Ovarian cancer is hard to detect. Focusing on these 4 symptoms can help with diagnosis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ovarian cancers are often found when they are already advanced and hard to treat.
Researchers have long believed this was because women first experienced symptoms when ovarian cancer was already well-established. Symptoms can also be hard to identify as they’re vague and similar to other conditions.
But a new study shows promising signs ovarian cancer can be detected in its early stages. The study targeted women with four specific symptoms – bloating, abdominal pain, needing to pee frequently, and feeling full quickly – and put them on a fast track to see a specialist.
As a result, even the most aggressive forms of ovarian cancer could be detected in their early stages.
So what did the study find? And what could it mean for detecting – and treating – ovarian cancer more quickly?

Why is ovarian cancer hard to detect early?
Ovarian cancer cannot be detected via cervical cancer screening (which used to be called a pap smear) and pelvic exams aren’t useful as a screening test.
Current Australian guidelines recommend women get tested for ovarian cancer if they have symptoms for more than a month. But many of the symptoms – such as tiredness, constipation and changes in menstruation – are vague and overlap with other common illnesses.
This makes early detection a challenge. But it is crucial – a woman’s chances of surviving ovarian cancer are associated with how advanced the cancer is when she is diagnosed.
If the cancer is still confined to the original site with no spread, the five-year survival rate is 92%. But over half of women diagnosed with ovarian cancer first present when the cancer has already metastatised, meaning it has spread to other parts of the body.
If the cancer has spread to nearby lymph nodes, the survival rate is reduced to 72%. If the cancer has already metastasised and spread to distant sites at the time of diagnosis, the rate is only 31%.
There are mixed findings on whether detecting ovarian cancer earlier leads to better survival rates. For example, a trial in the UK that screened more than 200,000 women failed to reduce deaths.
That study screened the general public, rather than relying on self-reported symptoms. The new study suggests asking women to look for specific symptoms can lead to earlier diagnosis, meaning treatment can start more quickly.
What did the new study look at?
Between June 2015 and July 2022, the researchers recruited 2,596 women aged between 16 and 90 from 24 hospitals across the UK.
They were asked to monitor for these four symptoms:
- persistent abdominal distension (women often refer to this as bloating)
- feeling full shortly after starting to eat and/or loss of appetite
- pelvic or abdominal pain (which can feel like indigestion)
- needing to urinate urgently or more often.
Women who reported at least one of four symptoms persistently or frequently were put on a fast-track pathway. That means they were sent to see a gynaecologist within two weeks. The fast track pathway has been used in the UK since 2011, but is not specifically part of Australia’s guidelines.
Some 1,741 participants were put on this fast track. First, they did a blood test that measured the cancer antigen 125 (CA125). If a woman’s CA125 level was abnormal, she was sent to do a internal vaginal ultrasound.
What did they find?
The study indicates this process is better at detecting ovarian cancer than general screening of people who don’t have symptoms. Some 12% of women on the fast-track pathway were diagnosed with some kind of ovarian cancer.
A total of 6.8% of fast-tracked patients were diagnosed with high-grade serous ovarian cancer. It is the most aggressive form of cancer and responsible for 90% of ovarian cancer deaths.
Out of those women with the most aggressive form, one in four were diagnosed when the cancer was still in its early stages. That is important because it allowed treatment of the most lethal cancer before it had spread significantly through the body.
There were some promising signs in treating those with this aggressive form. The majority (95%) had surgery and three quarters (77%) had chemotherapy. Complete cytoreduction – meaning all of the cancer appears to have been removed – was achieved in six women out of ten (61%).
It’s a promising sign that there may be ways to “catch” and target ovarian cancer before it is well-established in the body.
What does this mean for detection?
The study’s findings suggest this method of early testing and referral for the symptoms leads to earlier detection of ovarian cancer. This may also improve outcomes, although the study did not track survival rates.
It also points to the importance of public awareness about symptoms.
Clinicians should be able to recognise all of the ways ovarian cancer can present, including vague symptoms like general fatigue.
But empowering members of the general public to recognise a narrower set of four symptoms can help trigger testing, detection and treatment of ovarian cancer earlier than we thought.
This could also save GPs advising every woman who has general tiredness or constipation to undergo an ovarian cancer test, making testing and treatment more targeted and efficient.
Many women remain unaware of the symptoms of ovarian cancer. This study shows recognising them may help early detection and treatment.
Jenny Doust, Clinical Professorial Research Fellow, Australian Women and Girls’ Health Research Centre, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What’s in the supplements that claim to help you cut down on bathroom breaks? And do they work?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
With one in four Australian adults experiencing problems with incontinence, some people look to supplements for relief.
With ingredients such as pumpkin seed oil and soybean extract, a range of products promise relief from frequent bathroom trips.
But do they really work? Let’s sift through the claims and see what the science says about their efficacy.
Christian Moro/Shutterstock What is incontinence?
Incontinence is the involuntary loss of bladder or bowel control, leading to the unintentional leakage of urine or faeces. It can range from occasional minor leaks to a complete inability to control urination and defecation.
This condition can significantly impact daily activities and quality of life, and affects women more often than it affects men.
Some people don’t experience bladder leakage but can sometimes feel an urgent need to go to the bathroom. This is known as overactive bladder syndrome, and occurs when the muscles around the bladder tighten on their own, which greatly reduces its capacity. The result is the person feels the need to go to the bathroom much more frequently.
There are many potential causes of incontinence and overactive bladders, including menopause, pregnancy and child birth, urinary tract infections, pelvic floor disorders, and an enlarged prostate. Conditions such as diabetes, neurological disorders and certain medications (such as diuretics, sleeping pills, antidepressants and blood-pressure drugs) can also contribute.
While pelvic muscle rehabilitation and behavioural techniques for bladder retraining can be helpful, some people are interested in pharmaceutical solutions.
What’s in these products?
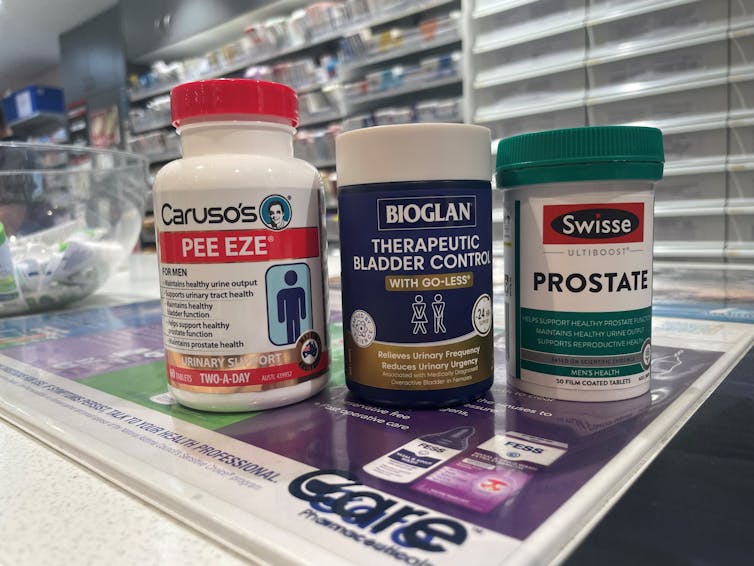
A number of supplements are available in Australia that include ingredients used in traditional medicine for urinary incontinence and overactive bladders. The three most common ingredients are:
- Cucurbita pepo (pumpkin seed extract)
- glycine max (soybean extract)
- an extract from the bark of the Crateva magna or nurvala (Varuna) tree.
The supplements have common ingredients. Author How are they supposed to work?
Pumpkin seeds are rich in plant sterols that are thought to reduce the testosterone-related enlargement of the prostate, as well as having broader anti-inflammatory effects. The seed extracts can also contain oleic acid, which may help increase bladder capacity by relaxing the muscles around the organ.
Soybean extracts are rich in isoflavones, especially daidzen and genistein. Like olieic acid, these are thought to act on the muscles around the bladder. Because isoflavones are similar in structure to the female hormone oestrogen, soy extracts may be most beneficial for postmenopausal women who have overactive bladders.
Crateva extract is rich in lupeol- and sterol-based chemicals which have strong anti-inflammatory effects. This has benefits not just for enlarged prostates but possibly also for reducing urinary tract infections.
Do they actually work?
It’s important to note that the government has only approved these types of supplements as “listed medicines”. This means the ingredients have only been assessed for safety. The companies behind the products have not had to provide evidence they actually work.
A 2014 clinical trial examined a combined pumpkin seed and soybean extract called cucurflavone on people with overactive bladders. The 120 participants received either a placebo or a daily 1,000mg dose of the herbal mixture over a period of 12 weeks.
By the end of study, those in the cucurflavone group went to the bathroom around three fewer times per day, compared with people in the control group, who only went to the bathroom on average one fewer time each day.
In a different trial, researchers examined a combination of Crateva bark extract with herbal extracts of horsetail and Japanese evergreen spicebush, called Urox.
For the 150 participants, the Urox formulation helped participants go to the bathroom less frequently when compared with placebo treatment.
After eight weeks of treatment, participants in the placebo group were going to the bathroom to urinate 11 times per day. Those in the Urox group were only going around to 7.5 times per day. And those who took Urox also needed to go to the bathroom one fewer time during the night.
Finally, another study also examined a Creteva, horsetail and Japanese spicebush combination, but this time in children. They were given either a 420mg dose of the supplement or a placebo, and then monitored for how many times they wet the bed.
After two months of taking the supplement, slightly more than 40% of the 24 kids in the supplement group wet the bed less often.
While these results may look promising, there are considerable limitations to the studies which means the data may not be reliable. For example, the trials didn’t include enough participants to have reliable data. To conclusively provide efficacy, final-stage clinical trials require data for between 300 and 3,000 patients.
From the studies, it is also not clear whether some participants were also taking other medicines as well as the supplement. This is important, as medications can interfere with how the supplements work, potentially making them less or more effective.
What if you want to take them?
If you have incontinence or an overactive bladder, you should always discuss this with your doctor, as it may due to a serious or treatable underlying condition.
Otherwise, your GP may give you strategies or exercises to improve your bladder control, prescribe medications or devices, or refer you to a specialist.
If you do decide to take a supplement, discuss this with your doctor and local pharmacist so they can check that any product you choose will not interfere with any other medications you may be taking.
Nial Wheate, Professor of Pharmaceutical Chemistry, Macquarie University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Is thirst a good predictor of dehydration?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Water is essential for daily functioning and health, and we can only survive a few days without it. Yet we constantly lose water through sweat, urination and even evaporation when we breathe.
This is why we have evolved a way to regulate and maintain water in our bodies. Like other animals, our survival relies on a strong biological drive that tells us to find and drink water to balance fluid loss.
This is thirst – a sensation of dryness in the mouth signalling we need to have a drink. This basic physiological mechanism is controlled mainly by part of the brain’s “control centre”, called the hypothalamus. The hypothalamus receives signals from various regions of the body and in return, releases hormones that act as a messenger to signal the thirst sensation.
KieferPix/Shutterstock What is dehydration?
Staying hydrated (having enough water in our bodies) is important for several reasons, including:
- regulating body temperature through sweat and respiration
- lubricating joints and eyes
- preventing infections
- digesting and absorbing nutrients
- flushing out waste (via the kidneys)
- preventing constipation
- brain function (including memory and concentration)
- mood and energy levels
- physical performance and recovery from exercise
- skin health.
Dehydration occurs when our body doesn’t have enough water. Even slight drops in fluid levels have noticeable consequences, such as headaches, feeling dizzy, lethargy and struggling to concentrate.
Chronic dehydration can pose more serious health risks, including urinary tract infections, constipation and kidney stones.
What does the evidence say?
Despite thirst being one of the most basic biological drivers for good hydration, science suggests our feelings of thirst and subsequent fluid intake don’t always correlate with hydration levels.
For example, a recent study explored the impact of thirst on fluid intake and hydration status. Participants attended a lab in the morning and then later in the afternoon to provide markers of hydration status (such as urine, blood samples and body weight). The relationship between levels of thirst in the morning and afternoon hydration status was negligible.
Further, thirst may be driven by environmental factors, such as access to water. For example, one study looked at whether ample access to water in a lab influenced how much people drank and how hydrated they were. The link between how thirsty they felt and how hydrated they were was weak, suggesting the availability of water influenced their fluid intake more than thirst.
Exercise can also change our thirst mechanism, though studies are limited at this stage.
Being thirsty doesn’t necessarily mean we’re dehydrated. puhhha/Shutterstock Interestingly, research shows women experience thirst more strongly than men, regardless of hydration status. To understand gender differences in thirst, researchers infused men and women with fluids and then measured their thirst and how hydrated they were. They found women generally reported thirst at a lower level of fluid loss. Women have also been found to respond more to feeling thirsty by drinking more water.
Other ways to tell if you need to drink some water
While acknowledging some people will need to drink more or less, for many people, eight cups (or two litres) a day is a good amount of water to aim for.
But beyond thirst, there are many other ways to tell whether you might need to drink more water.
1. urine colour: pale yellow urine typically indicates good hydration, while darker, concentrated urine suggests dehydration
2. frequency of going to the toilet: urinating regularly (around four to six times a day) indicates good hydration. Infrequent urination can signal dehydration
3. skin turgor test: gently pinching the skin (for example, on the back of the hand) and observing how quickly the skin returns to its normal position can help assess hydration. Slow return may indicate dehydration
If skin stays elevated after pinching it may be a sign of dehydration. SusaZoom/Shutterstock 4. mouth and lips: a dry mouth or cracked lips can be early signs of dehydration
5. headaches and fatigue: frequent headaches, dizziness, or unexplained fatigue can be signs of inadequate hydration
6. sweating: in physically active people, monitoring how much they sweat during activity can help estimate fluid loss and hydration needs. Higher levels of sweat may predispose a person to dehydration if they are unable to replace the fluid lost through water intake
These indicators, used together, provide a more comprehensive picture of hydration without solely depending on the sensation of thirst.
Of course, if you do feel thirsty, it’s still a good idea to drink some water.
Lauren Ball, Professor of Community Health and Wellbeing, The University of Queensland and Kiara Too, PhD candidate, School of Human Movement and Nutrition Sciences, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
How To Leverage Attachment Theory In Your Relationship
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Leverage Attachment Theory In Your Relationship
Attachment theory has come to be seen in “kids nowadays”’ TikTok circles as almost a sort of astrology, but that’s not what it was intended for, and there’s really nothing esoteric about it.
What it can be, is a (fairly simple, but) powerful tool to understand about our relationships with each other.
To demystify it, let’s start with a little history…
Attachment theory was conceived by developmental psychologist Mary Ainsworth, and popularized as a theory bypsychiatrist John Bowlby. The two would later become research partners.
- Dr. Ainsworth’s initial work focused on children having different attachment styles when it came to their caregivers: secure, avoidant, or anxious.
- Later, she would add a fourth attachment style: disorganized, and then subdivisions, such as anxious-avoidant and dismissive-avoidant.
- Much later, the theory would be extended to attachments in (and between) adults.
What does it all mean?
To understand this, we must first talk about “The Strange Situation”.
“The Strange Situation” was an experiment conducted by Dr. Ainsworth, in which a child would be observed playing, while caregivers and strangers would periodically arrive and leave, recreating a natural environment of most children’s lives. Each child’s different reactions were recorded, especially noting:
- The child’s reaction (if any) to their caregiver’s departure
- The child’s reaction (if any) to the stranger’s presence
- The child’s reaction (if any) to their caregiver’s return
- The child’s behavior on play, specifically, how much or little the child explored and played with new toys
She observed different attachment styles, including:
- Secure: a securely attached child would play freely, using the caregiver as a secure base from which to explore. Will engage with the stranger when the caregiver is also present. May become upset when the caregiver leaves, and happy when they return.
- Avoidant: an avoidantly attached child will not explore much regardless of who is there; will not care much when the caregiver departs or returns.
- Anxious: an anxiously attached child may be clingy before separation, helplessly passive when the caregiver is absent, and difficult to comfort upon the caregiver’s return.
- Disorganized: a disorganizedly attached child may flit between the above types
These attachment styles were generally reflective of the parenting styles of the respective caregivers:
- If a caregiver was reliably present (physically and emotionally), the child would learn to expect that and feel secure about it.
- If a caregiver was absent a lot (physically and/or emotionally), the child would learn to give up on expecting a caregiver to give care.
- If a caregiver was unpredictable a lot in presence (physical and/or emotional), the child would become anxious and/or confused about whether the caregiver would give care.
What does this mean for us as adults?
As we learn when we are children, tends to go for us in life. We can change, but we usually don’t. And while we (usually) no longer rely on caregivers per se as adults, we do rely (or not!) on our partners, friends, and so forth. Let’s look at it in terms of partners:
- A securely attached adult will trust that their partner loves them and will be there for them if necessary. They may miss their partner when absent, but won’t be anxious about it and will look forward to their return.
- An avoidantly attached adult will not assume their partner’s love, and will feel their partner might let them down at any time. To protect themself, they may try to manage their own expectations, and strive always to keep their independence, to make sure that if the worst happens, they’ll still be ok by themself.
- An anxiously attached adult will tend towards clinginess, and try to keep their partner’s attention and commitment by any means necessary.
Which means…
- When both partners have secure attachment styles, most things go swimmingly, and indeed, securely attached partners most often end up with each other.
- A very common pairing, however, is one anxious partner dating one avoidant partner. This happens because the avoidant partner looks like a tower of strength, which the anxious partner needs. The anxious partner’s clinginess can also help the avoidant partner feel better about themself (bearing in mind, the avoidant partner almost certainly grew up feeling deeply unwanted).
- Anxious-anxious pairings happen less because anxiously attached people don’t tend to be attracted to people who are in the same boat.
- Avoidant-avoidant pairings happen least of all, because avoidantly attached people having nothing to bind them together. Iff they even get together in the first place, then later when trouble hits, one will propose breaking up, and the other will say “ok, bye”.
This is fascinating, but is there a practical use for this knowledge?
Yes! Understanding our own attachment styles, and those around us, helps us understand why we/they act a certain way, and realize what relational need is or isn’t being met, and react accordingly.
That sometimes, an anxiously attached person just needs some reassurance:
- “I love you”
- “I miss you”
- “I look forward to seeing you later”
That sometimes, an avoidantly attached person needs exactly the right amount of space:
- Give them too little space, and they will feel their independence slipping, and yearn to break free
- Give them too much space, and oops, they’re gone now
Maybe you’re reading that and thinking “won’t that make their anxious partner anxious?” and yes, yes it will. That’s why the avoidant partner needs to skip back up and remember to do the reassurance.
It helps also when either partner is going to be away (physically or emotionally! This counts the same for if a partner will just be preoccupied for a while), that they parameter that, for example:
- Not: “Don’t worry, I just need some space for now, that’s all” (à la “I am just going outside and may be some time“)
- But: “I need to be undisturbed for a bit, but let’s schedule some me-and-you-time for [specific scheduled time]”.
Want to learn more about addressing attachment issues?
Psychology Today: Ten Ways to Heal Your Attachment Issues
You also might enjoy such articles such as:
- Nurturing secure attachment: building healthy relationships
- Why anxious and avoidant often attracted each other
- How to help an insecurely attached partner feel loved
- How to cope with a dismissive-avoidant partner
Lastly, to end on a light note…
Share This Post
Related Posts
-
Unlock Your Flexibility With These 4 New Stretches
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
People often stick to the same few stretches, which may limit flexibility progress, especially as the most common stretches often miss deeper, harder-to-reach areas.
So, here are some new (well, probably new to most people, at least) stretches that can get things moving in different directions:
Diversity Continues To Be Good!
The stretches are:
90/90 Hip stretch with a twist:
- Sit with your knees forming 90° angles; add an arm bar and twist your chest upward.
- Hold for 5 deep breaths and repeat.
- This one targets top glute muscles and quadratus lumborum in the lower back.
Shoulder mobility stretch using a wall:
- Kneel in front of a wall with your forearms placed shoulder-width apart, hands turned outward.
- Lift your hips, push your chest toward your legs, and use the wall and your body weight for deeper leverage.
- This one targets multiple shoulder and rotator cuff muscles through external rotation.
Quad stretch using body weight:
- Sit with your feet hip-width apart, lift your hips, step one foot back, and tuck in your tailbone.
- Focus on pointing your knee down and forward for a deep quad stretch.
- This one targets all four quad muscles, hip flexors, plantar fascia, and opens chest/shoulders.
Chicken wing stretch for upper back:
- Sit with bent knees, place the back of one hand on your waist (chicken wing position).
- Tuck the “wing” into the inner thigh, press your knee inward while resisting with the arm.
- This one broadens the shoulder blade and stretches rear shoulder/upper back muscles; it’s particularly effective for reaching difficult upper back areas not typically stretched.
For more on each of these plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Yoga Teacher: “If I wanted to get flexible in 2025, here’s what I’d do”
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Maca Root’s Benefits For The Mood And The Ability
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Maca Root: What It Does And Doesn’t Do
Maca root, or Lepidium meyenii, gets thought of as a root vegetable, though it’s in fact a cruciferous vegetable and more closely related to cabbage—notwithstanding that it also gets called “Peruvian ginseng”.
- Nutritionally, it’s full of all manner of nutrients (vitamins, minerals, fiber, and a wide array of phytochemicals)
- Medicinally, it’s long enjoyed traditional use against a wide variety of illnesses, including respiratory infections and inflammatory diseases.
It’s also traditionally an aphrodisiac.
Is it really anti-inflammatory?
Probably not… Unless fermented. This hasn’t been studied deeply, but a 2023 study found that non-fermented and fermented maca root extracts had opposite effects in this regard:
However, this was an in vitro study, so we can’t say for sure that the results will carry over to humans.
Is it really an aphrodisiac?
Actually yes, it seems so. Here’s a study in which 45 women with antidepressant-induced sexual dysfunction found it significantly improved both libido and sexual function:
❝In summary, maca root may alleviate antidepressant-induced sexual dysfunction as women age, particularly in the domain of orgasm❞
~ Dr. Christina Dording et al.
Read in full: A Double-Blind Placebo-Controlled Trial of Maca Root as Treatment for Antidepressant-Induced Sexual Dysfunction in Women
As for men, well these mice (not technically men) found it beneficial too:
Effects of combined extracts of Lepidium meyenii and Allium tuberosum Rottl. on [e-word] dysfunction
(pardon the censorship; we’re trying to avoid people’s spam filters)
It did also improve fertility (and, actually in real men this time):
Does Lepidium meyenii (Maca) improve seminal quality?
Oh, to be in the mood
Here’s an interesting study in which 3g/day yielded significant mood improvement in these 175 (human) subjects:
And yes, it was found to be “well-tolerated” which is scientist-speak for “this appears to be completely safe, but we don’t want to commit ourselves to an absolutist statement and we can’t prove a negative”.
Oh, to have the energy
As it turns out, maca root does also offer benefits in this regard too:
(that’s not an added ingredient; it’s just a relevant chemical that the root naturally contains)
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Managing Jealousy
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Jealousy is often thought of as a young people’s affliction, but it can affect us at any age—whether we are the one being jealous, or perhaps a partner.
And, the “green-eyed monster” can really ruin a lot of things; relationships, friendships, general happiness, physical health even (per stress and anxiety and bad sleep), and more.
The thing is, jealousy looks like one thing, but is actually mostly another.
Jealousy is a Scooby-Doo villain
That is to say: we can unmask it and see what much less threatening thing is underneath. Which is usually nothing more nor less than: insecurities
- Insecurity about losing one’s partner
- Insecurity about not being good enough
- Insecurity about looking bad socially
…etc. The latter, by the way, is usually the case when one’s partner is socially considered to be giving cause for jealousy, but the primary concern is not actually relational loss or any kind of infidelity, but rather, looking like one cannot keep one’s partner’s full attention romantically/sexually. This drives a lot of people to act on jealousy for the sake of appearances, in situations where they might otherwise, if they didn’t feel like they’d be adversely judged for it, be considerably more chill.
Thus, while monogamy certainly has its fine merits, there can also be a kind of “toxic monogamy” at hand, where a relationship becomes unhealthy because one partner is just trying to live up to social expectations of keeping the other partner in check.
This, by the way, is something that people in polyamorous and/or open relationships typically handle quite neatly, even if a lot of the following still applies. But today, we’re making the statistically safe assumption of a monogamous relationship, and talking about that!
How to deal with the social aspect
If you sit down with your partner and work out in advance the acceptable parameters of your relationship, you’ll be ahead of most people already. For example…
- What counts as cheating? Is it all and any sex acts with all and any people? If not, where’s the line?
- What about kissing? What about touching other body parts? If there are boundaries that are important to you, talk about them. Nothing is “too obvious” because it’s astonishing how many times it will happen that later someone says (in good faith or not), “but I thought…”
- What about being seen in various states of undress? Or seeing other people in various states of undress?
- Is meaningless flirting between friends ok, and if so, how do we draw the line with regard to what is meaningless? And how are we defining flirting, for that matter? Talk about it and ensure you are both on the same page.
- If a third party is possibly making moves on one of us under the guise of “just being friendly”, where and how do we draw the line between friendliness and romantic/sexual advances? What’s the difference between a lunch date with a friend and a romantic meal out for two, and how can we define the difference in a way that doesn’t rely on subjective “well I didn’t think it was romantic”?
If all this seems like a lot of work, please bear in mind, it’s a lot more fun to cover this cheerfully as a fun couple exercise in advance, than it is to argue about it after the fact!
See also: Boundary-Setting Beyond “No”
How to deal with the more intrinsic insecurities
For example, when jealousy is a sign of a partner fearing not being good enough, not measuring up, or perhaps even losing their partner.
The key here might not shock you: communication
Specifically, reassurance. But critically, the correct reassurance!
A partner who is jealous will often seek the wrong reassurance, for example wanting to read their partner’s messages on their phone, or things like that. And while a natural desire when experiencing jealousy, it’s not actually helpful. Because while incriminating messages could confirm infidelity, it’s impossible to prove a negative, and if nothing incriminating is found, the jealous partner can just go on fearing the worst regardless. After all, their partner could have a burner phone somewhere, or a hidden app for cheating, or something else like that. So, no reassurance can ever be given/gained by such requests (which can also become unpleasantly controlling, which hopefully nobody wants).
A quick note on “if you have nothing to fear, you have nothing to hide”: rhetorically that works, but practically it doesn’t.
Writer’s example: when my late partner and I formalized our relationship, we discussed boundaries, and I expressed “so far as I am concerned, I have no secrets from you, except secrets that are not mine to share. For example, if someone has confided in me and asked that I not share it, I won’t. Aside from that, you have access-all-areas in my life; me being yours has its privileges” and this policy itself would already pre-empt any desire to read my messages.
Now indeed, I had nothing to hide. I am by character devoted to a fault. But my friends may well sometimes have things they don’t want me to share, which made that a necessary boundary to highlight (which my partner, an absolute angel by the way and not prone to unhealthy manifestations of jealousy in any case, understood completely).
So, it is best if the partner of a jealous person can explain the above principles as necessary, and offer the correct reassurance instead. Which could be any number of things, but for example:
- I am yours, and nobody else has a chance
- I fully intend to stay with you for life
- You are the best partner I have ever had
- Being with you makes my life so much better
…etc. Note that none of these are “you don’t have to worry about so-and-so”, or “I am not cheating on you”, etc, because it’s about yours and your partner’s relationship. If they ask for reassurances with regard to other people or activities, by all means state them as appropriate, but try to keep the focus on you two.
And if your partner (or you, if it’s you who’s jealous) can express the insecurity in the format…
“I’m afraid of _____ because _____”
…then the “because” will allow for much more specific reassurance. We all have insecurities, we all have reasons we might fear not being good enough for our partner, or losing their affection, and the best thing we can do is choose to trust our partners at least enough to discuss those fears openly with each other.
See also: Save Time With Better Communication ← this can avoid a lot of time-consuming arguments
What about if the insecurity is based in something demonstrably correct?
By this we mean, something like a prior history of cheating, or other reasons for trust issues. In such a case, the jealous partner may well have a reason for their jealousy that isn’t based on a personal insecurity.
In our previous article about boundaries, we talked about relationships (romantic or otherwise) having a “price of entry”. In this case, you each have a “price of entry”:
- The “price of entry” to being with the person who has previously cheated (or similar), is being able to accept that.
- And for the person who cheated (or similar), very likely their partner will have the “price of entry” of “don’t do that again, and also meanwhile accept in good grace that I might be jittery about it”.
And, if the betrayal of trust was something that happened between the current partners in the current relationship, most likely that was also traumatic for the person whose trust was betrayed. Many people in that situation find that trust can indeed be rebuilt, but slowly, and the pain itself may also need treatment (such as therapy and/or couples therapy specifically).
See also: Relationships: When To Stick It Out & When To Call It Quits ← this covers both sides
And finally, to finish on a happy note:
Only One Kind Of Relationship Promotes Longevity This Much!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: