Freekeh Tomato Feast
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Fiber-dense freekeh stars in this traditional Palestinian dish, and the whole recipe is very gut-healthy, not to mention delicious and filling, as well as boasting generous amounts of lycopene and other phytonutrients:
You will need
- 1 cup dried freekeh (if avoiding gluten, substitute a gluten-free grain, or pseudograin such as buckwheat; if making such a substitution, then also add 1 tbsp nutritional yeast—for the flavor as well as the nutrients)
- 1 medium onion, thinly sliced
- 1 2oz can anchovies (if vegan/vegetarian, substitute 1 can kimchi)
- 1 14oz can cherry tomatoes
- 1 cup halved cherry tomatoes, fresh
- ½ cup black olives, pitted
- 1 5oz jar roasted peppers, chopped
- ½ bulb garlic, thinly sliced
- 2 tsp black pepper
- 1 tsp chili flakes
- 1 sprig fresh thyme
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Place a heavy-based (cast iron, if you have it) sauté pan over a medium heat. Add some olive oil, then the onion, stirring for about 5 minutes.
2) Add the anchovies, herbs and spices (including the garlic), and stir well to combine. The anchovies will probably soon melt into the onion; that’s fine.
3) Add the canned tomatoes (but not the fresh), followed by the freekeh, stirring well again to combine.
4) Add 2 cups boiling water, and simmer with the lid on for about 40 minutes. Stir occasionally and check the water isn’t getting too low; top it up if it’s getting dry and the freekeh isn’t tender yet.
5) Add the fresh chopped cherry tomatoes and the chopped peppers from the jar, as well as the olives. Stir for just another 2 minutes, enough to let the latest ingredients warm through.
6) Serve, adding a garnish if you wish:

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Eat More (Of This) For Lower Blood Pressure
- Making Friends With Your Gut (You Can Thank Us Later)
- Lycopene’s Benefits For The Gut, Heart, Brain, & More
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Eating Disorders: More Varied (And Prevalent) Than People Think
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Disordered Eating Beyond The Stereotypes
Around 10% of Americans* have (or have had) an eating disorder. That might not seem like a high percentage, but that’s one in ten; do you know 10 people? If so, it might be a topic that’s near to you.
*Source: Social and economic cost of eating disorders in the United States of Americ
Our hope is that even if you yourself have never had such a problem in your life, today’s article will help arm you with knowledge. You never know who in your life might need your support.
Very misunderstood
Eating disorders are so widely misunderstood in so many ways that we nearly made this a Friday Mythbusting edition—but we preface those with a poll that we hope to be at least somewhat polarizing or provide a spectrum of belief. In this case, meanwhile, there’s a whole cluster of myths that cannot be summed up in one question. So, here we are doing a Psychology Sunday edition instead.
“Eating disorders aren’t that important”
Eating disorders are the second most deadly category of mental illness, second only to opioid addiction.
Anorexia specifically has the highest case mortality rate of any mental illness:
Source: National Association of Anorexia Nervosa & Associated Disorders: Eating Disorder Statistics
So please, if someone needs help with an eating disorder (including if it’s you), help them.
“Eating disorders are for angsty rebellious teens”
While there’s often an element of “this is the one thing I can control” to some eating disorders (including anorexia and bulimia), eating disorders very often present in early middle-age, very often amongst busy career-driven individuals using it as a coping mechanism to have a feeling of control in their hectic lives.
13% of women over 50 report current core eating disorder symptoms, and that is probably underreported.
Source: as above; scroll to near the bottom!
“Eating disorders are a female thing”
Nope. Officially, men represent around 25% of people diagnosed with eating disorders, but women are 5x more likely to get diagnosed, so you can do the math there. Women are also 1.5% more likely to receive treatment for it.
By the time men do get diagnosed, they’ve often done a lot more damage to their bodies because they, as well as other people, have overlooked the possibility of their eating being disordered, due to the stereotype of it being a female thing.
Source: as above again!
“Eating disorders are about body image”
They can be, but that’s far from the only kind!
Some can be about control of diet, not just for the sake of controlling one’s body, but purely for the sake of controlling the diet itself.
Still yet others can be not about body image or control, like “Avoidant/Restrictive Food Intake Disorder”, which in lay terms sometimes gets dismissed as “being a picky eater” or simply “losing one’s appetite”, but can be serious.
For example, a common presentation of the latter might be a person who is racked with guilt and/or anxiety, and simply stops eating, because either they don’t feel they deserve it, or “how can I eat at a time like this, when…?” but the time is an ongoing thing so their impromptu fast is too.
Still yet even more others might be about trying to regulate emotions by (in essence) self-medicating with food—not in the healthy “so eat some fruit and veg and nuts etc” sense, but in the “Binge-Eating Disorder” sense.
And that latter accounts for a lot of adults.
You can read more about these things here:
Psychology Today | Types of Eating Disorder ← it’s pop-science, but it’s a good overview
Take care! And if you have, or think you might have, an eating disorder, know that there are organizations that can and will offer help/support in a non-judgmental fashion. Here’s the ANAD’s eating disorder help resource page, for example.
Share This Post

What Is Making The Ringing In Your Ears Worse?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Rachael Cook, an audiologist at Applied Hearing Solutions in Phoenix, Arizona, shares her professional insights into managing tinnitus.
If you’re unfamiliar with Tinnitus, it is an auditory condition characterized by a ringing, buzzing, or humming sound, and ffects nearly 10% of the population. We’ve written on Tinnitus, and how it can disrupt your life, in this article.
Key Triggers for Tinnitus
Several everyday habits can make your tinnitus louder. Caffeine and nicotine increase blood pressure, restricting blood flow to the cochlea and worsening tinnitus. Common medications, such as pain relievers, high-dose antibiotics, and antidepressants, can also exacerbate tinnitus, especially with higher or long-term dosages.
Impact of Diet and Sleep
Dietary choices significantly impact tinnitus. Alcohol and salt alter the fluid balance in the cochlea, increasing tinnitus perception. Alcohol changes blood flow patterns and neurotransmitter production, while high salt intake has similar effects. Poor sleep quality elevates stress levels, making it harder to ignore tinnitus signals. Addressing sleep disorders like sleep apnea and insomnia can help manage tinnitus symptoms.
Importance of Treating Hearing Loss
Untreated hearing loss worsens tinnitus. Nearly 90% of individuals with tinnitus have some hearing loss. Hearing aids can reduce tinnitus perception by restoring missing sounds and reducing the brain’s internal compensatory signals. Combining hearing aids with sound therapy is said to provide even greater relief.
Read more about hearing loss in our article on the topic.
Otherwise, for a great guide on managing tinnitus, we recommend watching Dr. Cook’s video:
Here’s hoping your ear’s aren’t ringing too much whilst watching the video!
Share This Post

Track Your Blood Sugars For Better Personalized Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There Will Be Blood
Are you counting steps? Counting calories? Monitoring your sleep? Heart rate zones? These all have their merits:
- Steps: One More Resource Against Osteoporosis!
- Calories: Is Cutting Calories The Key To Healthy Long Life?
- Sleep: A Head-To-Head Of Google and Apple’s Top Apps For Getting Your Head Down
- Heart Rate Zones: Heart Rate Zones, Oxalates, & More
About calories: this writer (it’s me, hi) opines that intermittent fasting has the same benefits as caloric restriction, without the hassle of counting, and is therefore superior. I also personally find fasting psychologically more pleasant. However, our goal here is to be informative, not prescriptive, and some people may have reasons to prefer CR to IF!
Examples that come to mind include ease of adherence in the case of diabetes management, especially Type 1, or if one’s schedule (and/or one’s “medications that need to be taken with food” schedule) does not suit IF.
And now for the blood…
A rising trend in health enthusiasts presently is the use of Continuous Glucose Monitors (CGMs), which do exactly what is sounds like they do: they continually monitor glucose. Specifically, the amount of it in your blood.
Of course, these have been in use in diabetes management for years; the technology is not new, but the application of the technology is.
A good example of what benefits a non-diabetic person can gain from the use of a CGM is Jessie Inchauspé, the food scientist of “Glucose Revolution” and “The Glucose Goddess Method” fame.
By wearing a CGM, she was able to notice what things did and didn’t spike her blood sugars, and found that a lot of the things were not stuff that people knew/advised about!
For example, much of diabetes management (including avoiding diabetes in the first place) is based around paying attention to carbs and little else, but she found that it made a huge difference what she ate (or didn’t) with the carbs. By taking many notes over the course of her daily life, she was eventually able to isolate these patterns, showed her working-out in The Glucose Revolution (there’s a lot of science in that book), and distilled that information into bite-size (heh) advice such as:
10 Ways To Balance Blood Sugars
That’s great, but since people like Inchauspé have done the work, I don’t have to, right?
You indeed don’t have to! But you can still benefit from it. For example, fastidious as her work was, it’s a sample size of one. If you’re not a slim white 32-year-old French woman, there may be some factors that are different for you.
All this to say: glucose responses, much like nutrition in general, are not a one-size-fits-all affair.
With a CGM, you can start building up your own picture of what your responses to various foods are like, rather than merely what they “should” be like.
This, by the way, is also one of the main aims of personalized health company ZOE, which crowdsourced a lot of scientific data about personalized metabolic responses to standardized meals:
Not knowing these things can be dangerous
We don’t like to scaremonger here, but we do like to point out potential dangers, and in this case, blindly following standardized diet advice, if your physiology is not standard, can have harmful effects, see for example:
Diabetic-level glucose spikes seen in non-diabetic people
Where can I get a CGM?
We don’t sell them, and neither does Amazon, but you can check out some options here:
The 4 Best CGM Devices For Measuring Blood Sugar in 2024
…and if your doctor is not obliging with a prescription, note that the device that came out top in the above comparisons, will be available OTC soon:
The First OTC Continuous Glucose Monitor Will Be Available Summer 2024
Take care!
Share This Post
Related Posts

The Path To Revenue – by Theresa Marcroft
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
So many books about start-ups skip right over the elephant in the room: survivorship bias. Not so for Marcroft! This book contains the most comprehensive and unapologetic treatment of it we’ve seen.
Less “here’s what Steve Jobs did right and here’s what Chocolate-Teapots-For-Dogs-R-Us did wrong; don’t mess up that badly and you’ll be fine”… and more realism. Marcroft gives us a many-angled critical analytic approach. In it, she examines why many things can seem similar in both content and presentation… but can cause growth or failure (and how and why), based on more than anecdotes and luck.
The book is information-dense (taking a marketing-centric approach) and/but well-presented in a very readable format.
If we can find any criticism of the book, it’s less about what’s in it and more about what’s not in it. This can never be a “your start-up bible!” book because it’s not comprehensive. It doesn’t cover assembling your team, for example. Nor does it give a lot of attention to management, preferring to focus on strategy.
But no single book can be all things, and we highly recommend this one—the marketing advice alone is more than worth the cost of the book!
Take Your First Step Along The Path To Revenue By Checking It Out On Amazon!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Stop Pain Spreading
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Put Your Back Into It (Or Don’t)!
We’ve written before about Managing Chronic Pain (Realistically!), and today we’re going to tackle a particular aspect of chronic pain management.
- It’s a thing where the advice is going to be “don’t do this”
- And if you have chronic pain, you will probably respond “yep, I do that”
However, it’s definitely a case of “when knowing isn’t the problem”, or at the very least, it’s not the whole problem.
Stop overcompensating and address the thing directly
We all do it, whether in chronic pain, or just a transient injury. But we all need to do less of it, because it causes a lot of harm.
Example: you have pain in your right knee, so you sit, stand, walk slightly differently to try to ease that pain. It works, albeit marginally, at least for a while, but now you also have pain in your left hip and your lumbar vertebrae, because of how you leaned a certain way. You adjust how you sit, stand, walk, to try to ease both sets of pain, and before you know it, now your neck also hurts, you have a headache, and you’re sure your digestion isn’t doing what it should and you feel dizzy when you stand. The process continues, and before long, what started off as a pain in one knee has now turned your whole body into a twisted aching wreck.
What has happened: the overcompensation due to the original pain has unduly stressed a connected part of the body, which we then overcompensate for somewhere else, bringing down the whole body like a set of dominoes.
For more on this: Understanding How Pain Can Spread
“Ok, but how? I can’t walk normally on that knee!”
We’re keeping the knee as an example here, but please bear in mind it could be any chronic pain and resultant disability.
Note: if you found the word “disability” offputting, please remember: if it adversely affects your abilities, it is a disability. Disabilities are not something that only happen to other people! They will happen to most of us at some point!
Ask yourself: what can you do, and what can’t you do?
For example:
- maybe you can walk, but not normally
- maybe you can walk normally, but not without great pain
- maybe you can walk normally, but not at your usual walking pace
First challenge: accept your limitations. If you can’t walk at your usual walking pace without great pain and/or throwing your posture to the dogs, then walk more slowly. To Hell with societal expectations that it shouldn’t take so long to walk from A to B. Take the time you need.
Second challenge: accept help. It doesn’t have to be help from another person (although it could be). It might be accepting the help of a cane, or maybe even a wheelchair for “flare-up” days. Society, especially American society which is built on ideas of self-sufficiency, has framed a lot of such options as “giving up”, but if they help you get about your day while minimizing doing further harm to your body, then they can be good and even health-preserving things. Same goes for painkillers if they help you from doing more harm to your body by balling up tension in a part of your body in a way that ends up spreading out and laying ruin to your whole body.
Speaking of which:
How Much Does It Hurt? Get The Right Help For Your Pain
After which, you might want to check out:
The 7 Approaches To Pain Management
and
Science-Based Alternative Pain Relief
Third challenge: deserves its own section, so…
Do what you can
If you have chronic pain (or any chronic illness, really), you are probably fed up of hearing how this latest diet will fix you, or yoga will fix you, and so on. But, while these things may not be miracle cures…
- A generally better diet really will lessen symptoms and avoid flare-ups (a low-inflammation diet is a great start for lessening the symptoms of a lot of chronic illnesses)
- Doing what exercise you can, being mindful of your limitations yes but still keeping moving as much as possible, will also prevent (or at least slow) deterioration. Consider consulting a physiotherapist for guidance (a doctor will more likely just say “rest, take it easy”, whereas a physiotherapist will be able to give more practical advice).
- Getting good sleep may be a nightmare in the case of chronic pain (or other chronic illnesses! Here’s to those late night hyperglycemia incidents for Type 1 Diabetics that then need monitoring for the next few hours while taking insulin and hoping it goes back down) but whatever you can do to prioritize it, do it.
Want to read more?
We reviewed a little while ago a great book about this; the title sounds like a lot of woo, but we promise the content is extremely well-referenced science:
…and if your issue is back pain specifically, we highly recommend:
Healing Back Pain: The Mind-Body Connection – by Dr. John Sarno
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

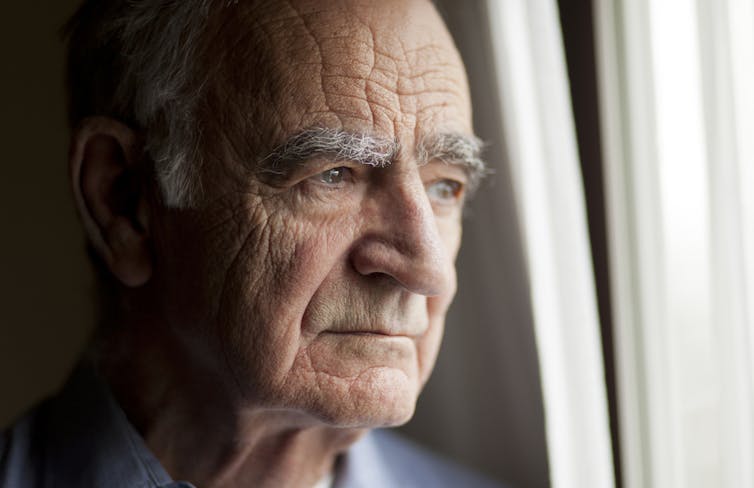
How do I handle it if my parent is refusing aged care? 4 things to consider
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s a shock when we realise our parents aren’t managing well at home.
Perhaps the house and garden are looking more chaotic, and Mum or Dad are relying more on snacks than nutritious meals. Maybe their grooming or hygiene has declined markedly, they are socially isolated or not doing the things they used to enjoy. They may be losing weight, have had a fall, aren’t managing their medications correctly, and are at risk of getting scammed.
You’re worried and you want them to be safe and healthy. You’ve tried to talk to them about aged care but been met with swift refusal and an indignant declaration “I don’t need help – everything is fine!” Now what?
Here are four things to consider.
1. Start with more help at home
Getting help and support at home can help keep Mum or Dad well and comfortable without them needing to move.
Consider drawing up a roster of family and friends visiting to help with shopping, cleaning and outings. You can also use home aged care services – or a combination of both.
Government subsidised home care services provide from one to 13 hours of care a week. You can get more help if you are a veteran or are able to pay privately. You can take advantage of things like rehabilitation, fall risk-reduction programs, personal alarms, stove automatic switch-offs and other technology aimed at increasing safety.
Call My Aged Care to discuss your options.

Is Mum or Dad OK at home?
Nadino/Shutterstock2. Be prepared for multiple conversations
Getting Mum or Dad to accept paid help can be tricky. Many families often have multiple conversations around aged care before a decision is made.
Ideally, the older person feels supported rather than attacked during these conversations.
Some families have a meeting, so everyone is coming together to help. In other families, certain family members or friends might be better placed to have these conversations – perhaps the daughter with the health background, or the auntie or GP who Mum trusts more to provide good advice.
Mum or Dad’s main emotional support person should try to maintain their relationship. It’s OK to get someone else (like the GP, the hospital or an adult child) to play “bad cop”, while a different person (such as the older person’s spouse, or a different adult child) plays “good cop”.
3. Understand the options when help at home isn’t enough
If you have maximised home support and it’s not enough, or if the hospital won’t discharge Mum or Dad without extensive supports, then you may be considering a nursing home (also known as residential aged care in Australia).
Every person has a legal right to choose where we live (unless they have lost capacity to make that decision).
This means families can’t put Mum or Dad into residential aged care against their will. Every person also has the right to choose to take risks. People can choose to continue to live at home, even if it means they might not get help immediately if they fall, or eat poorly. We should respect Mum or Dad’s decisions, even if we disagree with them. Researchers call this “dignity of risk”.
It’s important to understand Mum or Dad’s point of view. Listen to them. Try to figure out what they are feeling, and what they are worried might happen (which might not be rational).
Try to understand what’s really important to their quality of life. Is it the dog, having privacy in their safe space, seeing grandchildren and friends, or something else?
Older people are often understandably concerned about losing independence, losing control, and having strangers in their personal space.
Sometimes families prioritise physical health over psychological wellbeing. But we need to consider both when considering nursing home admission.
Research suggests going into a nursing home temporarily increases loneliness, risk of depression and anxiety, and sense of losing control.
Mum and Dad should be involved in the decision-making process about where they live, and when they might move.
Some families start looking “just in case” as it often takes some time to find the right nursing home and there can be a wait.
After you have your top two or three choices, take Mum or Dad to visit them. If this is not possible, take pictures of the rooms, the public areas in the nursing home, the menu and the activities schedule.
We should give Mum or Dad information about their options and risks so they can make informed (and hopefully better) decisions.
For instance, if they visit a nursing home and the manager says they can go on outings whenever they want, this might dispel a belief they are “locked up”.
Having one or two weeks “respite” in a home may let them try it out before making the big decision about staying permanently. And if they find the place unacceptable, they can try another nursing home instead.

You might need to have multiple conversations about aged care.
CGN089/Shutterstock4. Understand the options if a parent has lost capacity to make decisions
If Mum or Dad have lost capacity to choose where they live, family may be able to make that decision in their best interests.
If it’s not clear whether a person has capacity to make a particular decision, a medical practitioner can assess for that capacity.
Mum or Dad may have appointed an enduring guardian to make decisions about their health and lifestyle decisions when they are not able to.
An enduring guardian can make the decision that the person should live in residential aged care, if the person no longer has the capacity to make that decision themselves.
If Mum or Dad didn’t appoint an enduring guardian, and have lost capacity, then a court or tribunal can appoint that person a private guardian (usually a family member, close friend or unpaid carer).
If no such person is available to act as private guardian, a public official may be appointed as public guardian.
Deal with your own feelings
Families often feel guilt and grief during the decision-making and transition process.
Families need to act in the best interest of Mum or Dad, but also balance other caring responsibilities, financial priorities and their own wellbeing.

Lee-Fay Low, Professor in Ageing and Health, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: