even if they’re not acidic but can be caustic, such as baking soda
- rebuild your gums’ and teeth’s protective biofilm (yes, there are “good bacteria” that are supposed to be there) with proper brushing
- avoid cleanings that are more intensive than brushing—skip flossing until your gums have recovered, too
- adjust your diet to avoid acids and (especially) sugars
10almonds note: she also recommends the use of xylitol to promote a healthy oral environment; we don’t recommend that, as while it may be great for the teeth, studies have found it to be bad for the heart.
For more on all of her advices and a bit more of the science of it, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Toothpastes & Mouthwashes: Which Help And Which Harm?
- Flossing Without Flossing?
- Less Common Oral Hygiene Options ← including the miswak “chewing stick”, which even outperformed toothbrushes in clinical trials, by biochemically altering the composition of the saliva while gently cleaning like a toothbrush.
- Fluoride Toothpaste vs Non-Fluoride Toothpaste – Which is Healthier?
- Non-Alcohol Mouthwash vs Alcohol Mouthwash – Which is Healthier?
- Xylitol vs Erythritol – Which is Healthier?
Take care!
Share This Post
-
Indistractable – by Nir Eyal
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Have you ever felt that you could accomplish anything you wanted/needed, if only you didn’t get distracted?
This book lays out a series of psychological interventions for precisely that aim, and it goes a lot beyond the usual “download/delete these apps to help you stop checking social media every 47 seconds”.
Some you’ll have heard of before, some you won’t have, and if even one method works for you, it’ll have been well worth your while reading this book. This reviewer, for example, enjoyed the call to identity-based strength, e.g. adopting an “I am indistractable*” perspective going into tasks. This is akin to the strength of, for example, “I don’t drink” over “I am a recovering alcoholic”.
*the usual spelling of this, by the way, is “undistractable”, but we use the author’s version here for consistency. It’s a great marketing gimmick, as all searches for the word “indistractable” will bring up his book.
Nor is the book just about maximizing productivity to the detriment of everything else; this is not about having a 25 hours per day “grindset”. Rather, it even makes sure to cover such things as focusing on one’s loved ones, for instance.
Bottom line: if you’ve tried blocking out the distractions but still find you can’t focus, this book offers next-level solutions
Click here to check out Indistractible, and become indeed indistractable!
Share This Post
-
Dentists Debunk 15 Teeth Myths
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dentists Dr. John Yoo and Dr. Jason Lin leave no gaps in the truth:
The tooth, the whole tooth, and nothing but the tooth
Not only is there no tooth fairy (we are shocked), but also…
- “Baby teeth aren’t important.”
False! Baby teeth act as space holders for permanent teeth, affect speech development, and influence a child’s psychological well-being. - “Acidic fruits will whiten your smile.”
False! In any practical sense, anyway: acidic fruits may temporarily make teeth appear whiter by dispersing stains but cause enamel erosion and weaken teeth over time. - “Fillings last forever.”
False! Fillings can wear down, fail, or develop cavities underneath if oral hygiene isn’t maintained, requiring replacement over time. - “Cavities are irreversible.”
False! Cavities in the enamel can be reversed with fluoride and good oral hygiene, but cavities that reach the dentin are typically irreversible. - “Braces are just for crooked teeth.”
False! Braces also correct functional issues like overbites, underbites, crossbites, and prevent future complications like tooth impaction. - “A knocked-out tooth is gone for good.”
False! A knocked-out tooth can be reimplanted if done quickly (ideally within an hour); storing it in whole milk or saliva helps preserve it. - “Diet sodas won’t give you cavities.”
False! Diet sodas can still cause cavities due to their acidic pH, which erodes enamel, even without sugar. - “Dental cleanings aren’t necessary.”
False! Dental cleanings help remove plaque and tartar that regular brushing can’t, and allow for regular oral health checkups. - “Retainers aren’t for life.”
False! To maintain teeth alignment after braces, retainers should be worn long-term as teeth can shift even years later. - “You should floss before brushing.”
False! The order doesn’t matter, but do floss regularly. - “Everyone has wisdom teeth.”
False! Not everyone is born with wisdom teeth; they are the most commonly missing teeth, and not everyone needs them removed. - “Hydrogen peroxide and baking soda are good toothpaste replacements.”
False! While they are common components in toothpaste, they lack fluoride, which is essential for remineralizing and protecting enamel. - “You’re too old to get braces.”
False! There’s no age limit for braces or aligners; adults often seek them for both aesthetic and functional reasons. - “Teeth that have had root canals can’t feel.”
False! Teeth with root canals can’t feel pain from nerves, but you can still sense pressure due to surrounding ligaments. - “You’ll inevitably lose all your teeth when you’re old.”
False! Good oral hygiene and regular dental care can preserve natural teeth into old age, though genetics also play a role.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
- “Baby teeth aren’t important.”
Related Posts
-
Why You Probably Need More Sleep
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sleep: yes, you really do still need it!
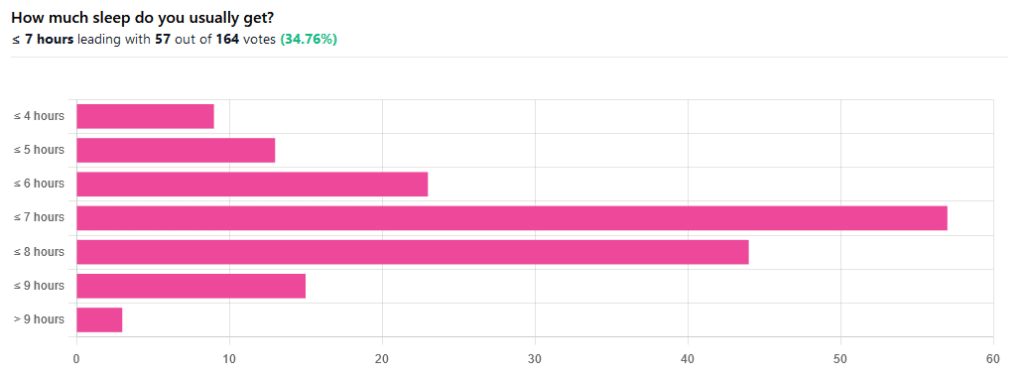
We asked you how much sleep you usually get, and got the above-pictured, below-described set of responses:
- A little of a third of all respondents selected the option “< 7 hours”
- However, because respondents also selected options such as < 6 hours, < 5 hours, and < 4 hours, so if we include those in the tally, the actual total percentage of respondents who reported getting under 7 hours, is actually more like 62%, or just under two thirds of all respondents.
- Nine respondents, which was about 5% of the total, reported usually getting under 4 hours sleep
- A little over quarter of respondents reported usually getting between 7 and 8 hours sleep
- Fifteen respondents, which was a little under 10% of the total, reported usually getting between 8 and 9 hours of sleep
- Three respondents, which was a little under 2% of the total, reported getting over 9 hours of sleep
- In terms of the classic “you should get 7–9 hours sleep”, approximately a third of respondents reported getting this amount.
You need to get 7–9 hours sleep: True or False?
True! Unless you have a (rare!) mutated ADRB1 gene, which reduces that.
The way to know whether you have this, without genomic testing to know for sure, is: do you regularly get under 6.5 hours sleep, and yet continue to go through life bright-eyed and bushy-tailed? If so, you probably have that gene. If you experience daytime fatigue, brain fog, and restlessness, you probably don’t.
About that mutated ADRB1 gene:
NIH | Gene identified in people who need little sleep
Quality of sleep matters as much as duration, and a lot of studies use the “RU-Sated” framework, which assesses six key dimensions of sleep that have been consistently associated with better health outcomes. These are:
- regularity / usual hours
- satisfaction with sleep
- alertness during waking hours
- timing of sleep
- efficiency of sleep
- duration of sleep
But, that doesn’t mean that you can skimp on the last one if the others are in order. In fact, getting a good 7 hours sleep can reduce your risk of getting a cold by three or four times (compared with six or fewer hours):
Behaviorally Assessed Sleep and Susceptibility to the Common Cold
^This study was about the common cold, but you may be aware there are more serious respiratory viruses freely available, and you don’t want those, either.
Napping is good for the health: True or False?
True or False, depending on how you’re doing it!
If you’re trying to do it to sleep less in total (per polyphasic sleep scheduling), then no, this will not work in any sustainable fashion and will be ruinous to the health. We did a Mythbusting Friday special on specifically this, a while back:
Could Just Two Hours Sleep Per Day Be Enough?
PS: you might remember Betteridge’s Law of Headlines
If you’re doing it as a energy-boosting supplement to a reasonable night’s sleep, napping can indeed be beneficial to the health, and can give benefits such as:
- Increased alertness
- Helps with learning
- Improved memory
- Boost to immunity
- Enhance athletic performance
However! There is still a right and a wrong way to go about it, and we wrote about this previously, for a Saturday Life Hacks edition of 10almonds:
How To Nap Like A Pro (No More “Sleep Hangovers”!)
As we get older, we need less sleep: True or False
False, with one small caveat.
The small caveat: children and adolescents need 9–12 hours sleep because, uncredited as it goes, they are doing some seriously impressive bodybuilding, and that is exhausting to the body. So, an adult (with a normal lifestyle, who is not a bodybuilder) will tend to need less sleep than a child/adolescent.
But, the statement “As we get older, we need less sleep” is generally taken to mean “People in the 65+ age bracket need less sleep than younger adults”, and this popular myth is based on anecdotal observational evidence: older people tend to sleep less (as our survey above shows! For any who aren’t aware, our readership is heavily weighted towards the 60+ demographic), and still continue functioning, after all.
Just because we survive something with a degree of resilience doesn’t mean it’s good for us.
In fact, there can be serious health risks from not getting enough sleep in later years, for example:
Sleep deficiency promotes Alzheimer’s disease development and progression
Want to get better sleep?
What gets measured, gets done. Sleep tracking apps can be a really good tool for getting one’s sleep on a healthier track. We compared and contrasted some popular ones:
The Head-To-Head Of Google and Apple’s Top Apps For Getting Your Head Down
Take good care of yourself!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Worst Cookware Lurking In Your Kitchen (Toxicologist Explains)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Yvonne Burkart gives us a rundown of the worst offenders, and what to use instead:
Hot mess
The very worst offender is non-stick cookware, the kind with materials such as Teflon. These are the most toxic, due to PFAS chemicals.
Non-stick pans release toxic gases, leach chemicals into food, and release microplastic particles, which can accumulate in the body.
One that a lot of people don’t think about, in that category, is the humble air-fryer, which often as not has a non-stick cooking “basket”. These she describes as highly toxic, as they combine plastic, non-stick coatings, and high heat, which can release fumes and other potentially dangerous chemicals into the air and food.
You may be wondering: how bad is it? And the answer is, quite bad. PFAS chemicals are linked to infertility, hypertension in pregnancy, developmental issues in children, cancer, weakened immune systems, hormonal disruption, obesity, and intestinal inflammation.
Dr. Burkart’s top picks for doing better:
- Pure ceramic cookware: top choice for safety, particularly brands like Xtrema, which are tested for heavy metal leaching.
- Carbon steel & cast iron: durable and safe; can leach iron in acidic foods (for most people, this is a plus, but some may need to be aware of it)
- Stainless steel: lightweight and affordable but can leach nickel and chromium in acidic foods at high temperatures. Use only if nothing better is available.
And specifically as alternatives to air-fryers: glass convection ovens or stainless steel ovens are safer than conventional air fryers. The old “combination oven” can often be a good choice here.
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- PFAS Exposure & Cancer: The Numbers Are High
- It’s Not Fantastic To Be Plastic ← for the closely related topic of microplastics and nanoplastics
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Get Well, Stay Well – by Dr. Gemma Newman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Gemma Newman is a GP (British equivalent of what in America is called a “family doctor”) who realized she was functioning great as a diagnostic flowchart interpreter and pill dispensary, but not actually doing much of what she got into the job to do: helping people.
Her patients were getting plenty of treatments, but not getting better. Often, they were getting worse. And she knew why: they come in for treatment for one medical problem, when they have six and a half medical problems probably a stack of non-medical problems that contributed to them,
So, this book sets out to do what she tries to do in her office, but often doesn’t have the time: treat the whole person.
In it, she details what areas of life to look at, what things are most likely to contribute to wellness/unwellness (be those things completely in your power or not), and how to—bit by bit—make all the parts better, and keep them that way.
The writing style is conversational, and while it’s heavily informed by her professional competence, there’s no arcane science here; it’s more about the system of bringing everything together harmoniously.
Bottom line: if you think there’s more to wellness than can be represented on an annual physicals chart, then this is the book to help you get/keep on top of things.
Click here to check out Get Well, Stay Well, and do just that!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: