What Flexible Dieting Really Means
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Flexibility Is The Dish Of The Day
This is Alan Aragon. Notwithstanding not being a “Dr. Alan Aragon”, he’s a research scientist with dozens of peer-reviewed nutrition science papers to his name, as well as being a personal trainer and fitness educator. Most importantly, he’s an ardent champion of making people’s pursuit of health and fitness more evidence-based.
We’ll be sharing some insights from a book of his that we haven’t reviewed yet, but we will link it at the bottom of today’s article in any case.
What does he want us to know?
First, get out of the 80s and into the 90s
In the world of popular dieting, the 80s were all about calorie-counting and low-fat diets. They did not particularly help.
In the 90s, it was discovered that not only was low-fat not the way to go, but also, regardless of the diet in question, rigid dieting leads to “disinhibition”, that is to say, there comes a point (usually not far into a diet) whereby one breaks the diet, at which point, the floodgates open and the dieter binges unhealthily.
Aragon would like to bring our attention to a number of studies that found this in various ways over the course of the 90s measuring various different metrics including rigid vs flexible dieting’s impacts on BMI, weight gain, weight loss, lean muscle mass changes, binge-eating, anxiety, depression, and so forth), but we only have so much room here, so here’s a 1999 study that’s pretty much the culmination of those:
Flexible vs. Rigid Dieting Strategies: Relationship with Adverse Behavioral Outcomes
So in short: trying to be very puritan about any aspect of dieting will not only not work, it will backfire.
Next, get out of the 90s into the 00s
…which is not only fun if you read “00s” out loud as “naughties”, but also actually appropriate in this case, because it is indeed important to be comfortable being a little bit naughty:
In 2000, Dr. Marika Tiggemann found that dichotomous perceptions of food (e.g. good/bad, clean/dirty, etc) were implicated as a dysfunctional cognitive style, and predicted not only eating disorders and mood disorders, but also adverse physical health outcomes:
Dieting and Cognitive Style: The Role of Current and Past Dieting Behaviour and Cognitions
This was rendered clearer, in terms of physical health outcomes, by Dr. Susan Byrne & Dr. Emma Dove, in 2009:
❝Weight loss was negatively associated with pre-treatment depression and frequency of treatment attendance, but not with dichotomous thinking. Females who regard their weight as unacceptably high and who think dichotomously may experience high levels of depression irrespective of their actual weight, while depression may be proportionate to the degree of obesity among those who do not think dichotomously❞
Aragon’s advice based on all this: while yes, some foods are better than others, it’s more useful to see foods as being part of a spectrum, rather than being absolutist or “black and white” about it.
Next: hit those perfect 10s… Imperfectly
The next decade expanded on this research, as science is wont to do, and for this one, Aragon shines a spotlight on Dr. Alice Berg’s 2018 study with obese women averaging 69 years of age, in which…
In other words (and in fact, to borrow Dr. Berg’s words from that paper),
❝encouraging a flexible approach to eating behavior and discouraging rigid adherence to a diet may lead to better intentional weight loss for overweight and obese older women❞
You may be wondering: what did this add to the studies from the 90s?
And the key here is: rather than being observational, this was interventional. In other words, rather than simply observing what happened to people who thought one way or another, this study took people who had a rigid, dichotomous approach to food, and gave them a 6-month behavioral intervention (in other words, support encouraging them to be more flexible and open in their approach to food), and found that this indeed improved matters for them.
Which means, it’s not a matter of fate or predisposition, as it could have been back in the 90s, per “some people are just like that; who’s to say which factor causes which”. Instead, now we know that this is an approach that can be adopted, and it can be expected to work.
Beyond weight loss
Now, so far we’ve talked mostly about weight loss, and only touched on other health outcomes. This is because:
- weight loss a very common goal for many
- it’s easy to measure so there’s a lot of science for it
Incidentally, if it’s a goal of yours, here’s what 10almonds had to say about that, along with two follow-up articles for other related goals:
Spoiler: we agree with Aragon, and recommend a relaxed and flexible approach to all three of these things
Aragon’s evidence-based approach to nutrition has found that this holds true for other aspects of healthy eating, too. For example…
To count or not to count?
It’s hard to do evidence-based anything without counting, and so Aragon talks a lot about this. Indeed, he does a lot of counting in scientific papers of his own, such as:
and
The effect of protein timing on muscle strength and hypertrophy: a meta-analysis
…as well as non-protein-related but diet-related topics such as:
But! For the at-home health enthusiast, Aragon recommends that the answer to the question “to count or not to count?” is “both”:
- Start off by indeed counting and tracking everything that is important to you (per whatever your current personal health intervention is, so it might be about calories, or grams of protein, or grams of carbs, or a certain fat balance, or something else entirely)
- Switch to a more relaxed counting approach once you get used to the above. By now you probably know the macros for a lot of your common meals, snacks, etc, and can tally them in your head without worrying about weighing portions and knowing the exact figures.
- Alternatively, count moderately standardized portions of relevant foods, such as “three servings of beans or legumes per day” or “no more than one portion of refined carbohydrates per day”
- Eventually, let habit take the wheel. Assuming you have established good dietary habits, this will now do you just fine.
This latter is the point whereby the advice (that Aragon also champions) of “allow yourself an unhealthy indulgence of 10–20% of your daily food”, as a budget of “discretionary calories”, eventually becomes redundant—because chances are, you’re no longer craving that donut, and at a certain point, eating foods far outside the range of healthiness you usually eat is not even something that you would feel inclined to do if offered.
But until that kicks in, allow yourself that budget of whatever unhealthy thing you enjoy, and (this next part is important…) do enjoy it.
Because it is no good whatsoever eating that cream-filled chocolate croissant and then feeling guilty about it; that’s the dichotomous thinking we had back in the 80s. Decide in advance you’re going to eat and enjoy it, then eat and enjoy it, then look back on it with a sense of “that was enjoyable” and move on.
The flipside of this is that the importance of allowing oneself a “little treat” is that doing so actively helps ensure that the “little treat” remains “little”. Without giving oneself permission, then suddenly, “well, since I broke my diet, I might as well throw the whole thing out the window and try again on Monday”.
On enjoying food fully, by the way:
Mindful Eating: How To Get More Nutrition Out Of The Same Food
Want to know more from Alan Aragon?
Today we’ve been working heavily from this book of his; we haven’t reviewed it yet, but we do recommend checking it out:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Try This At Home: ABI Test For Clogged Arteries
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Arterial plaque is a big deal, and statistically it’s more of a risk as we get older, often coming to a head around age 72 for women and 65 for men—these are the median ages at which people who are going to get heart attacks, get them. Or get it, because sometimes one is all it takes.
The Ankle-Brachial Index Test
Dr. Brewer recommends a home test for detecting arterial plaque called the Ankle-Brachial Index (ABI), which uses a blood pressure monitor. The test involves measuring blood pressure in both the arms and ankles, then calculating the ratio of these measurements:
- A healthy ABI score is between 1.0 and 1.4; anything outside this range may indicate arterial problems.
- Low ABI scores (below 0.8) suggest plaque is likely obstructing blood flow
- High ABI scores (above 1.4) may indicate artery hardening
Peripheral Artery Disease (PAD), associated with poor ABI results (be they high or low), can cause a whole lot of problems that are definitely better tackled sooner rather than later—remember that atherosclerosis is a self-worsening thing once it gets going, because narrower walls means it’s even easier for more stuff to get stuck in there (and thus, the new stuff that got stuck also becomes part of the walls, and the problem gets worse).
If you need a blood pressure monitor, by the way, here’s an example product on Amazon.
Do note also that yes, if you have plaque obstructing blood flow and hardened arteries, your scores may cancel out and give you a “healthy” score, despite your arteries being very much not healthy. For this reason, this test can be used to raise the alarm, but not to give the “all clear”.
For more on all of the above, plus a demonstration and more in-depth explanation of the test, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
-
Behaving During the Holidays
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝It’s hard to “behave” when it comes to holiday indulging…I’m on a low sodium, sugar restricted regimen from my doctor. Trying to get interested in bell peppers as a snack…wish me luck!❞
Good luck! Other low sodium, low sugar snacks include:
- Nuts! Unsalted, of course. We’re biased towards almonds 😉
- Mixed nuts are an especially healthy way to snack, though (assuming you don’t have an allergy, obviously)
- Air-popped popcorn (you can season it, just not with salt/sugar!)
- Fruit (but not fruit juice; it has to be in solid form)
- Peas (not a classic snack food, we know, but they can be enjoyed many ways)
- Seriously, try them frozen or raw! Frozen/raw peas are a great sweet snack.
- Chickpeas are great dried/roasted, by the way, and give much of the same pleasure as a salty snack without being salty! Obviously, this means cooking them without salt, but that’s fine, or if using tinned, choose “in water” rather than “in brine”
- Hummus is also a great healthy snack (check the ingredients for salt if not making it yourself, though) and can be enjoyed as a dip using raw vegetables (celery, carrot sticks, cruciferous vegetables, whatever you prefer)
Enjoy!
Share This Post
- Nuts! Unsalted, of course. We’re biased towards almonds 😉
-
The Rise Of The Machines
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In this week’s health science news, several pieces of technology caught our eye. Let’s hope these things roll out widely!
When it comes to UTIs, antimicrobial resistance is taking the p—
This has implications far beyond UTIs—though UTIs can be a bit of a “canary in the coal mine” for antimicrobial resistance. The more people are using antibiotics (intentionally, or because they are in the food chain), the more killer bugs are proliferating instead of dying when we give them something to kill them. And yes: they do proliferate sometimes when given antibiotics, not because the antibiotics did anything directly good for them, but because they killed their (often friendly bacteria) competition. Thus making for a double-whammy of woe.
This development tackles that, by using AI modelling to crunch the numbers of a real-time data-driven personalized approach to give much more accurate treatment options, in a way that a human couldn’t (or at least, couldn’t at anything like the same speed, and most family physicians don’t have a mathematician locked in the back room to spend the night working on a patient’s data).
Read in full: AI can help tackle urinary tract infections and antimicrobial resistance
Related: AI: The Doctor That Never Tires?
When it comes to CPR and women, people are feint of heart
When CPR is needed, time is very much of the essence. And yet, bystanders are much less likely to give CPR to a woman than to a man. Not only that, but CPR-training is part of what leads to this reluctance when it comes to women: the mannequins used are very homogenous, being male (94%) and lean (99%). They’re also usually white (88%) even in countries where the populations are not, but that is less critical. After all, a racist person is less likely to give CPR to a person of color regardless of what color the training mannequin was.
However, the mannequins being male and lean is an issue, because it means people suddenly lack confidence when faced with breasts and/or abundant body fat. Both can prompt the bystander to wonder if some different technique is needed (it isn’t), and breasts can also prompt the bystander to fear doing something potentially “improper” (the proper course of action is: save a person’s life; do not get distracted by breasts).
Read in full: Women are less likely to receive CPR than men. Training on manikins with breasts could help ← there are also CPR instructions (and a video demonstration) there, for anyone who wants a refresher, if perhaps your last first-aid course was a while ago!
Related: Heart Attack: His & Hers (Be Prepared!)
When technology is a breath of fresh air
A woman with COPD and COVID has had her very damaged lungs replaced using a da Vinci X robot to perform a minimally-invasive surgery (which is quite a statement, when it comes to replacing someone’s lungs).
Not without human oversight though—surgeon Dr. Stephanie Chang was directing the transplant. Surgery is rarely fun for the person being operated on, but advances like this make things go a lot more smoothly, so this kind of progress is good to see.
Read in full: Woman receives world’s first robotic double-lung transplant
Related: Why Chronic Obstructive Pulmonary Disease (COPD) Is More Likely Than You Think
Take care!
Share This Post
Related Posts
-
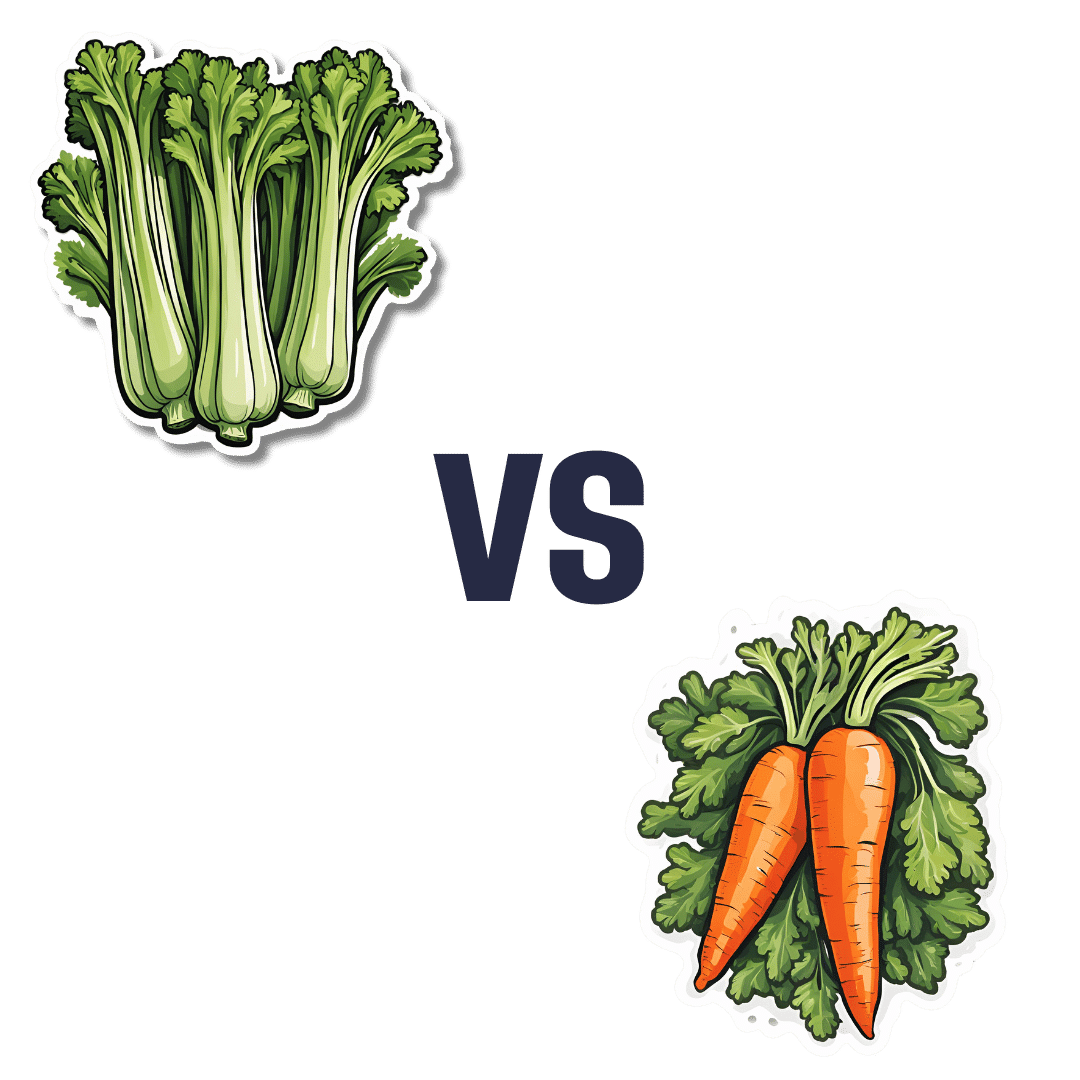
Celery vs Carrot – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing celery to carrot, we picked the carrot.
Why?
In terms of macros, carrot has more protein, carbs, and fiber, and is thus the “most food per food” option. The carb:fiber ratio is such that they have about the same glycemic index (when raw, anyway).
In the category of vitamins, celery has more of vitamins B9 and K, while carrot has more of vitamins A, B1, B2, B3, B5, B6, C, E, and choline. An easy win for carrot here.
When it comes to minerals, celery has more calcium and selenium, while carrot has more copper, iron, magnesium, manganese, phosphorus, potassium, and zinc. Another clear win for carrot.
In short, both are very respectable foods, but carrot simply has more in it, and it’s all good.
Enjoy!
Want to learn more?
You might like to read:
Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Cough Doctor
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Cough Doctor
This is Dr. Peter Small, who worked in epidemiology since the beginning of HIV epidemic. He became a pioneer in the field of molecular epidemiology. As such, his work was a guiding beacon for the public health response to the resurgence of tuberculosis. He’s travelled the world spending years in various institutions studying all manner of respiratory illnesses…. These have ranged from tuberculosis to pneumonia to lung cancer and (back to epidemiology) Covid-19.
He’s now the Chief Medical Officer at…
Hyfe
Hyfe, a medical AI company, was founded in 2020. Its objective: to build acoustic tools for respiratory diagnostics and monitoring.
In other words: it records coughs and collects data about coughing.
❝It’s ironic how much people focus on counting steps while ignoring cough, which is far more consequential. Hyfe is a science-driven company with the technology to make cough count. Particularly now, with increased awareness of cough and the rapid growth of digital health driven by Covid-19, this technology can improve the lives of patients, the care provided by doctors, and the efficiency of health systems.❞
~ Dr. Peter Small, CMO, Hyfe
How does it do it?
Hyfe’s AI monitors the number of times a person coughs and the sound of the cough through any smartphone or other smart device.
This data collected over time provides increasingly more reliable information than a single visit to the doctor! By constantly listening and analyzing, it can detect patterns that might otherwise go unnoticed.
How big is this “big data” effort?
Hyfe maintains the largest cough dataset in the world. This means it can compare the sound of a patient’s cough with more than 400 million cough-like sounds from 83 countries across all continents.
The human brain doesn’t handle big numbers well. So, just to illustrate: if the average cough is 1 second long, that means it’d take more than 12 years to listen to them all.
Hyfe, meanwhile, can:
- listen to many things simultaneously
- index them all against user and location,
- use its ever-growing neural net to detect and illustrate patterns.
It’s so attentive, that it can learn to distinguish between different people’s coughs in the same household.
❝Companies like Google Health see even basic information such as getting an accurate count of the number of times a person coughs a day as a useful resource, and part of a larger need to collect and chronicle more health information to refine the way doctors diagnose disease and manage treatments in the future.❞
What are the public health implications?
The most obvious application is to note when there’s a spike in coughing, and see how such spikes grow and spread (if they do), to inform of contagion risks.
Another is to cross-reference it with data about local environmental allergens. Knowing how things like pollution and even pollen affect individuals differently could be helpful in identifying (and managing) chronic conditions like asthma.
What are the private health implications?
❝It’s going to transform the whole clinical approach for this common and chronic symptom. Patients will come in, have the data on how much they are coughing, and the physician can suggest a treatment based on that information to see if it makes the coughs better❞
~ Dr. Peter Small
Dr. Small’s colleague Dr. Cai, speaking for Google Health on this project, sees even more utility for diagnostics:
❝When I was in medical school, never ever did they teach us that we could listen to somebody cough and identify whether that person has TB (tuberculosis), COPD, or a tumor. But I keep seeing more and more studies of people coughing into a microphone, and an algorithm can detect whether somebody has TB with 95% specificity and sensitivity, or if someone has pneumonia or an exacerbation of COPD❞
~ Dr. Lawrence Cai
And the privacy implications?
Perhaps you don’t quite fancy the idea of not being able to cough without Google knowing about it. Hyfe’s software is currently opt-in, but…
If you cough near someone else’s Hyfe app, their app will recognize you’re not the app’s user, and start building a profile for you. Of course, that won’t be linked to your name, email address, or other IDs, as it would if you were the app’s user.
Hyfe will ask to connect to your social media, to collect more information about you and your friends.
Whether you’d like to try this or perhaps you’re just curious to learn more about this fascinating project, you can check out:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Modern Art and Science of Mobility – by Aurélien Broussal-Derval
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed mobility books before, so what makes this one stand out?
We’ll be honest: the illustrations are lovely.
The science, the information, the exercises, the routines, the programs… All these things are excellent too, but these can be found in many a book.
What can’t usually be found is very beautiful (yet no less clear) watercolor paintings and charcoal sketches as anatomical illustrations.
There are photos too (also of high quality), but the artistry of the paintings and sketches is what makes the reader want to spend time perusing the books.
At least, that’s what this reviewer found! Because it’s all very well having access to a lot of information (and indeed, I read so much), but making it enjoyable increases the chances of rereading it much more often.
As for the rest of the content, the book’s information is divided in categories:
- Pain (what causes it, what it means, and how to manage it)
- Breathing (yes, a whole section devoted to this, and it is aligned heavily to posture also, as well as psychological state and the effect of stress on tension, inflammation, and more)
- Movement (this is mostly about kinds of movement and ranges of movement)
- Mobility (this is about aggregating movements as a fully mobile human)
So, each builds on from the previous because any pain needs addressing before anything else, breathing (and with it, posture) comes next, then we learn about movement, then we bring it all together for mobility.
Bottom line: this is a beautiful and comprehensive book that will make learning a joy
Click here to check out The Modern Art and Science of Mobility, and learn and thrive!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: