The Most Underrated Hip Mobility Exercise (Not Stretching)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cori Lefkowith, of “Redefining Strength” and “Strong At Every Age” fame, is back to help us keep our hips in good order:
These tips don’t lie
It’s less about stretching, and more about range of motion and “use it or lose it”:
- Full range of motion in lifting exercises enhances joint mobility and stability, whereas strengthening muscles through a limited range of motion (e.g., half squats) can cause tightness.
- Lifting through a larger range of motion may result in faster strength gains too, so that’s a bonus.
- Customize your range of motion based on your body type and capability, but do try for what you reasonably can—don’t give up!
- Lower weights and focus on deeper movements like split squats or single-leg squats, but work up slowly if you have any difficulties to start with.
- Using exercises like the Bulgarian split squat and deficit split squat can improve hip mobility and strength (you’ll really need to see the video for this one)
- Fully controlling the range of motion is key to progress, even if it means going lighter; prioritize mobility over brute strength. Strength is good, but mobility is even more critical.
- Adding instability, such as raising the front foot in lunges, challenges muscles and increases mobility. Obviously, please be safe while doing so, and slowly increase the range of motion while maintaining control, avoiding reliance on momentum.
- Final tip that most don’t consider: try starting exercises from the bottom position to ensure proper form and muscle engagement!
For more on each of these plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Does Ginseng Increase Testosterone Levels?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
❓ Q&A With 10almonds Subscribers!
Q: You talked about spearmint as reducing testosterone levels, what about ginseng for increasing them?
A: Hormones are complicated and often it’s not a simple matter of higher or lower levels! It can also be a matter of…
- how your body converts one thing into another
- how your body responds (or not) to something according to how the relevant hormone’s receptors are doing
- …and whether there’s anything else blocking those receptors.
All this to say: spearmint categorically is an anti-androgen, but the mechanism of action remains uncertain.
Panax ginseng, meanwhile, is one of the most well-established mysteries in herbal medicine.
Paradoxically, it seems to improve both male and female hormonal regulation, despite being more commonly associated with the former.
- It doesn’t necessarily increase or decrease testosterone or estrogen levels (but it can, even if indirectly)
- It does improve sexual function
- …and alleviates symptoms associated with conditions as varied as:
- Late-onset hypogonadism (common for men during the andropause)
- Benign prostate hyperplasia (again common for men during the andropause)
- …and also counteracts unwanted side-effects of finasteride. Finasteride is often taken by men as a hair loss remedy or, less often but critically, in the case of an enlarged prostate.
But it also…
- Alleviates symptoms of PCOS (polycystic ovary syndrome, which effects around 20% of women)
- May even be an effective treatment for PCOS (rat model only so far)
- It also may improve female reproductive fertility more generally (the studies are down to fruit flies now though)
Bottom line: Panax ginseng is popularly taken to improve natural hormone function, a task at which it appears to excel.
Scientists are still working out exactly how it does the many things it appears to do.
Progress has been made, and it clearly is science rather than witchcraft, but there are still far more unanswered questions than resolved ones!
Share This Post
-
Fatigue? Unexplained weight gain and dry skin? Could it be Hashimoto’s disease?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Maybe you feel worn out. Perhaps you’re also having trouble losing weight. Generally, you just don’t feel 100%.
Could it be Hashimoto’s disease? This common autoimmune thyroid disorder is when your immune system (which fights off viruses and bacteria), mistakenly attacks a part of your body. In this case, it’s your thyroid – a gland located at the base of your neck – and can cause low thyroid hormones levels (hypothyroidism).
Hypothyroidism affects one in 33 Australians and Hashimoto’s is one of the most common thyroid conditions in first-world countries.
While symptoms can be subtle, untreated Hashimoto’s can cause long-term problems with your heart, memory and fertility. Here is what you need to know.
What happens when you have Hashimoto’s?
Your thyroid gland is a butterfly-shaped gland in the neck. It is essential in regulating things like muscle function, digestion, metabolism, the heart and lungs. In children, thyroid hormones are also needed for normal growth and development.
Hashimoto’s thyroid disease, named after the Japanese doctor who discovered it in 1912, is also known as Hashimoto’s thyroiditis or chronic lymphocytic thyroiditis. The disease can cause the immune system to mistakenly produce proteins called antibodies (thyroid peroxidase and thyroglobulin). These can cause inflammation and long-term damage to the thyroid gland. Over time, as thyroid tissue is inflamed and/or destroyed, there can be a decrease in the production of thyroid hormones (hypothyroidism).
Hashimoto’s can present subtly at first. If you only have antibodies with no change in thyroid levels, it is likely you won’t have any symptoms.
However, as the disease progresses, you may experience fatigue, weight gain (or difficulty losing weight), increased sensitivity to the cold, constipation, dry skin, muscle aches, irregular or heavy menstrual cycles, enlarged thyroid (goitre) and occasionally hair loss, including at the ends of your eyebrows.
What causes Hashimoto’s thyroid disease?
Several risk factors can contribute to the development of Hashimoto’s including:
-
genetic risk – your risk is higher if you have family members with Hashimoto’s
-
gender – women are up to ten times more likely than men to develop the disease
-
age – you are more likely to develop the disease from 30 to 50 years of age
-
autoimmune condition – having another autoimmune condition like systemic lupus, Type 1 diabetes and celiac disease increases your risk
-
excessive iodine intake and radiation exposure may also increase risk in people who are already genetically at greater risk.
What are the long-term risks?
Long-term, untreated Hashimoto’s thyroiditis can cause heart issues, higher cholesterol levels, nerve damage (peripheral neuropathy), reduced cognition and infertility.
In pregnancy, Hashimoto’s has a higher risk of pre-eclampsia (high blood pressure affecting several organs), premature birth, placental abruption (when the placenta separates from the inner wall of the uterus before birth) and, in severe cases, pregnancy loss.
The disease has also been linked with an increased risk (but low incidence) of the lymphocytes of the thyroid turning into cancer cells to cause thyroid lymphoma.
How is Hashimoto’s diagnosed?
Diagnosis can be confirmed with a blood test to check thyroid levels and antibodies.
Thyroid peroxidase antibodies are commonly present but about 5% of patients test antibody-negative. In those people, diagnosis depends on the thyroid levels, clinical presentation and ultrasound appearance of general inflammation. An ultrasound may not be required though, especially if the diagnosis is obvious.
Three hormone levels are tested to determine if you have Hashimoto’s.
Thyroid stimulating hormone (TSH) is produced by the brain to speak to the thyroid, telling it to produce two types of thyroid hormones – T3 and T4.
If you have either relative or absolute thyroid hormone deficiency, a test will show the stimulating hormones as high because the brain is trying to get the thyroid to work harder.
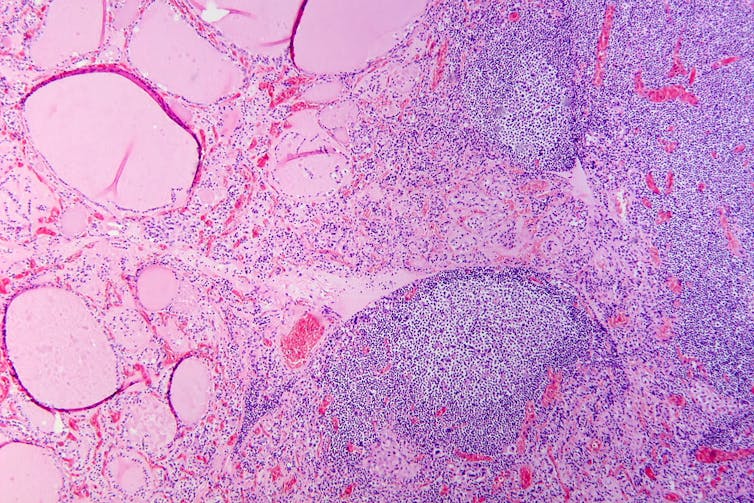
Hashimoto’s thyroiditis under the microscope. Antibodies against thyroid peroxidase and thyroglobulin were elevated.
Patho/Wikimedia Commons, CC BY-SACan it be treated?
The management of Hashimoto’s depends on the severity of the thyroid levels. Up to 20% of the population can have antibodies but normal thyroid levels. This is still Hashimoto’s thyroid disease, but it is very mild and does not require treatment. There is no current treatment to reduce antibody levels alone.
Because thyroid peroxidase antibodies increase the risk of abnormal thyroid levels in the future, regular thyroid testing is recommended.
When the thyroid stimulating hormone is high with normal thyroid hormone levels it is termed “subclinical hypothyroidism”. When it is paired with low hormone levels it is called “overt hypothyroidism”. The first is a mild form of the disease and treatment depends on the degree of stimulating hormone elevation.
Overt hypothyroidism warrants treatment. The main form of this is thyroid hormone replacement therapy (levothyroxine) with the dose of the drug adjusted until thyroid levels are within the normal range. This is usually a lifelong treatment but, once the dose is optimised, hormone levels usually remain relatively stable.
In some people with very enlarged thyroid glands causing compressive symptoms (such as difficulty swallowing or breathing), thyroidectomy (surgical removal of the thyroid) is considered.
Hashimoto’s thyroiditis is a common condition caused by your body’s immune system incorrectly damaging to your thyroid and can go undetected. Long-term, untreated, it can cause issues with your heart, cognition, and fertility. It can be diagnosed with a simple blood test. Speak to your doctor if you have any concerns as early diagnosis and treatment can help prevent complications.
Aakansha Zala, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
-
Almonds vs Pecans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing almonds to pecans, we picked the almonds.
Why?
In terms of macros, almonds have more protein, carbs, and fiber, as well as the lower glycemic index. A strong start for almonds here, though pecans have more fat (and the healthy blend of fats is quite comparable from one nut to the other).
In the category of vitamins, almonds have more of vitamins B2, B3, B9, E, and choline, while pecans have more of vitamins A, B1, B5, B6, and K. Numerically that’s a tie, though the biggest margins of difference are for vitamins A and E, respectively, and we might want to prioritize almonds’ extra vitamin E, over pecans’ extra vitamin A, given that vitamin A is more easily found in large quantities in many foods, whereas vitamin E is not quite so abundant generally. So in short, either a tie or a slight win for almonds here.
When it comes to minerals, both contain a lot of goodness, but almonds have more calcium, iron, magnesium, phosphorus, potassium, and selenium, while pecans have more copper, manganese, and zinc. A clear win for almonds, though as we say, pecans are also great for this, just not as great as almonds.
As a side-note, both of these nuts have been found to have anticancer properties against breast cancer cell lines. In all likelihood this means they help against other cancers too, but breast cancer is what the extant research has been for.
So, naturally, enjoy either or both (in fact, both is ideal). But if you want to choose one for nutritional density, it’s almonds.
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Share This Post
Related Posts
-
The Diet Myth – by Dr. Tim Spector
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Why are we supposed to go low-carb, but get plenty of whole grains? Avoid saturated fat, but olive oil is one of the healthiest fats around? Will cheese kill us or save us? Even amongst the well-informed, there’s a lot of confusion. This book addresses these and many such topics.
A main theme of the book is howa lot of it relates to the state of our gut microbiome, and what is good or bad for that. He also discusses, for example, how microbes predict obesity better than genes, and the good news is: we can change our microbes a lot more easily than we can change our genes!
In the category of criticism, he repeats some decades-old bad science in some areas outside of his field (i.e. unrelated to nutrition), so that’s unfortunate, and/but doesn’t detract from the value of the book if we keep to the main topic.
Bottom line: if you’d like to understand better the physiology and microbiology behind why dieting does work for most people (and how to do it better), then this is a great book for that.
Click here to check out The Diet Myth, and learn the science behind the confusion!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
High-Octane Brain – by Dr. Michelle Braun
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
True to the title, Dr. Braun jumps straight into action here, making everything as practical as possible as quickly as possible and giving the most attention to the science-based steps to take. Thereafter, and almost as an addendum, she gives examples of “brain role models” from various age groups, to show how these things can be implemented and benefitted-from in the real world.
The greatest strength of this book is that it is the product of a lot of hard science made easy; this book has hundreds of scientific references (of which, many RCTs etc), and many contributions from other professionals in her field, to make one of the most evidence-based guidebooks around, and all presented in one place and in a manner that is perfectly readable to the layperson.
The style, thus, is easy-reading, with references for those who want to jump into further reading but without that being required for applying the advice within.
Bottom line: if you’d like to improve your brain with an evidence-based health regiment and minimal fluff, this is the book for you.
Click here to check out High-Octane Brain, and level-up yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Dates vs Grapes – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing dates to grapes, we picked the dates.
Why?
It’s not close:
In terms of macros, dates have 4x the carbs and/but 8x the fiber, making for the lower glycemic index. Also, for what it’s worth, they have nearly 4x the protein, but probably nobody is eating either of these fruits for the protein. In any case, it’s an easy and clear win for dates in the category of macros.
In the category of vitamins, dates have more of vitamins B2, B3, B5, B6, B9, and choline, while grapes have more of vitamins B1, C, E, and K, making for a 6:4 win for dates.
When it comes to minerals, it’s more one-sided: dates have more calcium, copper, iron, magnesium, phosphorus, potassium, selenium, and zinc, while grapes have more manganese. An easy win for dates here.
Of course, enjoy either or both (diversity is good), but if you’re looking for nutrient density, dates are where it’s at.
Want to learn more?
You might like:
Can We Drink To Good Health? ← while there are polyphenols such as resveratrol in red wine that per se would boost heart health, there’s so little per glass that you may need 100–1000 glasses per day to get the dosage that provides benefits in mouse studies.
If you’re not a mouse, you might even need more than that!
To this end, many people prefer resveratrol supplementation ← link is to an example product on Amazon, but there are plenty more so feel free to shop around 😎
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: