What Happens Every Day When You Quit Sugar For 30 Days
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We all know that sugar isn’t exactly a health food, but it can be hard to quit. How long can cravings be expected to last, and when can we expect to see benefits? Today’s video covers the timeline in a realistic yet inspiring fashion:
What to expect on…
Day 1: expect cravings and withdrawal symptoms including headaches, fatigue, mood swings, and irritability—as well as tiredness, without the crutch of sugar.
Days 2 & 3: more of the same, plus likely objections from the gut, since your Candida albicans content will not be enjoying being starved of its main food source.
Days 4–7: reduction of the above symptoms, better energy levels, improved sleep, and likely the gut will be adapting or have adapted.
Days 8–14: beginning of weight loss, clearer skin, improved complexion; taste buds adapt too, making foods taste sweeter. Continued improvement in energy and focus, as well.
Days 15–21: more of the same improvements, plus the immune system will start getting stronger around now. But watch out, because there may still be some cravings from time to time.
Days 22–30: all of the above positive things, few or no cravings now, and enhanced metabolic health as a whole.
For more specificity on each of these stages, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
The Not-So-Sweet Science Of Sugar Addiction
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Anti-Inflammatory Cookbook for Beginners – by Melissa Jefferson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For some of us, avoiding inflammatory food is a particularly important consideration. For all of us, it should be anyway.
Sometimes, we know what’s good against inflammation, and we know what’s bad for inflammation… but we might struggle to come up with full meals of just-the-good, especially if we want to not repeat meals every day!
The subtitle is slightly misleading! It says “Countless Easy and Delicious Recipes”, but this depends on your counting ability. Melissa Jefferson gives us 150 anti-inflammatory recipes, which can be combined for a 12-week meal plan. We think that’s enough to at least call it “many”, though.
First comes an introduction to inflammation, inflammatory diseases, and a general overview of what to eat / what to avoid. After that, the main part of the book is divided into sections:
- Breakfasts (20)
- Soups (15)
- Beans & Grains (20)
- Meat (20)
- Fish (20)
- Vegetables (20)
- Sides (15)
- Snacks (10)
- Desserts (10)
If you’ve a knowledge of anti-inflammation diet already, you may be wondering how “Meat” and “Desserts” works.
- The meat section is a matter of going light on the meat and generally favoring white meats, and certainly unprocessed.
- Of course, if you are vegetarian or vegan, substitutions may be in order anyway.
As for the dessert section? A key factor is that fruits and chocolate are anti-inflammatory foods! Just a matter of not having desserts full of sugar, flour, etc.
The recipes themselves are simple and to-the-point, with ingredients, method, and nutritional values. Just the way we like it.
All in all, a fine addition to absolutely anyone’s kitchen library… And doubly so if you have a particular reason to focus on avoiding/reducing inflammation!
Get your copy of “Anti-Inflammatory Cookbook for Beginners” from Amazon today!
Share This Post
-
Health Simplified – by Daniel Cottmeyer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Health Simplified – by Daniel Cottmeyer
A lot of books focus on the most marketable aspects of health, such as fat loss or muscle gain. Instead, Cottmeyer takes a “birds-eye-view” of health in all its aspects, and then boils it down to the most critical key parts.
Rather than giving a science-dense tome that nobody reads, or a light motivational piece that everyone reads but it amounts to “you can do it!”, here we get substance… but in a digestible form.
Which we at 10almonds love.
The book presents a simple action plan to:
- Improve your relationship with food/exercise
- Actually get better sleep
- Understand how nutrition really works
- Set up helpful habits that are workable and sustainable
- Bring these components together synergistically
Bottom line: if you’re going to buy only one health/fitness book, this is a fine contender.
Share This Post
-
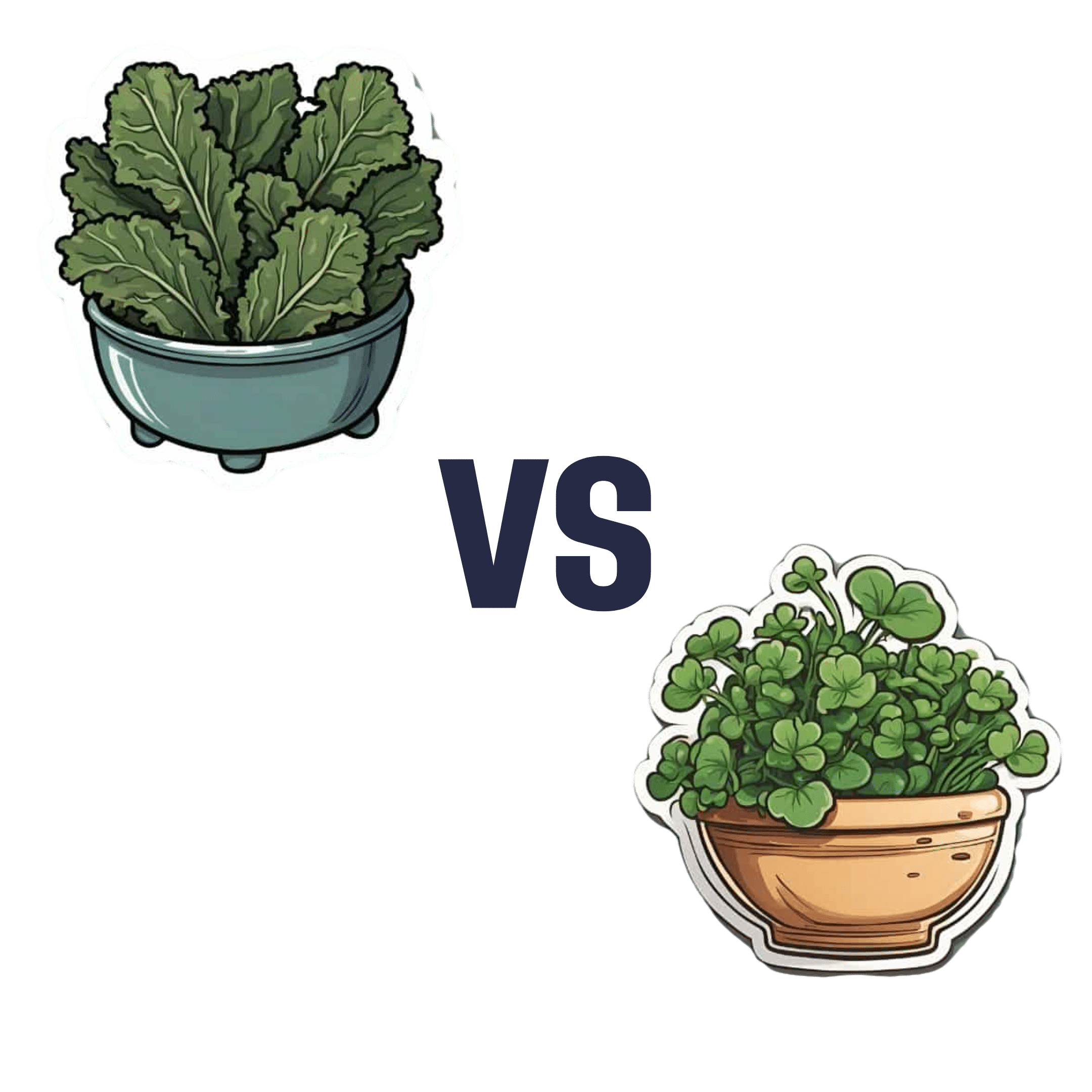
Spinach vs Kale – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing spinach to kale, we picked the spinach.
Why?
In terms of macros, spinach and kale are very similar. They are mostly water wrapped in fiber, with very small amounts of carbohydrates and protein and trace amounts of fat.
Spinach has a lot more vitamins and minerals—a wider variety, and in most cases, more of them.
Kale is notably higher in vitamin C, though. Everything else, spinach is higher or close to equal.
Spinach is especially notably a lot higher in B vitamins, as well as iron, calcium, magnesium, and zinc.
One downside to spinach, though, which is that it’s high in oxalates, which can increase the risk of kidney stones. If your kidneys are in good health and you eat spinach in moderation, this is not a problem for most people—but if your kidneys aren’t in good health (or you are, for whatever reason, consuming Popeye levels of spinach), you might consider switching to kale.
While spinach swept the board in most categories, kale remains a very good option too, and a diet diverse in many kinds of plants is usually best.
Want to learn more?
Spinach and kale are very both good sources of carotenoids; check out:
Enjoy!
Share This Post
Related Posts
-
The Good, The Bad, & The Vigorously Debated
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This week in health news sees some pretty varied topics:
One more reason to care about the gut-brain axis
Stroke is a top killer in much of the industrialized world, usually making it into the top-few list on a per-country basis. And, it’s rising in prevalence, too. This is partly because our longevity is increasing so age-related things kill us more often, statistically, than age-unrelated things. But that’s only part of the reason; another is that our lifestyle (on the national level) is becoming more conducive to stroke. Diet is a large contributor to that, and gut health has now been identified as a key factor.
What recent research has shown is that minutes after a stroke occurs, normal gut anatomy is disrupted, and cells responsible for gut barrier integrity are eroded, and bugs from the gut get into the blood, and arrive at the (newly damaged) brain vasculature, where the blood-brain barrier is often also compromised on account of the stroke.
Because of this, critical to reducing post-stroke neuroinflammation (something that makes stroke damage more severe and recovery a lot harder) is improving the gut’s ability to heal itself quickly.
This can be helped with a dose of Insulin-like Growth Factor (IGF-1), but there are other things that can help or hinder, and those other things are modifiable by us as individuals in our lifestyle choices (e.g. a gut-healthy diet with plenty of fiber, and avoiding gut-unhealthy things like sugar and alcohol that feed C. albicans growths that will put roots through your intestines and make holes as they do), because the better/worse your gut barrier integrity is to start with, the easier/harder it will be for your gut to repair itself quickly:
Read in full: Healing the gut can reduce long-term impact of stroke
Related: Stop Sabotaging Your Gut
How about that seasonal lead-spiced hot drink?
Lead contamination in ground spices has become a bit of an issue, ground turmeric has had quite some flak in this regard, and now the spotlight is on cinnamon.
These reports, by the way, do not specify what kind of cinnamon (i.e. cassia vs Ceylon), however, clicking through to assorted sources and then doing our own digging finds that all cinnamon products we found listed as contaminated, were cassia cinnamon. This is unsurprising, as a) it’s cheaper b) it’s the kind most readily found on shelves in the US. That said, when it comes to Ceylon (sweet) cinnamon, absence of evidence is not evidence of absence, so that doesn’t mean they got the all-clear on lead contamination, but rather, that they haven’t received the same scrutiny as yet.
It’s worth noting that cinnamon sticks have been found to have less contamination than ground cinnamon, though.
It’s also worth noting that since some adulterated products have had lead added deliberately in increase the weight and darken the color, this is more likely to happen to cassia cinnamon than sweet cinnamon because cassia cinnamon is visibly darker, so adding a darkening agent to sweet cinnamon would just make it look like cassia (which no seller would want to do since cassia is the cheaper of the two).
Read in full: Why lead-tainted cinnamon products have turned up on shelves, and what questions consumers should ask
Related: Sweet Cinnamon vs Regular Cinnamon – Which is Healthier? ← this also covers toxicity issues, by the way
A matter of life and death
Assisted dying is currently legal in 10/40 US states, and Canada. Over in the UK, it’s being debated (and voted on) in Parliament today, at time of writing.
While bodily autonomy discussions are usually quite straightforward arguments between the very separate camps of
- “my body, my choice” vs
- “they shouldn’t be allowed to do that”,
…this one comes with a considerable middleground, because
- “people should have to right to end things without extra suffering and on their own terms”, and
- “many disabled people fear being placed in a position of having justify why they are not exercising their right to die when it might be cheaper and easier for others if they did”
…are positions with a lot of potential overlap.
In any case, we know most of our readers are in the US, but with a 10/40 split in US states (and some recent controversies in Canada), it’s likely a topic that’ll come up for most people at some point, so it’s good to understand it, and this is as good an opportunity as any:
Read in full: How would the assisted dying bill work and what issues might it create?
Related: Managing Your Mortality ← this talks about psychological/social considerations, as well as end-of-life care, palliative care (which is not quite the same thing!) and euthanasia in various forms, including the unofficial kind that you might want to be aware of if you want to avoid that happening.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Truth About Statins – by Barbara H. Roberts, M.D.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
All too often, doctors looking to dispense a “quick fix” will prescribe from their playbook of a dozen or so “this will get you out of my office” drugs. Most commonly, things that treat symptoms rather than the cause. Sometimes, this can be fine! For example, in some cases, painkillers and antidepressants can make a big improvement to people’s lives. What about statins, though?
Prescribed to lower cholesterol, they broadly do exactly that. However…
Dr. Roberts wants us to know that we could be missing the big picture of heart health, and making a potentially fatal mistake.
This is not to say that the book argues that statins are necessarily terrible, or that they don’t have their place. Just, we need to understand what they will and won’t do, and make an informed choice.
To which end, she does advise regards when statins can help the most, and when they may not help at all. She also covers the questions to ask if your doctor wants to prescribe them. And—all so frequently overlooked—the important differences between men’s and women’s heart health, and the implications these have for the efficacy (or not) of statins.
With regard to the “alternatives to cholesterol-lowering drugs” promised in the subtitle… we won’t keep any secrets here:
Dr. Roberts (uncontroversially) recommends the Mediterranean diet. She also provides two weeks’ worth of recipes for such, in the final part of the book.
All in all, an important book to read if you or a loved one are taking, or thinking of taking, statins.
Pick up your copy of The Truth About Statins on Amazon today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Without Medicare Part B’s Shield, Patient’s Family Owes $81,000 for a Single Air-Ambulance Flight
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Without Medicare Part B’s Shield, Patient’s Family Owes $81,000 for a Single Air-Ambulance Flight
Debra Prichard was a retired factory worker who was careful with her money, including what she spent on medical care, said her daughter, Alicia Wieberg. “She was the kind of person who didn’t go to the doctor for anything.”
That ended last year, when the rural Tennessee resident suffered a devastating stroke and several aneurysms. She twice was rushed from her local hospital to Vanderbilt University Medical Center in Nashville, 79 miles away, where she was treated by brain specialists. She died Oct. 31 at age 70.
One of Prichard’s trips to the Nashville hospital was via helicopter ambulance. Wieberg said she had heard such flights could be pricey, but she didn’t realize how extraordinary the charge would be — or how her mother’s skimping on Medicare coverage could leave the family on the hook.
Then the bill came.
The Patient: Debra Prichard, who had Medicare Part A insurance before she died.
Medical Service: An air-ambulance flight to Vanderbilt University Medical Center.
Service Provider: Med-Trans Corp., a medical transportation service that is part of Global Medical Response, an industry giant backed by private equity investors. The larger company operates in all 50 states and says it has a total of 498 helicopters and airplanes.
Total Bill: $81,739.40, none of which was covered by insurance.
What Gives: Sky-high bills from air-ambulance providers have sparked complaints and federal action in recent years.
For patients with private insurance coverage, the No Surprises Act, which went into effect in 2022, bars air-ambulance companies from billing people more than they would pay if the service were considered “in-network” with their health insurers. For patients with public coverage, such as Medicare or Medicaid, the government sets payment rates at much lower levels than the companies charge.
But Prichard had opted out of the portion of Medicare that covers ambulance services.
That meant when the bill arrived less than two weeks after her death, her estate was expected to pay the full air-ambulance fee of nearly $82,000. The main assets are 12 acres of land and her home in Decherd, Tennessee, where she lived for 48 years and raised two children. The bill for a single helicopter ride could eat up roughly a third of the estate’s value, said Wieberg, who is executor.
The family’s predicament stems from the complicated nature of Medicare coverage.
Prichard was enrolled only in Medicare Part A, which is free to most Americans 65 or older. That section of the federal insurance program covers inpatient care, and it paid most of her hospital bills, her daughter said.
But Prichard declined other Medicare coverage, including Part B, which handles such things as doctor visits, outpatient treatment, and ambulance rides. Her daughter suspects she skipped that coverage to avoid the premiums most recipients pay, which currently are about $175 a month.
Loren Adler, a health economist for the Brookings Institution who studies ambulance bills, estimated the maximum charge that Medicare would have allowed for Prichard’s flight would have been less than $10,000 if she’d signed up for Part B. The patient’s share of that would have been less than $2,000. Her estate might have owed nothing if she’d also purchased supplemental “Medigap” coverage, as many Medicare members do to cover things like coinsurance, he said.
Nicole Michel, a spokesperson for Global Medical Response, the ambulance provider, agreed with Adler’s estimate that Medicare would have limited the charge for the flight to less than $10,000. But she said the federal program’s payment rates don’t cover the cost of providing air-ambulance services.
“Our patient advocacy team is actively engaged with Ms. Wieberg’s attorney to determine if there was any other applicable medical coverage on the date of service that we could bill to,” Michel wrote in an email to KFF Health News. “If not, we are fully committed to working with Ms. Wieberg, as we do with all our patients, to find an equitable solution.”
The Resolution: In mid-February, Wieberg said the company had not offered to reduce the bill.
Wieberg said she and the attorney handling her mother’s estate both contacted the company, seeking a reduction in the bill. She said she also contacted Medicare officials, filled out a form on the No Surprises Act website, and filed a complaint with Tennessee regulators who oversee ambulance services. She said she was notified Feb. 12 that the company filed a legal claim against the estate for the entire amount.
Wieberg said other health care providers, including ground ambulance services and the Vanderbilt hospital, wound up waiving several thousand dollars in unpaid fees for services they provided to Prichard that are normally covered by Medicare Part B.
But as it stands, Prichard’s estate owes about $81,740 to the air-ambulance company.
More from Bill of the Month
- The Colonoscopies Were Free. But the ‘Surgical Trays’ Came With $600 Price Tags. Jan 25, 2024
- When a Quick Telehealth Visit Yields Multiple Surprises Beyond a Big Bill Dec 19, 2023
- Out for Blood? For Routine Lab Work, the Hospital Billed Her $2,400 Nov 21, 2023
The Takeaway: People who are eligible for Medicare are encouraged to sign up for Part B, unless they have private health insurance through an employer or spouse.
“If someone with Medicare finds that they are having difficulty paying the Medicare Part B premiums, there are resources available to help compare Medicare coverage choices and learn about options to help pay for Medicare costs,” Meena Seshamani, director of the federal Center for Medicare, said in an email to KFF Health News.
She noted that every state offers free counseling to help people navigate Medicare.
In Tennessee, that counseling is offered by the State Health Insurance Assistance Program. Its director, Lori Galbreath, told KFF Health News she wishes more seniors would discuss their health coverage options with trained counselors like hers.
“Every Medicare recipient’s experience is different,” she said. “We can look at their different situations and give them an unbiased view of what their next best steps could be.”
Counselors advise that many people with modest incomes enroll in a Medicare Savings Program, which can cover their Part B premiums. In 2023, Tennessee residents could qualify for such assistance if they made less than $1,660 monthly as a single person or $2,239 as a married couple. Many people also could obtain help with other out-of-pocket expenses, such as copays for medical services.
Wieberg, who lives in Missouri, has been preparing the family home for sale.
She said the struggle over her mother’s air-ambulance bill makes her wonder why Medicare is split into pieces, with free coverage for inpatient care under Part A, but premiums for coverage of other crucial services under Part B.
“Anybody past the age of 70 is likely going to need both,” she said. “And so why make it a decision of what you can afford or not afford, or what you think you’re going to use or not use?”
Bill of the Month is a crowdsourced investigation by KFF Health News and NPR that dissects and explains medical bills. Do you have an interesting medical bill you want to share with us? Tell us about it!
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: