What’s the difference between ‘strep throat’ and a sore throat? We’re developing a vaccine for one of them
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s the difference? is a new editorial product that explains the similarities and differences between commonly confused health and medical terms, and why they matter.
It’s the time of the year for coughs, colds and sore throats. So you might have heard people talk about having a “strep throat”.
But what is that? Is it just a bad sore throat that goes away by itself in a day or two? Should you be worried?
Here’s what we know about the similarities and differences between strep throat and a sore throat, and why they matter.

How are they similar?
It’s difficult to tell the difference between a sore throat and strep throat as they look and feel similar.
People usually have a fever, a bright red throat and sometimes painful lumps in the neck (swollen lymph nodes). A throat swab can help diagnose strep throat, but the results can take a few days.
Thankfully, both types of sore throat usually get better by themselves.
How are they different?
Most sore throats are caused by viruses such as common cold viruses, the flu (influenza virus), or the virus that causes glandular fever (Epstein-Barr virus).
These viral sore throats can occur at any age. Antibiotics don’t work against viruses so if you have a viral sore throat, you won’t get better faster if you take antibiotics. You might even have some unwanted antibiotic side-effects.
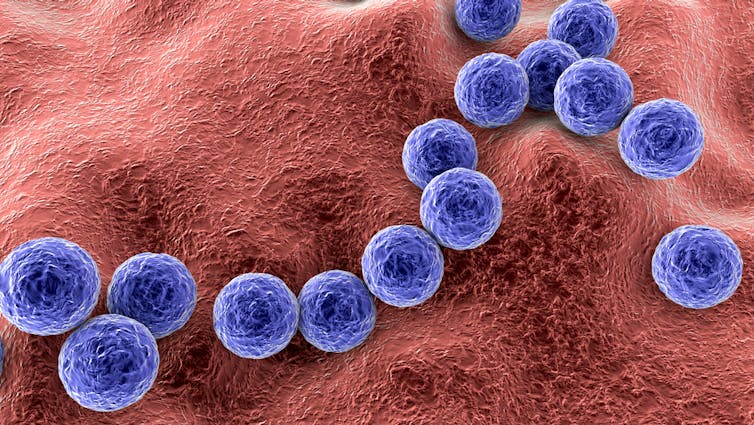
But strep throat is caused by Streptococcus pyogenes bacteria, also known as strep A. Strep throat is most common in school-aged children, but can affect other age groups. In some cases, you may need antibiotics to avoid some rare but serious complications.
In fact, the potential for complications is one key difference between a viral sore throat and strep throat.
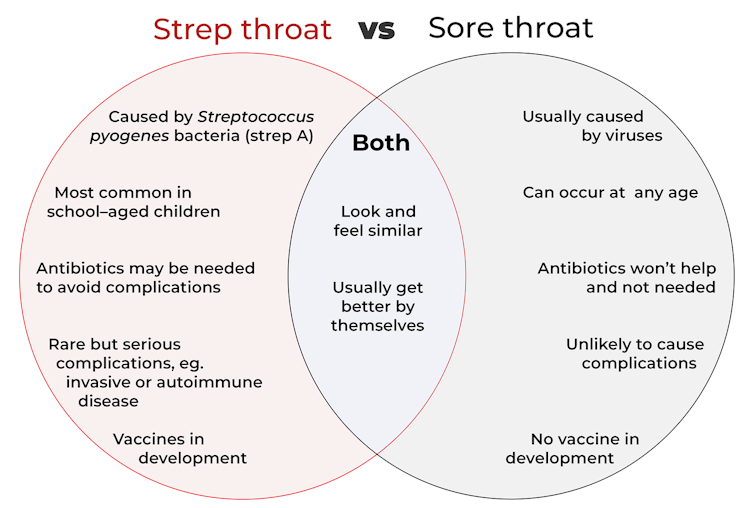
Generally, a viral sore throat is very unlikely to cause complications (one exception is those caused by Epstein-Barr virus which has been associated with illnesses such as chronic fatigue syndrome, multiple sclerosis and certain cancers).
But strep A can cause invasive disease, a rare but serious complication. This is when bacteria living somewhere on the body (usually the skin or throat) get into another part of the body where there shouldn’t be bacteria, such as the bloodstream. This can make people extremely sick.
Invasive strep A infections and deaths have been rising in recent years around the world, especially in young children and older adults. This may be due to a number of factors such as increased social mixing at this stage of the COVID pandemic and an increase in circulating common cold viruses. But overall the reasons behind the increase in invasive strep A infections are not clear.
Another rare but serious side effect of strep A is autoimmune disease. This is when the body’s immune system makes antibodies that react against its own cells.
The most common example is rheumatic heart disease. This is when the body’s immune system damages the heart valves a few weeks or months after a strep throat or skin infection.
Around the world more than 40 million people live with rheumatic heart disease and more than 300,000 die from its complications every year, mostly in developing countries.
However, parts of Australia have some of the highest rates of rheumatic heart disease in the world. More than 5,300 Indigenous Australians live with it.
Why do some people get sicker than others?
We know strep A infections and rheumatic heart disease are more common in low socioeconomic communities where poverty and overcrowding lead to increased strep A transmission and disease.
However, we don’t fully understand why some people only get a mild infection with strep throat while others get very sick with invasive disease.
We also don’t understand why some people get rheumatic heart disease after strep A infections when most others don’t. Our research team is trying to find out.
How about a vaccine for strep A?
There is no strep A vaccine but many groups in Australia, New Zealand and worldwide are working towards one.
For instance, Murdoch Children’s Research Institute and Telethon Kids Institute have formed the Australian Strep A Vaccine Initiative to develop strep A vaccines. There’s also a global consortium working towards the same goal.
Companies such as Vaxcyte and GlaxoSmithKline have also been developing strep A vaccines.
What if I have a sore throat?
Most sore throats will get better by themselves. But if yours doesn’t get better in a few days or you have ongoing fever, see your GP.
Your GP can examine you, consider running some tests and help you decide if you need antibiotics.
Kim Davis, General paediatrician and paediatric infectious diseases specialist, Murdoch Children’s Research Institute; Alma Fulurija, Immunologist and the Australian Strep A Vaccine Initiative project lead, Telethon Kids Institute, and Myra Hardy, Postdoctoral Researcher, Infection, Immunity and Global Health, Murdoch Children’s Research Institute
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Ricezempic: is there any evidence this TikTok trend will help you lose weight?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you spend any time looking at diet and lifestyle content on social media, you may well have encountered a variety of weight loss “hacks”.
One of the more recent trends is a home-made drink called ricezempic, made by soaking uncooked rice and then straining it to drink the leftover starchy water. Sounds delicious, right?
Its proponents claim it leads to weight loss by making you feel fuller for longer and suppressing your appetite, working in a similar way to the sought-after drug Ozempic – hence the name.
So does this drink actually mimic the weight loss effects of Ozempic? Spoiler alert – probably not. But let’s look at what the evidence tells us.
New Africa/Shutterstock How do you make ricezempic?
While the recipe can vary slightly depending on who you ask, the most common steps to make ricezempic are:
- soak half a cup of white rice (unrinsed) in one cup of warm or hot water up to overnight
- drain the rice mixture into a fresh glass using a strainer
- discard the rice (but keep the starchy water)
- add the juice of half a lime or lemon to the starchy water and drink.
TikTokers advise that best results will happen if you drink this concoction once a day, first thing in the morning, before eating.
The idea is that the longer you consume ricezempic for, the more weight you’ll lose. Some claim introducing the drink into your diet can lead to a weight loss of up to 27 kilograms in two months.
Resistant starch
Those touting ricezempic argue it leads to weight loss because of the resistant starch rice contains. Resistant starch is a type of dietary fibre (also classified as a prebiotic). There’s no strong evidence it makes you feel fuller for longer, but it does have proven health benefits.
Studies have shown consuming resistant starch may help regulate blood sugar, aid weight loss and improve gut health.
Research has also shown eating resistant starch reduces the risk of obesity, diabetes, heart disease and other chronic diseases.
Ricezempic is made by soaking rice in water. Kristi Blokhin/Shutterstock Resistant starch is found in many foods. These include beans, lentils, wholegrains (oats, barley, and rice – particularly brown rice), bananas (especially when they’re under-ripe or green), potatoes, and nuts and seeds (particularly chia seeds, flaxseeds and almonds).
Half a cup of uncooked white rice (as per the ricezempic recipe) contains around 0.6 grams of resistant starch. For optimal health benefits, a daily intake of 15–20 grams of resistant starch is recommended. Although there is no concrete evidence on the amount of resistant starch that leaches from rice into water, it’s likely to be significantly less than 0.6 grams as the whole rice grain is not being consumed.
Ricezempic vs Ozempic
Ozempic was originally developed to help people with diabetes manage their blood sugar levels but is now commonly used for weight loss.
Ozempic, along with similar medications such as Wegovy and Trulicity, is a glucagon-like peptide-1 (GLP-1) receptor agonist. These drugs mimic the GLP-1 hormone the body naturally produces. By doing so, they slow down the digestive process, which helps people feel fuller for longer, and curbs their appetite.
While the resistant starch in rice could induce some similar benefits to Ozempic (such as feeling full and therefore reducing energy intake), no scientific studies have trialled ricezempic using the recipes promoted on social media.
Ozempic has a long half-life, remaining active in the body for about seven days. In contrast, consuming one cup of rice provides a feeling of fullness for only a few hours. And simply soaking rice in water and drinking the starchy water will not provide the same level of satiety as eating the rice itself.
Other ways to get resistant starch in your diet
There are several ways to consume more resistant starch while also gaining additional nutrients and vitamins compared to what you get from ricezempic.
1. Cooked and cooled rice
Letting cooked rice cool over time increases its resistant starch content. Reheating the rice does not significantly reduce the amount of resistant starch that forms during cooling. Brown rice is preferable to white rice due to its higher fibre content and additional micronutrients such as phosphorus and magnesium.
2. More legumes
These are high in resistant starch and have been shown to promote weight management when eaten regularly. Why not try a recipe that has pinto beans, chickpeas, black beans or peas for dinner tonight?
3. Cooked and cooled potatoes
Cooking potatoes and allowing them to cool for at least a few hours increases their resistant starch content. Fully cooled potatoes are a rich source of resistant starch and also provide essential nutrients like potassium and vitamin C. Making a potato salad as a side dish is a great way to get these benefits.
In a nutshell
Although many people on social media have reported benefits, there’s no scientific evidence drinking rice water or “ricezempic” is effective for weight loss. You probably won’t see any significant changes in your weight by drinking ricezempic and making no other adjustments to your diet or lifestyle.
While the drink may provide a small amount of resistant starch residue from the rice, and some hydration from the water, consuming foods that contain resistant starch in their full form would offer significantly more nutritional benefits.
More broadly, be wary of the weight loss hacks you see on social media. Achieving lasting weight loss boils down to gradually adopting healthy eating habits and regular exercise, ensuring these changes become lifelong habits.
Emily Burch, Accredited Practising Dietitian and Lecturer, Southern Cross University and Lauren Ball, Professor of Community Health and Wellbeing, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Food Expiration Dates Don’t Mean What Most People Think They Mean
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Have you ever wondered why rock salt that formed during the Precambrian era has a label on it saying that it expires next month? To take something more delicate, how about eggs that expire next Thursday; isn’t that oddly specific for something that is surely affected by many variables? What matters, and what doesn’t?
Covering their assets
The US in particular wastes huge amounts of food, with 37% of food waste coming from households. Confusion over date labels is a major contributor, accounting for 20% of household food waste. Many people misinterpret these labels, often discarding food that is still safe to eat—which is good for the companies selling the food, because then they get to sell you more.
Date labels were introduced in the 70s with the “open dating” system to indicate optimal freshness, not safety. These dates are often conservative, set by manufacturers to ensure food is consumed at its best quality and encourage repeat purchases. However, many foods remain safe well past their labeled dates, including shelf-stable items like pasta, rice, and canned goods, as well as frozen foods stored properly.
Some foods do pose safety risks, especially meat and dairy products, as well as many grain-based foods, all of which which can harbor harmful bacteria. Infant formula labels are strictly regulated for safety. However, most date labels are not linked to health risks, leading to unnecessary waste.
When it comes down to it, our senses of sight, smell, and taste are more reliable than dates on packaging. Some quick pointers and caveats:
- If it has changed color in some way that’s not associated with a healthily ripening fruit or vegetable, that’s probably bad
- If it is moldy, that’s probably bad (but the degree of badness varies from food to food; see the link beneath today’s video for more on that)
- If a container has developed droplets of water on the inside when it didn’t have those before, that’s probably bad (it means something is respiring, and is thus alive, that probably shouldn’t be)
- If it smells bad, that’s probably bad—however this is not a good safety test, because a bad smell may often mean you are inhaling mold spores, which are not good for your lungs.
- If it tastes different than that food usually does, that’s probably bad (especially if it became bitter, pungent, tangy, sour, or cheesy, and does nor normally taste that way).
Some places have trialled clearer labelling, for example a distinction between “expires” and merely “best before”, but public awareness about the distinction is low. Some places have trialled removing dates entirely, to oblige the consumer to use their own senses instead. This is good for the seller in a different way than household food waste is, because it means the seller will have less in-store waste (because they can still sell something that might previously have been labelled as expired).
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
-
Be Your Future Self Now – by Dr. Benjamin Hardy
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Affirmations in the mirror are great and all, but they can only get you so far! And if you’re a regular reader of our newsletter, you probably know about the power of small daily habits adding up and compounding over time. So what does this book offer, that’s different?
“Be Your Future Self Now” beelines the route “from here to there”, with a sound psychological approach. On which note…
The book’s subtitle mentions “the science of intentional transformation”, and while Dr. Hardy is a psychologist, he’s an organizational psychologist (which doesn’t really pertain to this topic). It’s not a science-heavy book, but it is heavy on psychological rationality.
Where Dr. Hardy does bring psychology to bear, it’s in large part that! He teaches us how to overcome our biases that cause us to stumble blindly into the future… rather than intentfully creating our own future to step into. For example:
Most people (regardless of age!) acknowledge what a different person they were 10 years ago… but assume they’ll be basically the same person 10 years from now as they are today, just with changed circumstances.
Radical acceptance of the inevitability of change is the first step to taking control of that change.
That’s just one example, but there are many, and this is a book review not a book summary!
In short: if you’d like to take much more conscious control of the direction your life will take, this is a book for you.
Click here to get your copy of “Be Your Future Self Now” from Amazon!
Share This Post
Related Posts
-
What Are The “Bright Lines” Of Bright Line Eating?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is Dr. Susan Thompson. She’s a cognitive neuroscientist who has turned her hand to helping people to lose weight and maintain it at a lower level, using psychology to combat overeating. She is the founder of “Bright Line Eating”.
We’ll say up front: it’s not without some controversy, and we’ll address that as we go, but we do believe the ideas are worth examining, and then we can apply them or not as befits our personal lives.
What does she want us to know?
Bright Line Eating’s general goal
Dr. Thompson’s mission statement is to help people be “happy, thin, and free”.
You will note that this presupposes thinness as desirable, and presumes it to be healthy, which frankly, it’s not for everyone. Indeed, for people over a certain age, having a BMI that’s slightly into the “overweight” category is a protective factor against mortality (which is partly a flaw of the BMI system, but is an interesting observation nonetheless):
When BMI Doesn’t Quite Measure Up
Nevertheless, Dr. Thompson makes the case for the three items (happy, thin, free) coming together, which means that any miserable or unhealthy thinness is not what the approach is valuing, since it is important for “thin” to be bookended by “happy” and “free”.
What are these “bright lines”?
Bright Line Eating comes with 4 rules:
- No flour (no, not even wholegrain flour; enjoy whole grains themselves yes, but flour, no)
- No sugar (and as a tag-along to this, no alcohol) (sugars naturally found in whole foods, e.g. the sugar in an apple if eating an apple, is ok, but other kinds are not, e.g. foods with apple juice concentrate as a sweetener; no “natural raw cane sugar” etc is not allowed either; despite the name, it certainly doesn’t grow on the plant like that)
- No snacking, just three meals per day(not even eating the ingredients while cooking—which also means no taste-testing while cooking)
- Weigh all your food (have fun in restaurants—but more seriously, the idea here is to plan each day’s 3 meals to deliver a healthy macronutrient balance and a capped calorie total).
You may be thinking: “that sounds dismal, and not at all bright and cheerful, and certainly not happy and free”
The name comes from the idea that these rules are lines that one does not cross. They are “bright” lines because they should be observed with a bright and cheery demeanour, for they are the rules that, Dr. Thompson says, will make you “happy, thin, and free”.
You will note that this is completely in opposition to the expert opinion we hosted last week:
What Flexible Dieting Really Means
Dr. Thompson’s position on “freedom” is that Bright Line Eating is “very structured and takes a liberating stand against moderation”
Which may sound a bit of an oxymoron—is she really saying that we are going to be made free from freedom?
But there is some logic to it, and it’s about the freedom from having to make many food-related decisions at times when we’re likely to make bad ones:
Where does the psychology come in?
Dr. Thompson’s position is that willpower is a finite, expendable resource, and therefore we should use it judiciously.
So, much like Steve Jobs famously wore the same clothes every day because he had enough decisions to make later in the day that he didn’t want unnecessary extra decisions to make… Bright Line Eating proposes that we make certain clear decisions up front about our eating, so then we don’t have to make so many decisions (and potentially the wrong decisions) later when hungry.
You may be wondering: ”doesn’t sticking to what we decided still require willpower?”
And… Potentially. But the key here is shutting down self-negotiation.
Without clear lines drawn in advance, one must decide, “shall I have this cake or not?”, perhaps reflecting on the pros and cons, the context of the situation, the kind of day we’re having, how hungry we are, what else there is available to eat, what else we have eaten already, etc etc.
In short, there are lots of opportunities to rationalize the decision to eat the cake.
With clear lines drawn in advance, one must decide, “shall I have this cake or not?” and the answer is “no”.
So while sticking to that pre-decided “no” still may require some willpower, it no longer comes with a slew of tempting opportunities to rationalize a “yes”.
Which means a much greater success rate, both in adherence and outcomes. Here’s an 8-week interventional study and 2-year follow-up:
Bright Line Eating | Research Publications
Counterpoint: pick your own “bright lines”
Dr. Thompson is very keen on her 4 rules that have worked for her and many people, but she recognizes that they may not be a perfect fit for everyone.
So, it is possible to pick and choose our own “bright lines”; it is after all a dietary approach, not a religion. Here’s her response to someone who adopted the first 3 rules, but not the 4th:
Bright Lines as Guidelines for Weight Loss
The most important thing for Bright Line Eating, therefore, is perhaps the action of making clear decisions in advance and sticking to them, rather than seat-of-the-pantsing our diet, and with it, our health.
Want to know more from Dr. Thompson?
You might like her book, which we reviewed a while ago:
Bright Line Eating – by Dr. Susan Peirce Thompson
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Feel-Good Productivity – by Dr. Ali Abdaal
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Rise and grind” is not a sustainable way to live. Yet for most of us, there are things we do have to do every day that we don’t necessarily do for fun. So, how to be productive with those things, and not feel like we are constantly compromising and sacrificing our time on this earth for some intrinsically trivial but extrinsically required activity that’ll be forgotten tomorrow?
And most of us do also have dreams and ambitions (and if you don’t, then what were they before life snatched them away from you?), things to work towards. So there is “carrot” for us as well as “stick”. But how to break the cycle and get more carrot and less stick, while being more productive than before?
Dr. Abdaal frames this principally in terms of neurology first, psychology next.
That when we are bored, we simply do not have the neurochemicals required to work well anyway, so addressing that first needs to be a priority. He lays out many ways of doing this, gives lots of practical tips, and brings attention to the ways it’s easy to go wrong (and how to fix those too).
The writing style isdeceptively relaxed and casual, leading the reader smoothly into understanding of each topic before moving on.
Bottom line: if you want to get more done while feeling better about it (not a tired wreck), then this is the book for you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Unprocessed – by Kimberly Wilson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this is not: hundreds of pages to say “eat less processed food”. That is, of course, also advisable (and indeed, is advised in the book too), but there’s a lot more going on here too.
Though not a doctor, the author is a psychologist who brings a lot of data to the table, especially when it comes to the neurophysiology at hand, what forgotten micronutrients many people are lacking, and what trends in society worsen these deficiencies in the population at large.
If you only care about the broadest of take-away advice, it is: eat a diet that’s mostly minimally processed plants and some oily fish, watch out for certain deficiencies in particular, and increase dietary intake of them where necessary (with taking supplements as a respectable next-best remedy).
On which note, a point of criticism is that there’s some incorrect information about veganism and brain health; she mentions that DHA is only found in fish (in fact, fish get it from algae, which has it, and is the basis of many vegan omega-3 supplements), and the B12 is found only in animals (also found in yeast, which is not an animal, as well as various bacteria in soil, and farm animals get their B12 from supplements these days anyway, so it is arguable that we could keep things simpler by just cutting out the middlecow).
However, the strength of this book really is in the delivery of understanding about why certain things matter. If you’re told “such-and-such is good for the brain”, you’ll up your intake for 1–60 days, depending on whether you bought a supermarket item or ordered a batch of supplements. And then you’ll forget, until 6–12 months later, and you’ll do it again. On the other hand, if you understand how something is good or bad for the brain, what it does (for good or ill) on a cellular level, the chemistry and neurophysiology at hand, you’ll make new habits for life.
The style is middle-range pop-science; by this we mean there are tables of data and some long words that are difficult to pronounce, but also it’s not just hard science throughout—there’s (as one might expect from an author who is a psychologist) a lot about the psychology and sociology of why many people make poor dietary decisions, and the things governments often do (or omit doing) that affect this adversely—and how we can avoid those traps as individuals (unless we be incarcerated or such).
As an aside, the author is British, so governmental examples are mostly UK-based, but it doesn’t take a lot to mentally measure that against what the governments of, for example, the US or Canada do the same or differently.
Bottom line: there’s a lot of great information about brain health here; the strongest parts are whether the author stays within her field (psychology encompasses such diverse topics as neurophysiology and aspects of sociology, but not microbiology, for example). If you want to learn about the physiology of brain health and enjoy quite a sociopolitical ride along the way, this one’s a good one for that.
Click here to check out Unprocessed, and make the best choices for you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: