HRT Side Effects & Troubleshooting
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.

This is Dr. Heather Hirsch. She’s a board-certified internist, and her clinical expertise focuses on women’s health, particularly in midlife and menopause, and its intersection with chronic diseases (ranging from things associated with sexual health, to things like osteoporosis and heart disease).
So, what does she want us to know?
HRT can be life-changingly positive, but it can be a shaky start
Hormone Replacement Therapy (HRT), and in this context she’s talking specifically about the most common kind, Menopausal Hormone Therapy (MHT), involves taking hormones that our body isn’t producing enough of.
If these are “bioidentical hormones” as used in most of the industrialized world and increasingly also in N. America, then this is by definition a supplement rather than a drug, for what it’s worth, whereas some non-bioidentical hormones (or hormone analogs, which by definition function similarly to hormones but aren’t the same thing) can function more like drugs.
We wrote a little about his previously:
Hormone Replacement Therapy: A Tale Of Two Approaches
For most people most of the time, bioidentical hormones are very much the best way to go, as they are not only more effective, but also have fewer side effects.
That said, even bioidentical hormones can have some undesired effects, so, how to deal with those?
Don’t worry; bleed happy
A reprise of (usually quite light) menstrual bleeding is the most common side effect of menopausal HRT.
This happens because estrogen affects* the uterus, leading to a build-up and shedding of the uterine lining.
*if you do not have a uterus, estrogen can effect uterine tissue. That’s not a typo—here we mean the verb “effect”, as in “cause to be”. It will not grow a new uterus, but it can cause some clumps of uterine tissue to appear; this means that it becomes possible to get endometriosis without having a uterus. This information should not be too shocking, as endometriosis is a matter of uterine tissue growing inconveniently, often in places where it shouldn’t, and sometimes quite far from the uterus (if present, or its usual location, if absent). However, the risk of this happening is far lower than if you actually have a uterus:
What you need to know about endometriosis
Back to “you have a uterus and it’s making you wish you didn’t”:
This bleeding should, however, be light. It’ll probably be oriented around a 28-day cycle even if you are taking your hormones at the same dose every day of the month, and the bleeding will probably taper off after about 6 months of this.
If the bleeding is heavier, all the time, or persists longer than 6 months, then speak to your gynecologist about it. Any of those three; it doesn’t have to be all three!
Bleeding outside of one’s normal cycle can be caused by anything from fibroids to cancer; statistically speaking it’s probably nothing too dire,but when your safety is in question, don’t bet on “probably”, and do get it checked out:
When A Period Is Very Late (i.e., Post-Menopause)
Dr. Hirsch recommends, as possible remedies to try (preferably under your gynecologist’s supervision):
- lowering your estrogen dose
- increasing your progesterone dose
- taking progesterone continuously instead of cyclically
And if you’re not taking progesterone, here’s why you might want to consider taking this important hormone that works with estrogen to do good things, and against estrogen to rein in some of estrogen’s less convenient things:
Progesterone Menopausal HRT: When, Why, And How To Benefit
(the above link contains, as well as textual information, an explanatory video from Dr. Hirsch herself)
Get the best of the breast
Calm your tits. Soothe your boobs. Destress your breasts. Hakuna your tatas. Undo the calamity beleaguering your mammaries.
Ok, more seriously…
Breast tenderness is another very common symptom when starting to take estrogen. It can worry a lot of people (à la “aagh, what is this and is it cancer!?”), but is usually nothing to worry about. But just to be sure, do also check out:
Keeping Abreast Of Your Cancer Risk: How To Triple Your Breast Cancer Survival Chances
Estrogen can cause feelings of breast fullness, soreness, nipple irritation, and sometimes lactation, but this later will be minimal—we’re talking a drop or two now and again, not anything that would feed a baby.
Basically, it happens when your body hasn’t been so accustomed to normal estrogen levels in a while, and suddenly wakes up with a jolt, saying to itself “Wait what are we doing puberty again now? I thought we did menopause? Are we pregnant? What’s going on? Ok, checking all systems!” and then may calm down not too long afterwards when it notes that everything is more or less as it should be already.
If this persists or is more than a minor inconvenience though, Dr. Hirsch recommends looking at the likely remedies of:
- Adjust estrogen (usually the cause)
- Adjust progesterone (less common)
- If it’s progesterone, changing the route of administration can ameliorate things
What if it’s not working? Is it just me?
Dr. Hirsch advises the most common reasons are simply:
- wrong formulation (e.g. animal-derived estrogen or hormone analog, instead of bioidentical)
- wrong dose (e.g. too low)
- wrong route of administration (e.g. oral vs transdermal; usually transdermal estradiol is most effective but many people do fine on oral; progesterone meanwhile is usually best as a pessary/suppository, but many people do fine on oral)
Writer’s example: in 2022 there was an estrogen shortage in my country, and while I had been on transdermal estradiol hemihydrate gel, I had to go onto oral estradiol valerate tablets for a few months, because that’s what was available. And the tablets simply did not work for me at all. I felt terrible and I have a good enough intuitive sense of my hormones to know when “something wrong is not right”, and a good enough knowledge of the pharmacology & physiology to know what’s probably happening (or not happening). And sure enough, when I got my blood test results, it was as though I’d been taking nothing. It was such a relief to get back on the gel once it became available again!
So, if something doesn’t seem to be working for you, speak up and get it fixed if at all possible.
See also: What You Should Have Been Told About Menopause Beforehand
Want to know more from Dr. Hirsch?
You might like this book of hers, which we haven’t reviewed yet, but present here for your interest:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
An Accessible New Development Against Alzheimer’s
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dopamine vs Alzheimer’s
One of the key hallmarks of Alzheimer’s disease is the formation of hardened beta-amyloid plaques around neurons. The beta-amyloid peptides themselves are supposed to be in the brain, but the hardened pieces of them that form the plaques are not.
While the full nature of the relationship between those plaques and Alzheimer’s disease is not known for sure (there are likely other factors involved, and “the amyloid hypothesis” is at this stage nominally just that, a hypothesis), one thing that has been observed is that increasing or reducing the plaques increases or reduces (respectively) Alzheimer’s symptoms such as memory loss.
Neprilysin
There is an enzyme, neprilysin, that can break down those plaques.
Neprilysin is made naturally in the brain, and/but we cannot take it as a supplement or medication, because it’s too big to pass through the blood-brain barrier.
A team of researchers led by Dr. Takaomi Saido genetically manipulated mice to produce more neprilysin, and those mice resultantly experienced fewer beta-amyloid plaques and better memory in their old age.
However wonderful for the mice (and a great proof of principle) the above approach is not useful as a treatment for humans whose genomes weren’t modified at our conception in a lab.
Since (as mentioned before) we also can’t take it as a medication/supplement, that leaves one remaining option: find a way to make our already-existing brains produce more of it.
The team’s previous research allowed them to narrow this down to “there is probably a hormone made in the hypothalamus that modulates this”, so they began experimenting with making the mice produce more hormones there.
The DREADD switch
DREADDs, or Designer Receptors Exclusively Activated by Designer Drugs, were the next tool in the toolbox. The scientists attached these designer receptors to dopamine-producing neurons in the mice, so that they could be activated by the appropriate designer drugs—basically, allowing for a “make more dopamine” button, without having to literally wire up the brains with electrodes. The “button” gets triggered instead by a chemical trigger, the designer drug. You can read more about them here:
DREADDs for Neuroscientists: A Primer
The result was positive; when the mice made more dopamine, the result was that they also made more neprilysin. So far, the hypothesis is that the presence of dopamine upregulates the production of neprilysin. In other words, the increased neprilysin levels were caused by the increased dopamine levels (the alternatives would have been: they were both caused by the same thing—in this case that’d be the DREADD activation—or the increase was caused by something else entirely that hadn’t been controlled for).
As to how the causal relationship was determined…
“But I don’t have (or want) a DREADD switch in my head”
Happily for us (and probably happily for the mice too, because dopamine causes feelings of happiness), the experiments continued.
This time, instead of using the DREADD system, they tried simply supplementing the mouse food with l-dopa, a dopamine precursor. L-dopa is often used in the treatment of Parkinson’s disease, because the molecules are small enough to pass through the blood-brain barrier, and can be converted to full dopamine inside the brain itself. So, taking l-dopa normally raises dopamine levels.
The results? The mice who were given l-dopa enjoyed:
- higher dopamine levels
- higher neprilysin levels
- lower beta-amyloid plaque levels
- better memory in tests
The next step for the researchers is to investigate how exactly dopamine regulates neprilysin in the brain, but for now, the relationship between l-dopa consumption and the reduction of Alzheimer’s symptoms seems clear.
You can read about the study here:
The dopaminergic system promotes neprilysin-mediated degradation of amyloid-β in the brain
Is there a catch?
L-dopa has common side effects that are not pleasant; the list begins with nausea and vomiting, and continues with things that one might expect from having “too much of a good thing” when it comes to dopamine, such as dyskinesia (extra movements) and hallucinations.
You can read about it more here at the Parkinson’s Foundation:
Parkinson’s Foundation | Levodopa
However! All is not lost. Rather than reaching for the heavy guns by taking l-dopa unnecessarily, there are other dopamine precursors that don’t have those side effects (and are consequently less restricted, to the point they can be purchased as supplements, or indeed, enjoyed where they occur naturally in some foods).
Top of the list of such safe* and readily-available dopamine precursors is…
N-Acetyl L-Tyrosine (NALT): The Dopamine Precursor & More
If you’d like to try that, here’s an example product on Amazon… Or you could eat fish, white beans, tofu, natto, or pumpkin seeds 😉
*Quick note on safety: “safe” is a relative term and may vary from person to person. Please speak with your own doctor to be sure, check with your pharmacist in case of any meds interactions, and be especially careful taking anything that increases dopamine levels if you have bipolar disorder or are otherwise prone to psychosis of any kind. For most people, this shouldn’t be an issue as our brains have a built-in mechanism for scrubbing excess dopamine and ensuring we don’t end up with too much, but for some people whose dopamine regulation is not so good in that regard, it can cause problems. So again, speak with your doctor to be sure, because we are not doctors, let alone your doctor.
Lastly…
If you’d like an entirely drug-free approach, that’s skipping even the “nutraceuticals”, you might enjoy:
Short On Dopamine? Science Has The Answer
Take care!
Share This Post
-
The Case Against Sugar – by Gary Taubes
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We generally already know that sugar is bad for the health. Most people don’t know how bad.
Taubes makes, as the title goes, “the case against sugar”. Implicated in everything from metabolic syndrome to cancer to Alzheimer’s, sugar is ruinous to the health.
It’s hard to review this book without making a comparison to William Duffy’s 1975 bestseller, “Sugar Blues“. Stylistically it’s very similar, and the general gist is certainly the same.
However! Where this book beats Sugar Blues is in content; Duffy’s book often makes bold claims without scientific backing. Some of those claims didn’t stand the test of time and are now disproven. Instead, Taubes’ book leans on actual up-to-date science, and talks more about what we actually know, than what we imagine.
If this book has a weak point, it’s when it veers away from its main topic and starts talking about, for example, saturated fat. In this side-topic, the book makes some good points, but is less well-considered, cherry-picks data, and lacks nuance.
On its main topic, though, the investigation of sugar, it is rather more thorough.
Bottom line: if you want a next-level motivation to reduce or eliminate dietary sugar, this book may certainly provide that.
Click here to check out The Case Against Sugar and reduce a lot of your health risks!
Share This Post
-
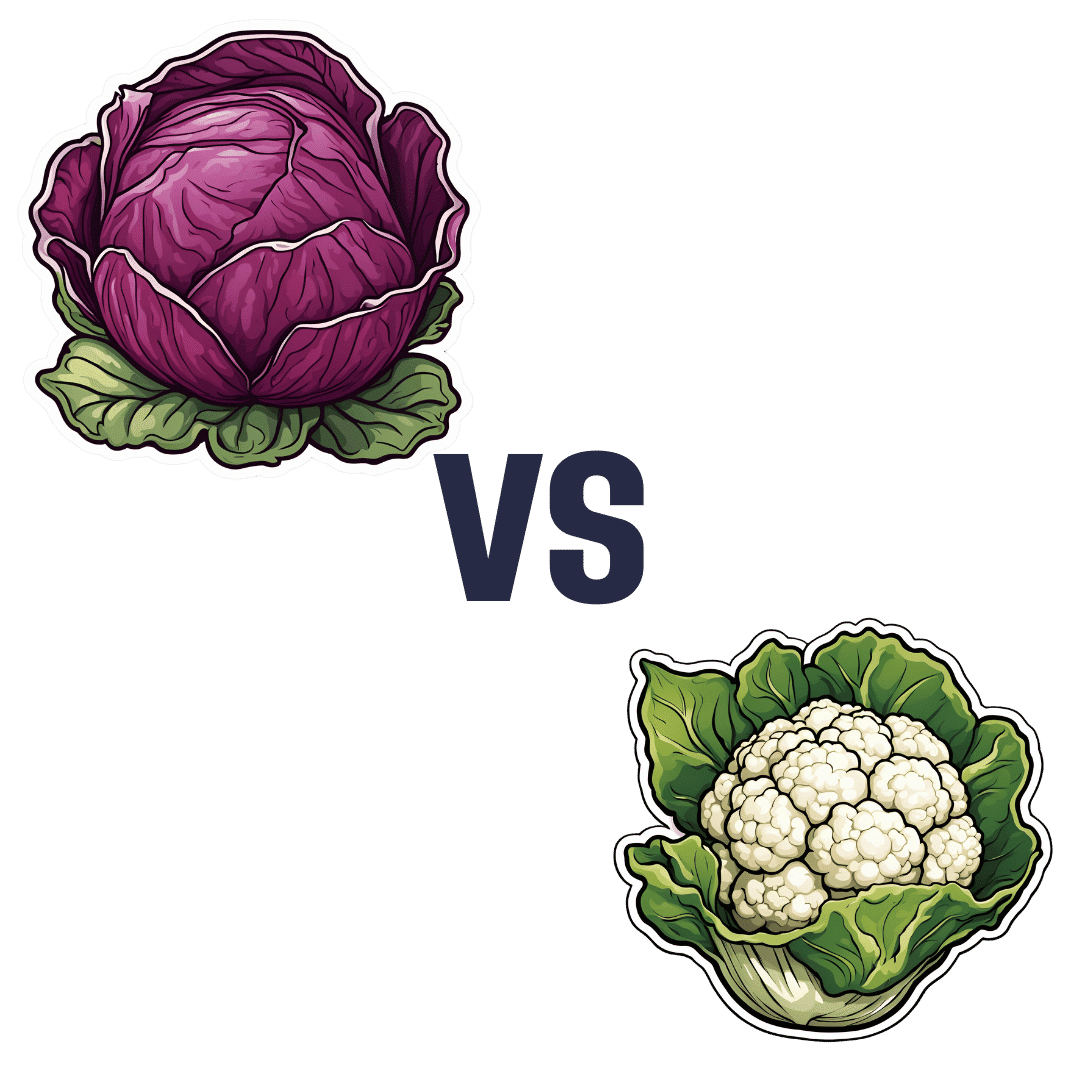
Red Cabbage vs Cauliflower – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing red cabbage to cauliflower, we picked the cabbage.
Why?
In terms of macros, there’s no meaningful difference between them; they’re both mostly water with just enough fiber to hold them together, a small amount of carbs, and an even more trivial amount of protein. So, a tie on macros.
Looking at the vitamins, red cabbage has more of vitamins A, B1, B2, B6, C, E, and K, while cauliflower has more of vitamins B3, B5, B9, and choline. So, a 7:4 win for red cabbage.
In the category of minerals, red cabbage has more calcium, manganese, and iron, while cauliflower has more copper, phosphorus, and potassium. The margins of difference are comparable too, thus, a 3:3 tie on minerals.
It’s always worth taking a look at polyphenols for plants like these, but in this case, once again, there’s not much to set one above the other. However, it’s good to note also that despite them both being Brassica oleracea (same species, different cultivar), there isn’t much overlap in their polyphenol content, meaning they complement each other very well. In particular, red cabbage is a source of luteolin and quercetin, while cauliflower is a source of gallic acid and caffeic acid, for example.
Adding up the three ties and the one win for red cabbage, gives the cabbage the victory today—but do enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
21 Most Beneficial Polyphenols & What Foods Have Them
Enjoy!
Share This Post
Related Posts
-
Thinking about trying physiotherapy for endometriosis pain? Here’s what to expect
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Endometriosis is a condition that affects women and girls. It occurs when tissue similar to the lining of the uterus ends up in other areas of the body. These areas include the ovaries, bladder, bowel and digestive tract.
Endometriosis will affect nearly one million Australian women and girls in their lifetime. Many high-profile Australians are affected by endometriosis including Bindi Irwin, Sophie Monk and former Yellow Wiggle, Emma Watkins.
Symptoms of endometriosis include intense pelvic, abdominal or low back pain (that is often worse during menstruation), bladder and bowel problems, pain during sex and infertility.
But women and girls wait an average of seven years to receive a diagnosis. Many are living with the burden of endometriosis and not receiving treatments that could improve their quality of life. This includes physiotherapy.
Netpixi/Shutterstock How is endometriosis treated?
No treatments cure endometriosis. Symptoms can be reduced by taking medications such as non-steriodal anti-inflammatories (ibuprofen, aspirin or naproxen) and hormonal medicines.
Surgery is sometimes used to diagnose endometriosis, remove endometrial lesions, reduce pain and improve fertility. But these lesions can grow back.
Whether they take medication or have surgery, many women and girls continue to experience pain and other symptoms.
Pelvic health physiotherapy is often recommended as a non-drug management technique to manage endometriosis pain, in consultation with a gynaecologist or general practitioner.
The goal of physiotherapy treatment depends on the symptoms but is usually to reduce and manage pain, improve ability to do activities, and ultimately improve quality of life.
What could you expect from your first appointment?
Physiotherapy management can differ based on the severity and location of symptoms. Prior to physical tests and treatments, your physiotherapist will comprehensively explain what is going to happen and seek your permission.
They will ask questions to better understand your case and specific needs. These will include your age, weight, height as well as the presence, location and intensity of symptoms.
You will also be asked about the history of your period pain, your first period, the length of your menstrual cycle, urinary and bowel symptoms, sexual function and details of any previous treatments and tests.
They may also assess your posture and movement to see how your muscles have changed because of the related symptoms.
During the consultation, your physio will assess you for painful areas and muscle tightness. Netpixi/Shutterstock They will press on your lower back and pelvic muscles to spot painful areas (trigger points) and muscle tightness.
If you consent to a vaginal examination, the physiotherapist will use one to two gloved fingers to assess the area inside and around your vagina. They will also test your ability to coordinate, contract and relax your pelvic muscles.
What type of treatments could you receive?
Depending on your symptoms, your physiotherapist may use the following treatments:
General education
Your physiotherapist will give your details about the disease, pelvic floor anatomy, the types of treatment and how these can improve pain and other symptoms. They might teach you about the changes to the brain and nerves as a result of being in long-term pain.
They will provide guidance to improve your ability to perform daily activities, including getting quality sleep.
If you experience pain during sex or difficulty using tampons, they may teach you how to use vaginal dilators to improve flexibility of those muscles.
Pelvic muscle exercises
Pelvic muscles often contract too hard as a result of pain. Pelvic floor exercises will help you contract and relax muscles appropriately and provide an awareness of how hard muscles are contracting.
This can be combined with machines that monitor muscle activity or vaginal pressure to provide detailed information on how the muscles are working.
Yoga, stretching and low-impact exercises
Yoga, stretching and low impact aerobic exercise can improve fitness, flexibility, pain and blood circulation. These have general pain-relieving properties and can be a great way to contract and relax bigger muscles affected by long-term endometriosis.
These exercises can help you regain function and control with a gradual progression to perform daily activities with reduced pain.
Low-impact exercise can reduce pain. ABO Photography/Shutterstock Hydrotherapy (physiotherapy in warm water)
Performing exercises in water improves blood circulation and muscle relaxation due to the pressure and warmth of the water. Hydrotherapy allows you to perform aerobic exercise with low impact, which will reduce pain while exercising.
However, while hydrotherapy shows positive results clinically, scientific studies to show its effectiveness studies are ongoing.
Manual therapy
Women frequently have small areas of muscle that are tight and painful (trigger points) inside and outside the vagina. Pain can be temporarily reduced by pressing, massaging or putting heat on the muscles.
Physiotherapists can teach patients how to do these techniques by themselves at home.
What does the evidence say?
Overall, patients report positive experiences pelvic health physiotherapists treatments. In a study of 42 women, 80% of those who received manual therapy had “much improved pain”.
In studies investigating yoga, one study showed pain was reduced in 28 patients by an average of 30 points on a 100-point pain scale. Another study showed yoga was beneficial for pain in all 15 patients.
But while some studies show this treatment is effective, a review concluded more studies were needed and the use of physiotherapy was “underestimated and underpublicised”.
What else do you need to know?
If you have or suspect you have endometriosis, consult your gynaecologist or GP. They may be able to suggest a pelvic health physiotherapist to help you manage your symptoms and improve quality of life.
As endometriosis is a chronic condition you may be entitled to five subsidised or free sessions per calendar year in clinics that accept Medicare.
If you go to a private pelvic health physiotherapist, you won’t need a referral from a gynaecologist or GP. Physiotherapy rebates can be available to those with private health insurance.
The Australian Physiotherapy Association has a Find a Physio section where you can search for women’s and pelvic physiotherapists. Endometriosis Australia also provides assistance and advice to women with Endometriosis.
Thanks to UTS Masters students Phoebe Walker and Kasey Collins, who are researching physiotherapy treatments for endometriosis, for their contribution to this article.
Peter Stubbs, Senior Lecturer in Physiotherapy, University of Technology Sydney and Caroline Wanderley Souto Ferreira, Visiting Professor of Physiotherapy, University of Technology Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
With Medical Debt Burdening Millions, a Financial Regulator Steps In to Help
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When President Barack Obama signed legislation in 2010 to create the Consumer Financial Protection Bureau, he said the new agency had one priority: “looking out for people, not big banks, not lenders, not investment houses.”
Since then, the CFPB has done its share of policing mortgage brokers, student loan companies, and banks. But as the U.S. health care system turns tens of millions of Americans into debtors, this financial watchdog is increasingly working to protect beleaguered patients, adding hospitals, nursing homes, and patient financing companies to the list of institutions that regulators are probing.
In the past two years, the CFPB has penalized medical debt collectors, issued stern warnings to health care providers and lenders that target patients, and published reams of reports on how the health care system is undermining the financial security of Americans.
In its most ambitious move to date, the agency is developing rules to bar medical debt from consumer credit reports, a sweeping change that could make it easier for Americans burdened by medical debt to rent a home, buy a car, even get a job. Those rules are expected to be unveiled later this year.
“Everywhere we travel, we hear about individuals who are just trying to get by when it comes to medical bills,” said Rohit Chopra, the director of the CFPB whom President Joe Biden tapped to head the watchdog agency in 2021.
“American families should not have their financial lives ruined by medical bills,” Chopra continued.
The CFPB’s turn toward medical debt has stirred opposition from collection industry officials, who say the agency’s efforts are misguided. “There’s some concern with a financial regulator coming in and saying, ‘Oh, we’re going to sweep this problem under the rug so that people can’t see that there’s this medical debt out there,’” said Jack Brown III, a longtime collector and member of the industry trade group ACA International.
Brown and others question whether the agency has gone too far on medical billing. ACA International has suggested collectors could go to court to fight any rules barring medical debt from credit reports.
At the same time, the U.S. Supreme Court is considering a broader legal challenge to the agency’s funding that some conservative critics and financial industry officials hope will lead to the dissolution of the agency.
But CFPB’s defenders say its move to address medical debt simply reflects the scale of a crisis that now touches some 100 million Americans and that a divided Congress seems unlikely to address soon.
“The fact that the CFPB is involved in what seems like a health care issue is because our system is so dysfunctional that when people get sick and they can’t afford all their medical bills, even with insurance, it ends up affecting every aspect of their financial lives,” said Chi Chi Wu, a senior attorney at the National Consumer Law Center.
CFPB researchers documented that unpaid medical bills were historically the most common form of debt on consumers’ credit reports, representing more than half of all debts on these reports. But the agency found that medical debt is typically a poor predictor of whether someone is likely to pay off other bills and loans.
Medical debts on credit reports are also frequently riddled with errors, according to CFPB analyses of consumer complaints, which the agency found most often cite issues with bills that are the wrong amount, have already been paid, or should be billed to someone else.
“There really is such high levels of inaccuracy,” Chopra said in an interview with KFF Health News. “We do not want to see the credit reporting system being weaponized to get people to pay bills they may not even owe.”
The aggressive posture reflects Chopra, who cut his teeth helping to stand up the CFPB almost 15 years ago and made a name for himself going after the student loan industry.
Targeting for-profit colleges and lenders, Chopra said he was troubled by an increasingly corporate higher-education system that was turning millions of students into debtors. Now, he said, he sees the health care system doing the same thing, shuttling patients into loans and credit cards and reporting them to credit bureaus. “If we were to rewind decades ago,” Chopra said, “we saw a lot less reliance on tools that banks used to get people to pay.”
The push to remove medical bills from consumer credit reports culminates two years of intensive work by the CFPB on the medical debt issue.
The agency warned nursing homes against forcing residents’ friends and family to assume responsibility for residents’ debts. An investigation by KFF Health News and NPR documented widespread use of lawsuits by nursing homes in communities to pursue friends and relatives of nursing home residents.
The CFPB also has highlighted problems with how hospitals provide financial assistance to low-income patients. Regulators last year flagged the dangers of loans and credit cards that health care providers push on patients, often saddling them with more debt.
And regulators have gone after medical debt collectors. In December, the CFPB shut down a Pennsylvania company for pursuing patients without ensuring the debts were accurate.
A few months before that, the agency fined an Indiana company working with medical debt for violating collection laws. Regulators said the company had “risked harming consumers by pressuring or inducing them to pay debts they did not owe.”
With their business in the crosshairs, debt collectors are warning that cracking down on credit reporting and other collection tools may prompt more hospitals and doctors to demand patients pay upfront for care.
There are some indications this is happening already, as hospitals and clinics push patients to enroll in loans or credit cards to pay their medical bills.
Scott Purcell, CEO of ACA International, said it would be wiser for the federal government to focus on making medical care more affordable. “Here we’re coming up with a solution that only takes money away from providers,” Purcell said. “If Congress was involved, there could be more robust solutions.”
Chopra doesn’t dispute the need for bigger efforts to tackle health care costs.
“Of course, there are broader things that we would probably want to fix about our health care system,” he said, “but this is having a direct financial impact on so many Americans.”
The CFPB can’t do much about the price of a prescription or a hospital bill, Chopra continued. What the federal agency can do, he said, is protect patients if they can’t pay their bills.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The End of Alzheimer’s – by Dr. Dale Bredesen
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This one didn’t use the “The New Science Of…” subtitle that many books do, and this one actually is a “new science of”!
Which is exciting, and/but comes with the caveat that the overall protocol itself is still undergoing testing, but the results so far are promising. The constituent parts of the protocol are for the most already well-established, but have not previously been put together in this way.
Dr. Bredesen argues that Alzheimer’s Disease is not one condition but three (medical consensus agrees at least that it is a collection of conditions, but different schools of thought slice them differently), and outlines 36 metabolic factors that are implicated, and the good news is, most of them are within our control.
Since there’s a lot to put together, he also offers many workarounds and “crutches”, making for very practical advice.
The style of the book is on the hard end of pop-science, that is to say while the feel and tone is very pop-sciencey, there are nevertheless a lot of words that you might know but your spellchecker probably wouldn’t. He does explain everything along the way, but this does mean that if you’re not already well-versed, you can’t just dip in to a later point without reading the earlier parts.
Bottom line: even if you only implement half the advice in this book, you’ll be doing your long-term cognitive health a huge favor.
Click here to check out The End of Alzheimer’s, and keep cognitive decline at bay!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: